Lactulose is a disaccharide consisting of residues of galactose and fructose molecules, a synthetic stereoisomer of milk sugar - lactose. Lactulose is a synthetic product. The human body does not have enzymes capable of digesting it. Lactulose passes through the gastrointestinal tract and reaches the colon unchanged, without being significantly absorbed. For bifidobacteria and lactobacilli this is an ideal environment in which they happily grow and reproduce.
The role of bifidobacteria and lactobacilli for the body is difficult to overestimate. Their metabolic products are an important source of energy for the functioning of colon cells. They also block the formation of toxic and carcinogenic products of protein metabolism. Lactulose is absolutely unsuitable for feeding and propagating E. coli, clostridia, and salmonella. In its presence, pathogenic microorganisms die and are deprived of the opportunity to poison the host’s body.
Bacterial metabolism of lactulose leads to the formation of short-chain fatty acids (acetic, lactic, propionic, butyric). Their weak acidifying effect in the intestines helps restore peristalsis, and the osmotic effect helps create volume of feces and softens them. This promotes painless bowel movements and normalizes bowel function in general.
Preparations based on lactulose (Lactusan, Prelaxan) are the most preferable: they do not have a number of disadvantages inherent in other groups of laxatives. These are mild laxatives.
Scientific studies have proven that the inclusion of lactulose in dairy products for adults helps to increase beneficial bifidobacteria and lactobacilli from 7.5 to 57%, and the amount of E. coli is reduced by 100 times.
It is very important that Lactusan is absolutely harmless during pregnancy and breastfeeding, and is safe for children. It is not addictive even with prolonged use. Lactusan contains at least 55% of dry substances, of which: lactulose - no less than 45%, galactose and fructose - no more than 10%.
Lactusan has a complex effect on the intestines due to its osmotic effect and restoration of its own microflora. It successfully treats both acute and chronic constipation. Lactusan is available in the form of syrup in bottles of 100 and 300 g and tablets of 60 pcs. packaged.
|
The dosage of Lactusan is selected individually in order to achieve two or three stools. The average dosage of Lactusan syrup for adults is 10 ml (2 teaspoons) 2 times a day, for children over 3 years old - 5 ml (1 teaspoon) once a day, for children over 1 year old - 0.5–1 teaspoon spoons 1 time per day. The tablet form of Lactusan is prescribed for adults - 4-5 tablets per day; children over 5 years old - 3 tablets per day with food. The clinical effect occurs within 2–3 days from the start of taking Lactusan. The course of treatment is 7–14 days. In case of advanced dysbacteriosis and constipation, the duration of taking Lactusan increases by 1.5–2 times. If signs of diarrhea appear (more frequent stools up to 4 times a day), the dose of Lactusan should be reduced by 2 times.
Unlike lactulose preparations, irritant laxatives can be used primarily for acute forms of constipation, but long-term use is not recommended. Often drugs are used uncontrollably, not as prescribed by a doctor, which can lead to undesirable consequences: addiction to the drug, stretching or even rupture of the intestinal wall.
Irritating laxatives (sena, senadexin, etc.) have a damaging effect on the intestinal epithelium and lead to lazy bowel syndrome, addiction, and can have a mutagenic effect. Long-term use of these drugs sharply increases the risk of developing tumors.
Osmotic laxatives (Fortrans, Forlax, etc.) help retain water in the lumen of the large intestine and prevent it from being absorbed into the blood. Bulk laxatives absorb water, swell and stretch the intestinal wall. These drugs alleviate symptoms and affect the formation of feces, but the restoration of microflora in the intestines does not occur. Therefore, they are not recommended for use in cases of chronic constipation and pregnancy.
Probiotics (lactobacterin, linex, bifidumbacterin) help normalize intestinal microflora and contain live bacteria. They are not used to relieve acute constipation; they act gradually. Treatment with these drugs is long-term: a very small percentage of live bacteria enters the large intestine, where there are conditions for their reproduction.
Normal bowel function affects our longevity and well-being. It’s so good when everything in the body works “like a clock”: accurately and on time. And all “failures” can be eliminated using effective and safe means.
Lactobacterin or Bifidumbacterin - what is the difference?
To restore intestinal microflora, the drugs Lactobacterin and Bifidumbacterin are often prescribed separately or in combination. This confuses many, because the effect of these two drugs is almost the same, and the indications for use are not too different. What is the difference between Lactobacterin and Bifidobacterin? The drugs work due to bacteria belonging to different species.
