Intestinal diseases can lead to serious complications (peritonitis, severe fecal intoxication, malignant tumors of the gastrointestinal tract). Despite the high risk of complications and unpleasant symptoms (abdominal pain, diarrhea, constipation, metabolic disorders), patients often avoid going to the doctor for fear of painful examinations and long-term treatment.
CT or MRI of the intestine is used to painlessly study the structure of tissues, neoplasms and obstructions. The choice of study depends on the indications, the patient’s condition and the prospects for further monitoring of the gastrointestinal tract.
What does a CT scan of the intestines show?
In the images obtained during a computed tomography scan, you can find:
- neoplasms: in the stomach it is a cancerous tumor, in the intestines there are benign (polyps) and malignant tumors;
- intestinal obstruction;
- changes in the vessels of the intestinal mesentery (vascular thrombosis);
- foreign bodies of the stomach and intestines;
- inflammation (Crohn's disease, etc.).
CT scan of the stomach and intestines with contrast
Two contrast methods are used to examine the gastrointestinal tract::
- use of radiocontrast agents based on iodine;
- Pneumoscanning: room air or other inert gas is used to straighten the walls of the stomach and intestines.
X-ray contrast agents can be introduced into the patient’s body in two ways:
- intravenously;
- orally.
The drug for oral administration is diluted in water and drunk before the examination. Drugs such as Omnipak or Ultravist are diluted in 0.5 liters of boiled water. You must drink the solution 3 hours before the examination. And an hour before the procedure, you need to take another 0.5 liters of pure still water.
Depending on the type of pathology the presence of which is suspected in the patient, drugs for intravenous administration may be administered:
- once in a jet immediately before the start of the procedure or during the examination after a series of native images (without contrast) has been taken;
- bolus: the drug is injected into the blood during the entire examination using a special device - an injector.
After the contrast agent is injected into the blood, the patient may feel a rush of warmth or heat in the body, or a metallic taste in the mouth. These reactions do not pose a potential danger to the patient's health, so the examination can be continued.
Alarming symptoms indicating the development of an allergic reaction to the drug are:
- swelling of the face;
- sore throat;
- nausea and vomiting;
- itchy skin, rash;
- bronchospasm;
- drop in blood pressure.
If any of the symptoms of intolerance to an iodine-containing drug appear, you must inform medical staff to receive timely medical attention.
Colon CT with contrast can be performed using a combination of intravenous and oral contrast agents. However, this combination is not always used and requires a high level of professionalism from the doctor conducting the examination, since the simultaneous use of two types of contrast can lead to overdiagnosis (detection of a non-existent pathology).
Experience in the use of CT enterography in the diagnosis of Crohn's disease
Radiologist at the X-ray computed tomography room
Patupchik Yu.N.
Small intestine imaging methods:
1. Endoscopic techniques (video capsule endoscopy, double-balloon intestinoscopy, endoscopic ultrasonography, intraoperative intestinoscopy)
2. Radiation methods (ultrasound, CT, MRI, barium passage)
3. Scintigraphy, PET/CT
CT imaging of the small intestine:
targeted study of the small intestine - CT enterography - is a non-invasive technique, is easy to perform and allows you to visualize extraintestinal structures in addition to the intestinal wall. Adequate preparation of patients and adherence to the protocol for filling the intestine with contrast medium is the key to the success of the study.
A comparison of positive and neutral oral contrasts reveals the advantage of the latter for diagnosing gastrointestinal pathology, and recent recommendations advise completely abandoning positive oral contrast in certain groups of patients.
Neutral contrast media:
- PEG: a product based on polyethylene glycol, the most famous representatives of Fortrans, Klean Prep. It is the best neutral contrast after Volumen.
- drinking water
- VOLUMEN: a suspension of barium sulfate with sorbitol in a very low concentration. FDA certified
- Recently, practically not used: methyl cellulose, water with sorbitol, lactulose, pineapple juice and milk.
Own experience of using neutral contrast media:
In our clinic, neutral oral contrast (drinking water) has been used for routine examination of abdominal organs since 2009; positive contrasts are used rarely and for certain indications (water with the addition of water-soluble contrast is used as a positive contrast, 10 ml of water-soluble contrast per 1 liter of water).
