Escherichia coli
(syn.:
Bacterium coli commune, Escherichia coli
) is a gram-negative rod of the family Enterobacteriaceae, genus Escherichia. First isolated and described in 1885 by T. Escherich. According to the taxonomy of the Society of American Bacteriologists (Soc. Amer. Bact, committee, 1920) it belongs to the genus Escherichia Castellani and Chalmers, which includes 22 species.
The Subcommittee on Enterobacteriaceae Subcommittee, 1962 classified E. coli into the group Escherichia - Shigella, which, according to the classification of Ewing and Kauffmann, is represented by the tribe of the same name, which includes two genera - Escherichia and Shigella. The genus Escherichia according to this classification and the classification of Bergey's Manuel of Determinative Bacteriology includes only one species - E. coli. The latter, according to its antigenic structure, is divided into O- and OK-serogroups and into various biotypes: serological, enzymatic, phagotypes, colicino- and colicinogenotypes.
Some of the biotypes of Escherichia coli (the so-called common strains) are commensals of the intestinal tract of humans and animals, while others are parasites that cause diseases.
Many common strains of Escherichia coli have antagonistic properties, preventing the development of pathogenic enterobacteria, yeast-like fungi and other microbes in the intestine. Some strains of Escherichia coli synthesize vitamin B12 and other growth factors, covering to a certain extent the needs of the host body. Long-term use of broad-spectrum antibiotics leads to the death of K. and the development of dysbacteriosis (see).
E. coli, as a permanent inhabitant of the intestinal tract (see Intestines, microflora), is excreted with feces into the environment (soil, water bodies), where it does not reproduce, but retains its viability for approximately the same period as pathogenic enterobacteria (Shigella, Salmonella). Therefore, it is a sanitary indicator microorganism. The detection of K. in the test samples indicates their fecal contamination (see Coli-index, coli-titer), in which, along with K., pathogens of intestinal infections may occur.
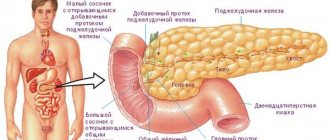
Certain biotypes of K. can be causative agents of acute intestinal infections and other human diseases (see Coli-infection). They are classified as enteropathogenic K. p. (syn. enteropathogenic Escherichia). K. items that produce enterotoxin are called enterotoxigenic. These bacteria are differentiated by O- and OK-antigens, which allows them to be classified into certain serogroups and serotypes. The etiological role of E. coli serogroups 026, 055, 086, 0111, 0126 and others in colienteritis of young children has been established; serogroups 025, 028 a, c, 032, 0124, 0144, etc. for dysentery-like diseases in adults and children; serogroups 01, 06, 015, 078, 0112 a, b, 0148 for cholera-like diseases in humans. For urinary tract infections, E. coli serogroups 02, 06, 09, 018, etc. are found, for appendicitis - 01, 02, 08, 015, etc., for cholecystitis - 01, 08, 011. For colibacillosis in animals, isolated from calves E. coli serogroups 08, 09, 078, 0115, etc., from piglets - 08, 0138, 0141, 0149, etc. Sometimes K. causes colisepsis, peritonitis, endotoxic (septic) shock (see Autointoxication), food toxic infections.
Escherichia coli is used as a universal model in general and molecular genetics. The study of a huge number of diverse mutants of one of the standard strains of K. p. - E. coli K-12 made it possible to compile a gene map and gene catalog of the bacterial chromosome (see Bacteria).
Ecology
The reservoir of E. coli in nature is a person, the colon of which is populated by different biotypes of this microbe from the moment the child switches to a mixed diet, approximately by the end of the first year of life. The number of cells in 1 g of feces ranges from several million to 1-3 billion individuals. Throughout a person's life, there is a repeated change of biotypes of cells in the intestines. Diet, previous infections, treatment with chemotherapy, antibiotics and other factors play a certain role in this process. Under natural conditions, K. p. also lives in the intestines of domestic animals, birds, wild mammals, reptiles, fish and many invertebrates.
How can you become infected with E. coli?
Intoxication can be caused by just a few E. coli bacteria entering the stomach. The most common routes of infection:
Unpasteurized milk. Dairy products are subjected to heat treatment, not least because of E. coli. E. coli enters milk from the cow's udder or milking equipment.
Vegetables and fruits. Fresh herbs, vegetables, fruits and berries will almost inevitably be contaminated with bacteria, since raw water is used for irrigation. Bacteria usually enter soil and water from organic fertilizers and animal manure.