What is the difference between Lactobacterin and Bifidobacterin?
The main difference between Lactobacterin and Bifidumbacterin is that the composition of the first drug is dominated by lactobacilli, and the composition of the second is dominated by bifidobacteria. Both are inhabitants of a healthy intestine and are vital for humans.
The normal ratio of bifidobacteria to lactobacilli is 100 to 1. Therefore, doctors often prescribe Bifidumbacterin to patients, because more bifidobacteria are required for normal functioning. An imbalance in the ratio of one bacteria to another is called dysbiosis. It can also be aggravated by the action of pathogenic microflora - staphylococci, streptococci, yeast and fungi.
Here are the main signs of dysbiosis:
- constipation or diarrhea;
- bloating;
- avitaminosis;
- constant feeling of fatigue;
- lack of appetite;
- flatulence.
Lactobacilli fight pathogens by producing lactic acid, which kills foreign bacteria. Bifidobacteria multiply quickly and simply displace pathogenic microflora with their numbers, and also accelerate the exit of bacterial waste products and toxins from the body. If you don’t know what to choose – Lactobacterin or Bifidumbacterin, you can buy a complex probiotic, for example, Linex or Lactovit Forte.
There is also a little trick that allows you to make a choice: bifidobacteria have a mild laxative effect, and lactobacilli strengthen. Therefore, if you suffer from constipation, it is better to give preference to Lactobacterin; if you suffer from diarrhea, it is better to give preference to Bifidumbacterin. To the question of which is better - Bifidumbacterin or Lactobacterin, there is no correct answer. These are products of the same category (probiotics) that are used in the treatment and prevention of dysbiosis along with each other, depending on the needs of the patient.
Is it possible to take Lactobacterin and Bifidumbacterin at the same time?
If two of these drugs are prescribed simultaneously, it is necessary to take both drugs without fail. If you cancel one of them, dysbiosis will only get worse. It is advisable to drink Lactobacterin and Bifidumbacterin at different times of the day, for example, one in the morning, the other in the evening. This will allow one type of bacteria to settle in the intestines before another type of bacteria enters.
There are several more secrets to using these medications:
- It is better to drink Lactobacterin earlier than Bifidumbacterin, since the intestines need slightly less bacteria of this type.
- Bifidobacteria go well with plant foods and dairy products; lactobacilli are best drunk with plain clean water.
- Lactobacillus is not recommended for people with lactose intolerance and sensitivity to dairy products.
- When buying a complex product, consult your doctor: usually such drugs are more expensive, and their need is not so high.
- It is preferable to give bifidobacteria to small children, and lactobacilli to adults.
Contraindications to both drugs are individual sensitivity and lactose intolerance. Side effects are extremely rare, usually various allergic reactions and diarrhea.
The best drugs for the intestines
Poor nutrition, stress, hormonal imbalances, inflammatory processes, and unfavorable environment often lead to digestive problems. First of all, the sensitive intestinal microflora suffers, manifesting ill health with spasms, bloating and disorder. To restore and prevent it, you need to choose the best drugs for the intestines, since the effectiveness of treatment depends on their quality. Based on user reviews and the opinions of leading doctors, experts have compiled the TOP 10 most effective drugs for the intestines.

Lactobacterin for constipation in infants
Lactobacterin for newborns has both positive and negative reviews for constipation. It's all about parents' ignorance of the rules of admission and self-medication. Not all constipation should be treated with probiotics, since in most cases of childhood constipation at this age, the cause lies not in dysbiosis, but in the gastrointestinal tract getting used to new food.

The instructions for the drug indicate the minimum age threshold for the patient to be 3 years. However, Lactobacterin is often prescribed by pediatricians, starting from the first month of life:
- up to 6 months – 1–2 capsules in 3 doses;
- from 6 months – up to three capsules;
- from one year to 3 years – 4 capsules.
When to give Lactobacterin to newborns? Constipation occurs frequently in infants. Many factors can provoke the problem, including the earlier introduction of complementary foods and the mother’s non-compliance with the diet during breastfeeding. The drug is recommended for use in cases of constipation, accompanied by colic, bloating and frequent regurgitation.
In addition, the indication is treatment with antibiotics, previous colds and viral diseases, as well as food poisoning.
We recommend that you read the article “Mixture for constipation.”
Which brand of intestinal medication is better to choose?
The review presents pharmaceutical companies with an impeccable reputation, which have been specializing in the production of drugs for many years. According to medical experts, these companies produce the best drugs for intestinal restoration that meet high quality standards.