The Republican Center for Gastroenterology (RCG) was created on the basis of the 10th City Clinical Hospital to provide specialized gastroenterological care. The RCH is the clinical base of the Department of Gastroenterology and Nutrition of the State Educational Institution "BelMAPO".
The clinic has 2 gastroenterology departments and a consultative and diagnostic gastroenterology office. In this regard, there was a need to introduce new CT techniques into practice (in particular, CT enterography using Fortrans) for targeted visualization of the small intestine. During this period of time, we performed 567 CT studies of the abdominal organs in patients with suspected Crohn's disease with preliminary special preparation of the intestine (CT enterography). We, together with the staff of the department (Professor Yu.V. Gorgun), have tried various methods described in the literature for preparing the small and large intestines for CT enterography; the methods described below have found their daily use. The key to a successful study is strict and consistent adherence to all stages of bowel preparation.
Preparation for CT enterography
IF A STUDY OF ONLY THE SMALL INTESTINE IS PLANNED
- Last meal - at 14.00
- After this, you are allowed to drink clear liquids without gas (drinking water, mineral water without gas, weak tea with or without sugar, etc.)
- The patient must arrive for the study 1.5-2 hours before it starts. Bring 1.5 liters of water and 1 sachet of Fortrans with you
- If possible, 1-1.5 hours before the study, the patient receives 1 tablet or 1 Buscopan rectal suppository.
Preparation for CT enterography
IF A STUDY OF THE SMALL AND LARGE INTESTINE IS PLANNED:
- Taking Fortrans should begin no earlier than 2 hours after a “light” lunch (chicken broth, tea, juice), usually at 16-18 hours. 1 sachet of FORTRANS is dissolved in 1 liter of drinking water at room temperature (carbonated water cannot be used). If the patient's weight is less than 80 kg, then 3 sachets of Fortrans should be dissolved in 3 liters of water. If the weight is more than 80 kg, then 4 sachets in 4 liters.
- Each liter of the resulting solution (3-4 liters in total) is taken over 1-1.5 hours (4-5 hours in total), a glass every 15-20 minutes, in separate sips (to improve the taste, you can drink it with juice without pulp).
- On the day of the study:
- The patient must arrive for the study 1.5-2 hours before it starts. Have 1.5 liters of water and 1 remaining sachet of Fortrans with you.
- If possible, 1-1.5 hours before the study, the patient receives 1 tablet or 1 Buscopan rectal suppository.
Contraindications to CT enterography:
- absolute contraindications are acute decompensated intestinal obstruction and an allergy to PEG drugs
- a relative contraindication is a very serious condition of patients, when they cannot drink a contrast medium or the presence of severe nausea and vomiting
CT enterography is important in the diagnosis of various pathological changes in the small intestine:
- inflammatory/granulomatous diseases of the small intestine (UC, Crohn's disease, infectious diseases of the small intestine, connective tissue diseases)
- tumor lesions of the small intestine (lymphoma, GIST, carcinoid, small intestinal cancer, metastases)
- level and causes of small intestinal obstruction.
- clarifying the cause and localization of gastrointestinal bleeding in a hemodynamically stable patient
- celiac disease
- ischemia of the small intestine.
Crohn's disease
- Crohn's disease is a chronic idiopathic inflammatory disease that affects all layers of the intestinal wall, as well as all segments of the gastrointestinal tract (the small intestine is affected in 80% of cases; 1/3 of patients have damage to the distal ileum), often accompanied by extraintestinal manifestations. The etiology of the disease is not reliably known. .
- The disease has two age peaks: at 20-25 years and at 50-70 years
- Clinic: characterized by acute or gradual development of symptoms of the disease: abdominal pain and diarrhea, often accompanied by fever and loss of weight of the patient. The course of the disease is chronic with periodic exacerbations (active phase).
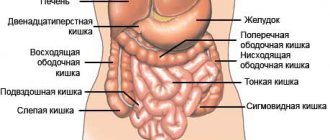
- Localization of the lesion: any part of the gastrointestinal tract can be affected throughout the entire length from the mouth to the anus
- Isolated damage to the small intestine is detected in 30% of patients (mainly the terminal part of the small intestine)
- Isolated damage to the colon is detected in 20-30% of patients
- Joint damage to both the small and large intestine is detected in 40-50% of patients.