Other food and drinks. Any unpasteurized and poorly washed foods, be it fruit juices, homemade yogurt, or cheese, can also contain E. coli.
Raw water. You can get an intestinal infection by accidentally swallowing water while swimming in a pond, lake or even a pool with insufficient chlorination. Regular tap water is generally safe.
Other people. Carriers of the infection themselves may not notice it until the bacteria enters their body. It is especially easy for infants under one year of age to become infected, who love to suck their own fingers, various objects and toys. Pay close attention to your personal hygiene when you pick up your baby!
Animals. Most often, ungulates and ruminants are carriers of E. coli. The infection can be easily picked up in petting zoos, at animal shows or when traveling to rural areas.
It is typical that you can get E. coli in your own kitchen. For example, if, after cutting raw meat, you use the same knife to chop vegetables and herbs that will not be cooked.
Morphology
Electron diffraction pattern of an ultrathin section of an E. coli cell: 1 - nucleoid;
2 - cytoplasm; 3 - cytoplasmic membrane; 4 - cell wall. E. coli cells have the shape of rods with rounded ends, 1-2 µm long, 0.4-0.6 µm thick (Fig.).
Escherichia coli is gram-negative, the ultrastructure is similar to other gram-negative bacteria. Along with mobile ones, there are also stationary forms.
The flagella are located peritrichially. There is no dispute. There are strains with a pronounced capsule, and some strains have cilia (pili).
Symptoms of E. coli infection in adults
The incubation period of E. coli averages 2–5 days. After this, typical symptoms begin:
diarrhea, in some cases with blood;
nausea and vomiting;
It is characteristic that E. coli practically does not provoke fever or increase in temperature. If it does exist, then it is insignificant - up to 37.5 degrees. In this sense, infection with E. coli is much easier to tolerate than salmonellosis. However, the symptoms of both infections are generally the same and can easily be confused.
In healthy people infected with E. coli, all symptoms usually go away within a week. However, there is one serious complication - hemolytic-uremic syndrome. This is an acute pathological condition that affects the kidneys. It poses a danger to the elderly and children.
Enzymatic properties
Kp produces numerous saccharolytic enzymes and quickly ferments glucose and other carbohydrates, most often with acid and gas formation. Almost all biotypes of K. constantly ferment mannitol, arabinose, and maltose with the formation of acid; St. 90% of strains - lactose, sorbitol; inconsistently - sucrose, raffinose, rhamnose, xylose, dulcite, salicin; As a rule, adonite and inositol are not fermented. K. p. does not utilize ammonium citrate, sodium malonate, does not grow on a medium with potassium cyanide, does not reduce nitrates to nitrites, does not break down urea, does not liquefy gelatin, most strains form indole and do not emit H2S. K. p. gives a positive reaction with methylrot and a negative Voges-Proskauer reaction (see Voges-Proskauer reaction), does not synthesize the enzymes cytochrome oxidase and phenylalanine deaminase, inconsistently decarboxylates lysine, ornithine and dehydrolyzes arginine.
Antigens
Escherichia coli contains O-, K- and H-antigens. O (somatic) antigens in K. p., Shigella and Salmonella have similar chemical properties. structure and are associated with lipopolysaccharide (LPS) of the cell wall (see Lipopolysaccharides). Immunohim, the specificity of the O-antigen is determined by the composition of hexasaccharides in the repeating units of the terminal section of the polysaccharide chain, the other end of which is connected through 2-keto-3-deoxyoctonate (KDO) to lipid A (I). Thus, the structure of E. coli 0111:B4 LPS is presented as follows:
Designations: Col - colitosis, Gl - glucose, Gal - galactose, N-AcGl - N-acetylglucosamine, Hep - heptose, x - unidentified component.
The amount of sugars in the same terminal link, as well as the number of determinant links, varies among different Escherichia serogroups. The specificity of O-antigens K. p. is usually determined in the agglutination reaction (see) with O- or OB-agglutinating coli sera on a glass slide, less often by other methods.
K-antigens denote surface antigens that are associated with the capsule and with LPS K. p. They are divided into A-, B- and L-antigens, which differ from each other in sensitivity to high temperature and chemicals. agents. The highest resistance to heat (up to 100° for 2.5 hours), alcohol and 1 N. HCl solution has the A-antigen, the least stable is the L-antigen. In most K. items, K-antigens are acidic polysaccharides containing uronic acids. Some K antigens (K 88) contain only protein. K. items having K-antigens are not agglutinated by homologous O-coli serum. This feature is inherent in living cultures and is lost after they are boiled or autoclaved. The presence of K-antigens is also established in the adsorption reaction of agglutinins and in immunoelectrophoretic studies (see Immunoelectrophoresis).