- Sandoz (Linex) is a German pharmaceutical company represented in 140 countries. In 1993, a representative office was opened in Moscow. The Sandoz brand has become a symbol of high-quality and affordable medicines. The domestic market offers a large selection of over-the-counter pharmaceutical drugs for preventive action.
- Microgen (Lactobacterin) is a Russian manufacturer of medical immunobiological preparations and other medicines. Since 2003, the company has produced more than 250 items. All products undergo strict certification for compliance with ISO and GMP standards.
- JSC Partner (Probifor) is the largest manufacturing company from Russia. It produces on the domestic market the best drugs for the intestines, innovative probiotic substances for the manufacture of dosage forms. Developer of mass therapeutic and preventive dietary nutrition products.
- Pharmstandard (Acipol) is an influential pharmaceutical company from Russia, founded in 2003. Actively works with foreign partners, introducing innovative developments. It produces more than 250 pharmaceutical drugs, of which 120 items are included in the list of vitally important drugs.
- Vita Farma (Bifidumbacterin) is a Russian pharmaceutical company, operating since 1996. The main activity is the development, production and release of immunobiological drugs. Dosage forms for the prevention and treatment of dysbiosis. The products meet high quality standards.
- Abbott Biologicals B.V./Veropharm JSC (Duphalac) – a joint Netherlands/Russia corporation is the largest manufacturer and supplier of medicines and medical products. Priority areas are oncology, gastroenterology, women's health.
- Teva Pharmaceutical (Hilak Forte) is an Israeli pharmaceutical company, a leading leader in the production of medicines using innovative technologies. The production produces more than 1,800 types of medications every day, tailored to the needs of each patient.
- Bifilux (Normoflorin) is a group of companies, founded in 1999. He is engaged in scientific activities, the development of innovative medicines, the production and sale of products patented in the biophytocorrection program for dysbacteriosis.
- Danisco (Maxilac) is an international global brand from France. The company is developing probiotic cultures on an industrial scale. The quality criterion is the highest survival rate of bifidobacteria under various conditions.
- Enzyme LLC (Bifiliz) is a pharmaceutical company from Russia, founded in 1995. The main activity is the production, storage and sale of medicines. Priority areas: production of probiotics, immunomodulators, interferons.
Rating of drugs for the intestines
In addition to the manufacturer, the decisive criterion when choosing a medicine will be the doctor’s prescription. For preventive purposes, probiotics and prebiotics for the intestines can be purchased at the pharmacy without a prescription. The rating includes the best drugs for the intestines, which were selected according to the following characteristics:
- Release form;
- Contraindications;
- Compound;
- Purpose;
- Side effects;
- Efficiency;
- Assimilation;
- Age of application;
- Safety.
For greater coverage of characteristics, patient reviews, experience and personal observations of health workers were also taken into account. We did not ignore the availability of freely available drugs, the ratio of quality and price.
The advisability of taking Bifidumbacterin for constipation
It is worth noting that taking Bifidumbacterin for constipation will only be effective if it is caused by dysbacteriosis. When another pathology is the provoking factor, bifidobacteria are powerless.
In adult patients and in childhood, including newborns, probiotic treatment is carried out in the following cases:
- As a component of the main therapy, when the development of constipation is due to the presence of dysbacteriosis of various origins. For example, formed after prolonged use of antibiotics, due to changes in climatic conditions and water composition. A probiotic is also prescribed when diagnosing irritable bowel syndrome.
- As a supporting medicine, Bifidumbacterin for constipation in adults will be relevant when identifying impaired motility of the biliary tract, as well as colitis, gastritis and duodenitis. Constipation can be eliminated only by prescribing therapy for the underlying disease that is adequate to the condition.
Doctors emphasize that Bifidumbacterin is a drug intended for long-term use. The probiotic does not start working immediately. Its main task is to restore the disturbed balance of microflora. And only after its stabilization, the functions of the gastrointestinal tract are restored. Therefore, in case of severe constipation, it is recommended to use drugs from the group of laxatives.
In infants, the drug is prescribed to “populate” the intestinal tract with “good” bacteria. A probiotic is used in the following cases: in case of prematurity, in case of birth by cesarean section, during artificial feeding.
General indications for taking a probiotic:
- development of allergic symptoms;
- in order to prevent the development of dysbiosis;
- for constipation caused by disorders of the intestinal microflora;
- for food poisoning;
- in case of diagnosing an intestinal infection - salmonellosis, enterocolitis and others.