- Extraintestinal manifestations: arthritis, cholelithiasis, eye and skin lesions, in children – developmental delay, etc.
Diagnostics:
- The diagnosis of Crohn's disease is based on a combination of clinical, laboratory, histological and imaging data. One research method is not enough to make a reliable diagnosis.
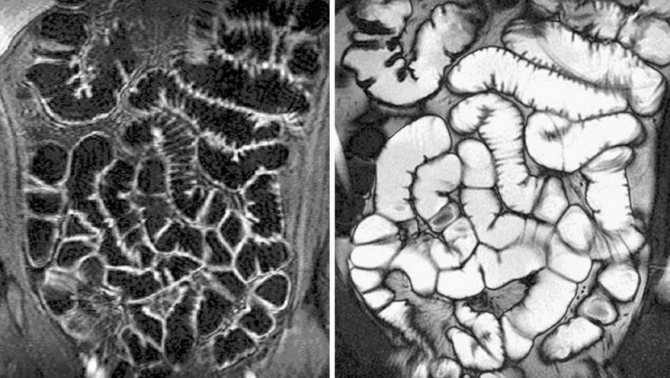
- Radiation research methods, in particular, CT enterography, can reliably detect Crohn's disease and evaluate non-intestinal manifestations/complications of this disease. At the moment, CT enterography is the “gold standard” for diagnostic imaging for suspected Crohn’s disease, as well as for monitoring treatment
- Radiation research methods:
1.help in making a primary diagnosis (due to the characteristic picture and extent of the lesion); for example, involvement of the small intestine helps differentiate CD from UC.
2.help in identifying complications of CD (CN, sinus tracts, fistulas, abscesses)
3.help differentiate acute inflammatory strictures from fibrous strictures, which may influence the choice of treatment (medical or surgical)
4.help in assessing the activity of the process and the dynamics of changes during treatment
CT signs of Crohn's disease activity:
- increased accumulation of CV in the mucous membrane: an important criterion for the activity of Crohn's disease. This sign is the most sensitive during an active process.
- thickening of the intestinal wall (thickness more than 3 mm)
- mural stratification involves visualization of individual layers of the intestinal wall that are not normally visible. The edematous intestinal wall has a 3-layer appearance with increased accumulation of CV in the outer (serous) and inner (mucosal) layers, between which there is a low-density submucosal layer. However, this sign is not specific to CD and can be detected during other inflammatory processes and even sometimes during ischemia of the intestinal wall. It should also be borne in mind that an insufficiently stretched loop of the small intestine can simulate increased accumulation of CV and wall thickening, therefore it is necessary to take into account other criteria for the activity of the process visible on CT enterography.
- emphasis of mesenteric vessels - “comb symptom” Emphasis and increase in the number of mesenteric vessels near the inflamed intestine. This sign is most sensitive during an active process
- stringy/creeping compaction of mesenteric fat (stranding/creeping fat) In the active phase, compaction of mesenteric fat is also often determined, due to the transmural spread of the inflammatory process through the seasonal membrane to the fiber of the mesentery of the small intestine, as well as due to hyperemia of the mesenteric vessels. This sign is most sensitive during an active process
- inflammatory (reversible) strictures - Presence of areas of narrowing and expansion
- CTE also plays a role in identifying reactive lymphadenopathy in the mesentery next to stenotic segments of the intestine, which is also an important criterion for the activity of the process.
CT signs of long-term Crohn's disease in the inactive phase
- Fat deposits in the submucosal layer are characteristic of a chronic inflammatory process and must be differentiated from the symptom of intestinal wall dissection during an active process.
- Also, submucosal fat can be confused with fibrosis of the submucosal layer (CT does not clearly differentiate them from each other).
- pseudosacculation (pseudo-protrusion) of the intestinal wall
- fibro-fatty proliferation of the adjacent parts of the intestinal mesentery. It is believed that fibro-fatty proliferation in the adjacent parts of the intestinal mesentery plays an important role in maintaining the inflammatory process due to the production of TNF-alpha in this area.