N-flagellar, or flagellar, antigens are inherent in actively motile strains. They are associated with the flagellin protein and determine the typical immunochemical specificity of K. p. H-antigens are thermolabile. They are completely destroyed when boiled for 2.5 hours.
In K. the item is described approx. 170 O-antigens, 97 K-antigens and 50 H-antigens. Strains of K. p., equipped with cilia, contain protein ciliated antigens. They are detected in the hemagglutination reaction (see).
St. 123 O-serological groups of Escherichia are connected to each other by unilateral or bilateral antigenic bonds. More than 56 serogroups have antigenic connections with Shigella and 42 serogroups with other representatives of the Enterobacteriaceae family.
K. items are designated according to antigenic formulas: the number of the O-antigen is placed in the first place, the number of the K-antigen is placed in the second place, and the number of the H-antigen is placed in the third place. The type of K antigen is indicated in parentheses. For example, K(A), K(B) or K(L). The numbers of O-, K- and H-antigens are separated by colons. According to antigenic formulas, the studied strain belongs to a certain serol group [for example, E. coli 026:K60 (B6)] and serol type [for example, E. coli 026:K60 (B6):H2]. Differences in the receptors (factor composition) of O-antigens are indicated by small letters. alphabet. For example, serogroup 0111:K58 (B4) is divided into 0111a,b:K58(B4) and 0111a,c:K58(B4).
Plasmids
Escherichia coli may contain various plasmids (see): prophage, F (fertility factor), Col (colicinogenic factor), R (resistance factor), K88 (antigenic factor), Ent (enterotoxigenic factor), etc. Prophages can cause changes in individual signs of K. p., for example. O-antigen (see Lysogeny). F-plasmids determine sexual polarity and cause the formation of sex cilia (sex-pili). Col plasmids control the formation of colicins, which inhibit the growth of phylogenetically related bacteria. R-plasmids are responsible for K. resistance to antibiotics. Plasmid K88 controls the synthesis of the antigen of the same name and threads that determine the adhesive properties of enteropathogenic and enterotoxigenic K. items; Plasmids can be of two types. One of them determines the synthesis of thermolabile, the other - thermolabile and thermostable enterotoxin.
Pathogenicity and virulence
Escherichia coli - commensals of the large intestine - can cause purulent-inflammatory processes in organs and tissues with a sharp decrease in the body's resistance.
The virulence of K. p. is manifested in the adhesiveness of K. p., i.e., adhesion to the villi of the intestinal epithelium, reproduction in the lumen of the small and large intestine, penetration into epithelial cells and intracellular reproduction, as well as in the suppression of the phagocytic activity of macrophages and polymorphic nuclear leukocytes (see Virulence). K. p. - causative agents of colienteritis in young children and cholera-like diseases in adults - multiply on the surface of intestinal epithelial cells. K. p. - causative agents of dysentery-like diseases - penetrate into epithelial cells and multiply in them in the same way as Shigella. The manifestation of virulence of K. depends on the dose of bacteria that has penetrated the human intestine. The virulence of K. is determined in tissue cultures, experiments on laboratory animals when reproducing experimental colienteritis, pneumonia and other processes. Penetration ability is established by Sheren's keratoconjunctival test by introducing a culture of K. p. onto the conjunctiva of a guinea pig's eye. K. p. forms endotoxin associated with LPS, which is part of the O-antigen. Biol, the activity of endotoxin is expressed differently in equal serogroups of K. p. The toxic properties of endotoxin are determined by the whole LPS molecule, since one lipid or polysaccharide is low toxic. Endotoxin affects the blood coagulation system, causes the Schwartzman phenomenon (see Schwartzman phenomenon) and other phenomena, and has pyrogenic, adjuvant, protective and mitogenic properties. In small doses it stimulates, and in large doses it inhibits the phagocytic reaction.
Many serogroups of K. produce enterotoxins. They are more constantly formed by E. coli serogroups 06, 08, 015, 075, 078, 0148, etc. It is believed that some serogroups of K. p. cause cholera-like diarrhea in humans, others only in animals (piglets, calves).
K. p. produce two types of enterotoxin. The heat-stable enterotoxin is inactivated only after boiling for 30 minutes, is slowly dialyzed through cellophane, and remains active at acidic pH values and after treatment with trypsin and pronase. Molecular weight 10^3 - 10^4. Does not have antigenic properties. The heat-labile enterotoxin is inactivated after 30 minutes of heating at 60°, pH 4.0-5.0, under the action of pronase and is not dualized. Mol. The weight is not exactly established. The antigenic specificity of heat-labile enterotoxins produced by different serogroups of K. p. and cholerogens is the same. They stimulate the activity of adenyl cyclase and cause the accumulation of cyclic adenosine monophosphate (cAMP), which leads to impaired secretion and the development of acute diarrhea.