Lactobacilli for constipation in adults
Lactobacterin for constipation in adults helps to normalize the pH of the intestines, enhances the contraction of the walls of the digestive tract, thereby accelerating the evacuation of feces. The drug improves regular bowel movements. Lactobacilli restore mucus secretion by transforming bound bile salts into free bile salts.
Free bile acid attracts a large amount of fluid, preventing its absorption in the intestinal lumen, which softens the stool and promotes its soft transit.
Lactobacterin is prescribed for the treatment of chronic stool retention and irritable bowel symptoms.
Lactobacterin for constipation in adults helps achieve the following effects:
- during the act of defecation reduces discomfort;
- normalizes the frequency of bowel movements;
- improves peristalsis;
- ensures continuous functioning of the digestive tract.
The effect of the drug occurs after two weeks of regular use, the incidence of constipation is reduced several times.

How the drug “works”
The main active component of the probiotic is dried bifidobacteria. They help normalize the balance between “bad” and “good” microflora. In case of their obvious deficiency, the intestines begin to work abnormally, as a result of which a person may develop persistent constipation.
After taking the drug and bacteria entering the intestinal lumen, they begin to actively reproduce, which leads to the normalization of all natural processes. Restoration of digestion is observed, thanks to better processing of food, the mobility of feces improves - normal stool is restored.
In addition, Bifidumbacterin relieves the symptoms of intoxication of the body. Thanks to the normalization of the quality of the gastrointestinal microflora, all toxic components are eliminated naturally, without having time to be absorbed into the intestinal mucosa and enter the bloodstream.
Release form of the drug and recommended dosages
Bifidumbacterin can be taken by patients of all age categories. Children can be given a probiotic immediately after birth. The product is available in dry form in several formats. This:
- vaginal and rectal suppositories;
- lyophilisate in vials and glass ampoules;
- bagged powder;
- capsules with powder (Bifidumbacterin-forte);
- tablet format (Bifidumbacterin-multi).
Manufacturers also offer bottled liquid probiotic: 100 ml of milk-hydrolyzed suspension containing a culture of live bacteria.
Composition and release form
The Bioflor preparation contains live E. coli M-17 - 108 CFU, which are normal bacterial agents of the human intestine.
The product also contains extracts of vegetables, propolis and soybeans as additional components that improve intestinal function and serve as a substrate for the growth of rods. The auxiliary components of the drug are water and sodium chloride. Bioflor is a clear or whitish solution placed in 100 and 250 ml bottles and packaged in cardboard packaging.
The country of origin of the drug Bioflor is Belarus.
General rules for taking a probiotic
The dry preparation must be diluted with any liquid in accordance with the attached instructions. For infants of the first year of life, the product is given during feeding. For dissolution, it is allowed to use breast milk or formula.
For children and adults, Bifidumbacterin can be diluted with any lactic acid drinks, warm water, or mixed into liquid food. It is advisable to take the product after or during meals.
Rectal suppositories
Rectal suppositories are mainly prescribed to adult patients. Treatment is carried out according to several schemes:
- One to two suppositories three times a day in combination with a drug intended for oral administration (twice a day). Duration of therapy is 7–10 days. In some cases (on the recommendation of the attending physician), the duration of the course is increased to a full calendar month.
- To prevent dysbiosis during treatment with drugs from the antibiotic group, one suppository is used twice a day for a week.
- For intestinal infections, two suppositories are prescribed simultaneously three times a day. The duration of therapy in each specific case is determined individually.
Rectal suppositories are not used in people with hypersensitivity to actinobacteria. The drug is prescribed with caution in childhood.
Lyophilisate
This form of the drug must be dissolved in warm boiled water. For children, it can be diluted in milk or kefir. Take with meals. The dosage depends on the age of the patient:
- children over 7 years of age and the category of adult patients - 5 doses of the drug three to four times a day;
- children aged 3–7 years – 5 doses four times a day;
- children from 6 months to 3 years – 5 doses three times a day.
The duration of the course is up to four weeks. The dry contents of the bottle must be dissolved with warm boiled water. Calculation: 5 ml of liquid (teaspoon) per 1 dose of probiotic.
The solution for preparing the solution is as follows: you need to pour the required amount of water into a glass, depending on the number of doses in the bottle, ampoule or sachet. They are indicated on the packaging. Open the product and pour it into the liquid. Mix well. The powder does not dissolve immediately. This will take at least 5 minutes.