- fibrous (irreversible) strictures CT enterography has high sensitivity in detecting intestinal strictures - thickening of the intestinal wall with narrowing of the intestinal lumen. It is important to differentiate between inflammatory (reversible) and fibrous (irreversible) strictures, since the choice of treatment tactics (medical or surgical treatment) depends on this.
Reversible strictures that occur during the active phase of the disease are characterized by increased accumulation of CV in the mucous membrane, wall dissection, thickening of the mesenteric fat of a creeping nature, and hyperemia of the mesenteric vessels.
Irreversible strictures, with a long-term disease with the presence of transmural fibrosis of the wall, are characterized by reduced accumulation of CV in the intestinal wall and the absence of a symptom of wall dissection.
Video capsule endoscopy is contraindicated in the presence of inflammatory or fibrous strictures, in which the diameter of the intestinal lumen is less than 1 cm (there is a high risk that the capsule will get stuck in the intestinal lumen and cause CI). The likelihood of capsule getting stuck in patients with CD and the presence of small intestinal strictures is relatively high (13%). In order to avoid this complication, CTE should be performed before video capsule endoscopy.
Complications of Crohn's disease
- intestinal obstruction CT enterography is contraindicated in the presence of acute decompensated CI (in this case, the method of choice is routine CT examination of the abdominal cavity and pelvis, which makes it possible to localize the obstruction zone, identify changes in the mesentery and blood vessels, determine the presence of free fluid in the abdominal cavity, determine presence of free gas if bowel perforation is suspected). In all other cases, if the presence of CI is suspected, CT enterography is an excellent technique that allows a more reliable assessment of the location and extent of intestinal strictures.
- sinus tracts (deep ulcerative defect throughout the entire thickness of the intestinal wall)
- fistulas are tubular tracts accumulating a contrast agent that connect individual intestinal loops. They may or may not contain liquid content.
- interintestinal abscesses are an extraintestinal accumulation of liquid contents without communication with the intestinal lumen. Since the contents of the abscess may have a density and characteristics identical to the intraintestinal contents, to make a diagnosis of an abscess it is necessary to exclude the presence of communication between the intestine and the fluid collector. In such cases, viewing multiplanar reconstructions (MPR) in the coronal and sagittal planes, as well as curvilinear reconstructions (CPR), is often helpful, especially in patients with little intra-abdominal fat.
CONCLUSIONS
- CT enterography is a non-invasive technique that is of great importance in the diagnosis/differential diagnosis of various pathological processes in the small intestine (inflammatory/granulomatous diseases, tumor diseases, hidden hemorrhages in the gastrointestinal tract, CI, ischemia, etc.)
- CT enterography allows us to identify involvement in the pathological process not only of the small intestine, but also of extraintestinal structures (using CT, you can assess the condition of the mesentery, mesenteric vessels, colon, parenchymal organs, and lymph nodes).
- According to the ACR criteria, CT enterography is the method of choice for Crohn's disease (it is important for the diagnosis and differential diagnosis of the disease, assessing the activity of the pathological process, plays a role in choosing a treatment method and assessing its effectiveness, identifying complications)
- High-quality bowel preparation before the study and strict implementation of the technique (use of neutral contrast medium and PEG preparations) are the key to successful diagnosis!!!
Indications for examination
The scope of the examination depends on the presence of which pathology needs to be confirmed or excluded in the patient.
CT scanning of the stomach and intestines is rarely performed at the same time due to the fact that the large scope of the examination involves the patient receiving a large dose of radiation. To prescribe a diagnosis of the condition of the entire gastrointestinal tract, very serious indications are needed.
CT scan of the stomach is used for:
- detection of a cancerous tumor of the stomach walls;
- determining the location, size of the tumor, its spread to neighboring organs;
- identifying mucosal ulcers;
- searching for areas of bleeding.
Get a referral from your doctor for a CT scan of the small intestine:
- neoplasms (lymphomas, cancer);
- inflammation (colitis);
- mucosal ulcers;
- bleeding;
- damage to the walls of the small intestine due to celiac disease;
- foci of necrosis (death) due to thrombosis of the vessels of the intestinal mesentery.