To detect enterotoxigenic K., they use their ability to cause expansion of the bandaged areas of the rabbit’s small intestine and the formation of serous-hemorrhagic exudate. Other methods are based on the ability of heat-labile enterotoxin to activate adenyl cyclase and cause the accumulation of cAMP in tissue culture (Chinese hamster ovaries, pig thyroid gland), which leads to the induction of the synthesis of various metabolites and morphological changes in cells.
Test for E. coli in urine and stool
One of the reliable methods for detecting Eschirichia is bacteriological culture. This is usually done by taking a stool sample. It detects several types of pathogenic microorganisms: staphylococci, salmonella, shigella, and atypical Escherichia coli.
Also, traces of E. coli can be found in the urine, and the patient may not feel any symptoms. But normally, a healthy person should not have E. coli in their urine.
In addition to urine and feces, E. coli can be detected in genital swabs, in an open unhealed wound, or in a lung affected by pneumonia.
Fortunately, the infection usually goes away on its own without requiring any special treatment.
Some unusual strains that cause diarrhea (called traveler's diarrhea) may require a course of antibiotics. They are prescribed in moderately severe cases when the body is not able to get rid of the pathogenic microorganism itself.
However, bloody diarrhea, fever and fever may indicate shigellosis. In this case, taking antibiotics is contraindicated, as it can provoke even stronger production of Shiga toxin and aggravate the symptoms.
During E. coli food poisoning, it is important to rest and ensure you drink plenty of fluids to replenish lost fluids.
Don't take over-the-counter anti-diarrhea medications—they slow down your digestive system and prevent the infection from being cleared from your body.
Once you feel better, stick to low-fiber foods. Don't eat fat or dairy! This may make the condition worse.
Resistance
The resistance of Escherichia coli to external factors is common for asporogenous bacteria. In the external environment (water, soil), it survives, depending on specific conditions, for several months. When heated in suspension, it dies at 55° after an hour, at 60° after 15 minutes, in 1% phenol solution after 10 minutes. ., in a solution of sublimate 1:4000 - after 2 minutes. K. has selective sensitivity to brilliant green and tetrathionic acid salts. This is the basis for the use of a number of selective media. Many strains of K. p. are highly sensitive to monomycin, kanamycin, and gentamicin.
Methods of isolation and identification. The material for isolating K. is objects of the external environment (water, soil, swabs from various objects); in case of diseases - feces, vomit, urine, duodenal contents or blood, as well as food products suspected as a source of infection. The material is inoculated on differential diagnostic media (see), followed by isolation of a pure culture of K. p. Identification of the latter is carried out by studying morphological, cultural, biochemical and antigenic characteristics. The final step is to determine the biotype of Escherichia coli, especially the serogroup and serotype.
See also Escherichia.
Bibliography:
Borisov L. B. Enteropathogenic Escherichia coli and their phages, L., 1976, bibliogr.; Kaufman F. Family of intestinal bacteria, trans. from English, M., 1959, bibliogr.; Methods of sanitary-microbiological research of environmental objects, ed. G. I. Sidorenko, M., 1978; Minkevich I. E. Bacteria of the Escherichia coli group as sanitary indicator microorganisms, L., 1949; Acute intestinal infections, ed. T. V. Peradze, p. 73, L., 1973, bibliogr.; Tabachnik A.L., Girshovich E.S. and Temper R.M. Enterotoxigenic E. coli, Zhurn, mikr., epid, i immun., No. 3, p. 31, 1977, bibliogr.; Bergey's manual of determinative bacteriology, ed. by RE Buchanan a. NE Gibbons, Baltimore, 1975, bibliogr.; Cooke EM Escherichia coli and man, Edinburgh—L., 1974; Medearis DN, Cammitta BM a. Heath EC Cell wall composition and virulence in Escherichia coli, J. exp. Med., v. 128, p. 399, 1968; Orskov I. ao Serology, chemistry and genetics of O and K antigens of Escherichia coli, Bact. Rev., v. 41, p. 667, 1977, bibliogr.
L. B. Borisov.
(Escherichia coli)
- https://www.water.ru/bz/likbez/escherichia.shtml Escherichia coli ( E.coli) – - , Enterobacteriaceae, Escherichia (). 1885 . (T.