Basic rules for taking the drug in children
Before starting to use Lactobacterin, you must familiarize yourself with the following rules of administration:
- The drug is taken in liquid form.
- Lactobacterin in powder form for newborns is diluted with breast milk or formula.
- The daily dose depends on the age and body weight of the child.
- Before each use, it is necessary to prepare a fresh portion of the drug.
- After taking the medicine, the child needs to drink enough liquid.
- Treatment should last for at least two to three months.
Before using the medicine, consult your pediatrician, who will select an individual dose and number of doses per day.
Using probiotics for constipation
Possible common causes of constipation include dysbiosis or a violation of the ratio of beneficial and pathogenic microflora in the intestine in favor of predominance or simply increasing the concentration of the latter.
In addition to irregular bowel movements, the list of symptoms of dysbiosis includes:
- diarrhea;
- feeling of discomfort, bloating in the abdomen;
- intestinal colic;
- increased gas formation;
- decreased appetite;
- belching;
- nausea.

Delayed bowel movements cause abdominal pain and severe discomfort
Probiotics are used for the prevention and as part of complex treatment of constipation. They help with delayed bowel movements that occur due to previous infectious intestinal diseases, taking medications to eliminate them, and impaired digestion of food. Due to the acceleration of the regeneration processes of the mucous membrane, probiotics are effective for constipation against the background of inflammatory pathologies of the digestive tract.
Note: During normal functioning of the gastrointestinal tract, the act of defecation occurs once a day. Digestive dysfunction accompanied by the absence of stool for more than 48 hours is called constipation.
When using probiotics to eliminate difficulties with bowel movements, it should be borne in mind that they have a cumulative effect and are not able to have an immediate effect. Therefore, in case of acute stool retention, their use will not be effective. However, for the treatment of chronic disorders of the regularity of bowel movements, they will be beneficial. The recommended course of therapy is from 2 weeks to 3 months, taking into account the severity of the condition.
When is Lactobacterin prescribed for constipation?
Probiotics are recommended to be taken in certain cases of constipation. Thus, Lactobacterin for constipation in adults is prescribed for intestinal dysfunction associated with an imbalance between beneficial and pathogenic microflora, which can arise as a result of:
- taking antibiotics;
- suffered poisoning;
- chronic constipation lasting more than 4–5 days;
- infectious disease;
- pathological process in the intestine.
However, Lactobacterin can be drunk not only for the purpose of restoring intestinal flora. The drug is also recommended to be taken to prevent dysbiosis and its consequences in the form of constipation. This remedy is often prescribed for colds, ARVI, helminthiasis, allergic diseases, problems with the genitourinary system, bacterial infections of the reproductive system, etc.

Lactobacterin is indicated for both partial constipation and complete, persistent absence of stool. It is prescribed to patients as an adjuvant for unstable bowel movements caused by:
- intestinal infection;
- irritable bowel syndrome;
- colitis and enteritis;
- chronic gastrointestinal diseases;
- gastritis and stomach ulcers.
If we talk about infants, Lactobacterin is prescribed for constipation in children to improve digestion and intestinal function. Since at this age the gastrointestinal tract is still quite weak, constipation occurs frequently. This probiotic helps restore bowel movements without the use of laxatives and enemas.
We recommend that you read the article “Nutrilon mixture for constipation.”
The mechanism of action of probiotics for irregular bowel movements
To treat constipation, drugs containing Lactobacilli and Bifidobacteria for the intestines are used. Bifidobacteria participate in the synthesis of amino acids, vitamins, fatty acids, activate parietal digestion, protect against the penetration of microbes and toxins into the internal environment of the body, and prevent the proliferation of pathogenic and opportunistic microflora. Lactobacilli convert dietary carbohydrates into lactic acid, improve metabolic processes, and suppress the development of pathogenic microorganisms (staphylococci, E. coli, Proteus, Shigella).
In case of chronic absence of regular bowel movements, probiotics contribute to:
- improving digestion;
- relieving painful discomfort in the abdominal area;
- normalization of motor function of the gastrointestinal tract;
- facilitating the passage of processed food due to the production of mucous substances covering the intestinal walls by beneficial bacteria;
- restoration of the normal composition of intestinal microflora;
- reduction of fermentation processes and gas formation.