CT scan of the large intestine is performed for the following indications:
- suspicion of the presence of polyps and other benign neoplasms;
- colon cancer;
- blood in the stool, pain in the rectum;
- preventive examination of the patient if intestinal cancer is detected in blood relatives;
- the presence of “minor signs” of cancer: alternating diarrhea with constipation, causeless weight loss, malaise, fatigue, etc.
Contraindications for examination
It is prohibited to perform a CT scan of the stomach and intestines in the following cases:
- pregnancy;
- The patient's weight exceeds 120 kg.
Carry out with caution and only if there are serious indications.:
- children under 12 years old;
- nursing women;
- patients with renal failure;
- with multiple myeloma.
Contraindications for the administration of a radiocontrast agent:
- pregnancy and lactation;
- renal and liver failure;
- diabetes;
- intolerance to iodine-containing contrast agents.
When not to conduct an examination

Contraindications for MRI and CT examinations are somewhat different. Magnetic nuclear tomography is sensitive to metal, so if there are permanent metal implants in the body, manipulation cannot be performed. Below are general contraindications for the study.
- Artificial pacemaker.
- Mental disorders that do not allow the patient to lie still.
- General serious condition, since the patient will not be able to remain face down.
- Allergy to contrast agent.
Computer enterography of the small intestine is not performed in pregnant women, as well as in people suffering from radiation sickness.
Preparing for the examination
The presence of food in the stomach, intestinal contents and gases in the intestines, active peristalsis can significantly complicate the examination and make images of organs unclear.
Before the procedure, it is recommended to carry out special preparation in order to make the examination as informative as possible.:
- From the diet for a couple of days before the examination, it is necessary to exclude any foods that provoke increased gas formation in the intestines (legumes, carbonated drinks, cabbage, etc.);
- to completely remove contents from the intestines, you must take Fortrans or another drug with a similar effect;
- A cleansing enema on the evening before the examination is carried out if indicated.
The regimen for taking Fortrans is not complicated. To prepare for a CT scan of the intestine, you will need to use 3-4 packets of the drug. The contents of one package are dissolved in one liter of water. It is necessary to start taking the drug the evening before the examination, from approximately 18.00. Every 15 minutes you need to drink 1 glass of solution.
When is an MRI of the intestine prescribed?
Magnetic resonance imaging does not require special preparation; if the rules of the study are followed, it shows the condition of the mucous membrane and surrounding tissues. Magnetic tomograph displays:
- ulcers;
- developmental anomalies;
- medium, large tumors;
- narrowing of the intestines;
- thickening of the walls;
- condition of blood vessels.
MRI does not show physiological disorders well; the method cannot be performed in case of poisoning due to active peristalsis. Noise appears due to the movements of the diaphragm.
If the patient's condition is stable, an MRI is prescribed. Indications for this are as follows:
- soreness;
- suspicion of inflammation;
- impossibility of endoscopy;
- intestinal obstruction;
- control of the performed operation;
- suspicion of cancer.
In these cases, MRI is informative; the images will help make an accurate diagnosis. Since the method is harmless, it is performed frequently to monitor treatment.
How is the examination carried out?
When heading to the clinic, it is advisable to choose clothes that are spacious enough to allow you to lie still in them for a long time. Chains, hairpins, metal fasteners of clothing and belts can leave shadows in photographs, so it is better to remove jewelry and accessories.
To conduct the examination, the patient is placed on a retractable tomograph table in a supine position. Your hands will need to be placed behind your head. The supine or side lying position can also be used.

CT colonoscopy of the intestine suggests dilation of the intestinal loops with gas. To do this, the patient, who is lying on his side, is inserted into the anus with a special thin tube through which air is supplied into the intestinal lumen using a hand bulb or compressor. The procedure itself is uncomfortable. If the pain during the introduction of gas into the intestine becomes intense, then it is necessary to tell the medical staff about it. To relieve intestinal spasms, the doctor will prescribe an antispasmodic.