Escherich).E.coli , , , . . E.
coli , .
E.coli, . 150 ( “”) E.coli, : (), (), () ().
�������� ������ �������� ������� �� ��������� � ������� �����������, ��� 60�� ������ �� ��������� ����� 15 �����, ��� 100�� – ���������. ������������� �������� ������� ��� ������ ������������ � � ��������� ���������� ������� ����� ������� ������������. �� ��������� ������ � ���� � ����� �������� ������� ����� ����������� ��������� �������.
������� ��������������� �������� (�����, ��������, ������, ����� ����, �������, ������� ������� � ��.) � ������������ ����������� ������ ������� �������� �������
, E.coli . -, - , , ( ).
- . E.coli , .
������������� ������ ������ 3-6 ���� (���� 4-5 ����).
, E.Coli , , .
�������� ��������� ����� ���������� ��������������� �, ��������������, �� ���� (�������� ��� �������) ����� ������� ���������� ���������.
���������� ����� ����������� � �������� �������� (������, �����), ������ �������� �������� ��������� �������� ���-���� ��������� ����������� �������� ���� ��� ��������� �������.
( E.coli 100 10 , , E.coli – 10 ).
� ���������� ������� ������������ � ����������� ���� ������� ��������, ������� � ����������� ����. � ����� ��������� ��������� � ���� ��������� ������� ���������, ������������� � ��������� � ��������� ����� ������������. ��� ������� � ������� ������ �������������� ���������� �����������, �������, ��������.
� �������� �����������, ��������� ���������, ���������� �� ������� � ����������� ��������� ������ ����������. ��������� ���� � ������� � ������ ������, ���� (15-20%) ����������� ������������� � ������� (3%) �����.
������� � �������� � ����� ������ ���� �������������, �������� ������ ����������� ��������� � ����� ������� ��������� �����.
- https://www.med2000.ru:8002/n5/n92.htm – - . .
– Echerichia coli Enterobacteriaceae Escherichie. 167 (), 56 () () .��������� ���������������������, ����������������, ����������������, ������������������� � �������������������� ��������� ������� �������� �������. ������������ �������� ������� ��������� � ���������� �����, �������� ���������������� � ������ �� 34 ����, ������� ����������� ������ – �� 92 ����, �� �������� � ��������� ������� �� 3-5 ���.
��� 60- � ������ ����� 10 ���, ��� ������ ������� ���������, 1 % �������� ���������, 1-2 % �������� ������� �������, 1 % �������� ������, 3 % �������� ������ – �� 15-30 ���.
��������� � ��������� �����������: �������, ������� ��� ��������. ������� ����� ����� ������� ������������������ ����������, ��� ��������.
: , , , EIEC – 1- 2 , 3 . .
�������� �������� ����������� ��������-��������; ���� �������� – �������, ������, ������� (����� ������������ ����, ������� � ��.).
������������ ��������������� ����� �������, �������� ���������� ����� ������������� � ����������� �����. ����� 35 % �����, ���������� � ���������� ����������� ��������, ���������� ����������. ���������������� ���������, ��-��������, ����� ����������� ��������.
�������� ������������������ ��������. ������� �������������� �����������. ����������� ����������� ����������� (�� 90 %) �������������� ����� ����� ������� ���� �����. ���������� �������������� �������� �������� ��� �����������, ������������� ������� �������������.
����������, ��������� ����, ���������� ������� ������� � ������������� ������� ����������� � �������������� ��������; ���� �������������� �������������, ���� ��������� �����������, � �������� ����� ����� 1-3 ���. � �������� �������������� ������� �������� �������� ������� �����������������.
EIEC, EIEC, EIEC, EIEC , .
����������� ���� ����� ��������� ��������, ����������� ����� ����� 1,5-2 ���, ����� �����-������� ����������, ������� ���������������� ��� ���������������� ��������, ���� ���� ������������� ������������� ��������������, ������������� �� ���� ������������� �����, ��������������� ����� ����� � �������� �� 1 ����, � �������� ����� ����������� �� ������������� �������������, ������� ��������������� ��� ���������������� ��������. � ��������� �����������, ��������� ���� � ����, ������������� ���������� ����: ����������� �������� � ������� �������� ������� � ������ ����� ����� ������ 1 ���� � ��������; ���������� �����-������� ����������, �������� ������� � ����� ��� �����������. ������������� ������ �� 9 �� 72 �, ���� 10-12
- https://spm.genebee.msu.ru/manual/ru/node16.html
Source: https://kodomo.fbb.msu.ru/~ninka/ec.html