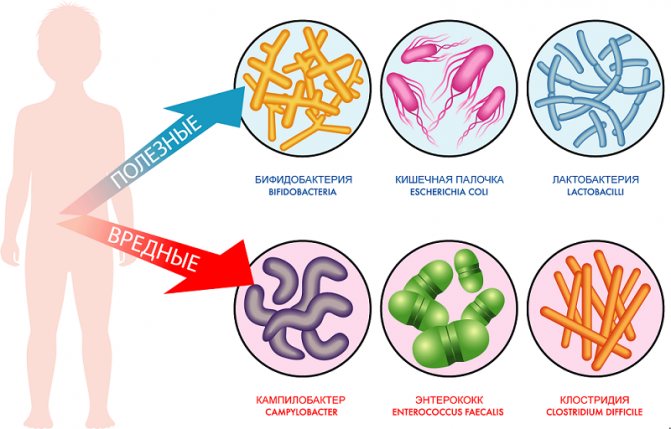
Beneficial and harmful bacteria of the intestinal microflora
The advantages of probiotics over traditionally prescribed laxatives are good tolerability, safety, absence of side effects and addictive effects.
Recommendation: To eliminate untimely bowel movements, it is important to make changes in lifestyle, normalize the drinking regime, increase physical activity, the amount of fresh vegetables, fruits, and fiber-rich foods in the diet.
Drugs that promote the proliferation of beneficial microflora for constipation
Prebiotics are among the drugs that create favorable conditions for the development and reproduction of beneficial intestinal microflora and provide a breeding ground for it. For constipation, they are often prescribed as mild laxatives.
The mechanism of their action is due to:
- improvement of gastrointestinal motility;
- softening of stagnant feces by increasing the water content in them;
- increased secretion of bile into the lumen of the small intestine;
- an increase in the volume of feces, stimulation of the urge to defecate;
- binding and removing accumulated waste and toxins;
- relief of the painful act of defecation.

If you have difficulty bowel movements, it is better to take prebiotics, since, compared to probiotics, they have a quick action. To eliminate constipation, both acute and chronic, lactulose-based drugs (Duphalac, Normaze, Lactusan) are most often prescribed. They have a mild effect, do not damage the mucous membrane of the colon, inhibit the growth of pathogenic bacteria, and stimulate the reproduction of beneficial microflora (Bifidobacteria and Lactobacilli). After taking drugs with lactulose, the laxative effect develops after 24–48 hours.
Sometimes, if you have irregular bowel movements, it is advisable to use medications that contain both pro- and prebiotics. They promote increased growth of colonies of beneficial microflora.
Taking medications for delayed and difficult bowel movements, despite the sensitivity of the problem, should be agreed with a doctor. It must be remembered that self-medication can aggravate the situation and provoke the development of complications (hemorrhoids, anal fissures, inflammation of the intestines, the appearance of pathological formations).
How probiotics make bowel movements easier
People often do not realize that the cause of rapid fatigue, relapses of bacterial and viral infections, and various vitamin deficiencies is constipation, provoked by the death of the intestinal biocenosis. These pathological conditions must be eliminated as quickly as possible, otherwise health problems will only accumulate and worsen. Probiotics can help relieve constipation in adults and children from difficulties with bowel movements.
These preparations contain dried cultures of living beneficial microorganisms that are in anaerobic “hibernation”. Bacterial strains exhibit their therapeutic activity in the liquid biological environment of the human body. After penetrating the stomach, beneficial fungi and bacteria enter the intestines, where the most favorable conditions for their growth and reproduction are present.
This is interesting: In the course of their life, microorganisms break down polysaccharides, inulins, and fiber into products that create an environment with acidic pH values.
A course of probiotics has a complex positive effect:
- restoration of optimal intestinal microbiocenosis;
- increasing the volume of feces due to beneficial bacteria;
- elimination of excess gas formation, rotting and fermentation processes;
- increased tone of intestinal smooth muscle muscles;
- stimulation of the synthesis of folic acid and vitamin K, helping to improve blood circulation.
The use of probiotics in the treatment of constipation can be one-component, when irregular bowel movements do not cause vitamin deficiency or dysbacteriosis, but only provoke increased anxiety and worry about one’s condition. If the lack of defecation has led to the active proliferation of clostridia and the development of infection, then drugs with beneficial bacteria are prescribed by gastroenterologists in combination with other drugs:
- intestinal antiseptics;
- enterosorbents;
- antimicrobials;
- balanced complexes of vitamins and microelements.
Taking probiotics creates an acidic environment in the intestines that is harmful to staphylococci, enterococci, and E. coli. Their numbers gradually decrease to optimal values - 15% of the total mass of bacteria.