An intravenous contrast agent may be administered before the examination begins or after native images are taken. If a bolus injection of the drug is planned, a special catheter is inserted into the patient’s vein, to which a thin tube from the injector is connected.
You will have to lie still for 15-30 minutes, so the patient’s body is fixed using special pillows and belts.
The prepared patient is placed into the machine along with the tomograph table. During the examination, the doctor may ask the patient to hold his breath for a few seconds in order to prevent displacement of organs during breathing and to obtain clearer and more informative images.
When the examination is completed, the doctor checks the quality of the images obtained. If all the images are clear and detailed, then the table along with the patient is pulled out of the tomograph capsule, and the patient is allowed to stand up.
Decoding the received data
During the examination, the doctor receives a series of images, which are black and white images of sections of organs in the area being examined. Deciphering means determining which areas of the images correspond to which organs and tissues, what changes there are in the structure of organs and tissues, and what types of pathology these changes are typical for. A radiologist or radiation diagnostics doctor is responsible for describing the images. Decryption can take from 30 to 60 minutes. After this, the patient receives photographs on digital media or film, as well as a doctor’s report certified by signature and seal.
You should be prepared for the fact that the doctor will not be able to recognize the formations present in the images. This is why it happens that during a CT scan it is not possible to take a biopsy of a “suspicious” area of tissue. In this regard, after performing a CT scan of the stomach and intestines, the doctor’s conclusion may include a recommendation to continue the examination using fibrogastroduodenoscopy (FGDS) or colonoscopy with a mandatory biopsy.
How often can a CT scan of the stomach and intestines be done?
CT scanners use X-rays to obtain images of tissue slices on the patient's body. The radiation dose that the patient receives during the examination directly depends on the scope of the examination. For example, the radiation dose that a patient receives during a CT scan of the stomach is much less than what can be received when performing a CT scan of the stomach and intestines. One such examination will not cause harm to the patient. But one should take into account the fact that performing several such procedures in a short time can lead to radiation sickness. In this regard, for computed tomography, restrictions have been introduced on the volume of one examination and the frequency of procedures.
The optimal frequency of CT scans is 12 months, regardless of whether the same area of the body will be examined as for the first time or a different one. If there are serious indications, a repeat procedure can be performed no earlier than 6 months after the first.
The fundamental difference between magnetic resonance imaging and computed tomography
The main difference between magnetic resonance and computed tomography is the method of obtaining images of the organs being examined. The different visualization principles cause differences in the accuracy of the methods, indications, contraindications and limitations to their use.
CT as a diagnostic method
Computed tomography is a research method that involves the use of X-rays to obtain various projections of internal organs. In standard radiography, rays pass through tissue, focusing on a special plate or film, producing a two-dimensional image. With CT, due to the multiplicity of images, the image is three-dimensional.
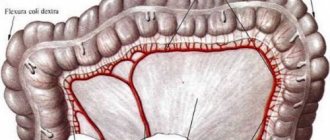
A three-dimensional model of the intestine is formed due to the specific design of the tomograph. The source of rays when performing a CT scan is a ring-shaped contour, inside of which the table is enclosed, where the patient is located. During one procedure, the device takes several hundred pictures from different points, which allows you to obtain an accurate three-dimensional model of the organ under study by combining the images in a computer program.
Based on the results of the study, the doctor can evaluate not only the overall picture of the tissue structure, but also individual sections no more than 1 mm thick. This expands the capabilities of the method and facilitates an accurate diagnosis.

Features of MRI
The magnetic resonance imaging method is based on the use of an electromagnetic field to obtain data on the condition of internal organs. The magnetic field reflects off the hydrogen ions, indicating the density of the tissue in the area being examined. The signal intensity in different areas of the intestine is recorded by the receiving sensor and transmitted to the computer.
As with CT, MRI allows you to simulate the structure of the intestine and examine the sections necessary for diagnosis.
The disadvantage of this method is the need to remain motionless for a long time (40-60 minutes). To ensure the accuracy of the result, the patient’s limbs are fixed with special straps in the MRI.
For both types of tomography, a contrast agent can be used. In the magnetic resonance method, gadolinium preparations are used as contrast, and in the radiographic (computer) method, iodine preparations are used.