Cholecystectomy is the first choice for treating symptomatic gallstones. But is gallbladder removal surgery dangerous? Although it is the most common elective surgery in the world, complications from surgery include serious injury and death. The most serious type of injury is damage to the vascular structures associated with biliary tract injuries—complex injuries to the bile ducts that carry bile.
Like any other operation, removing the gallbladder exposes a person to the risk of developing various infections, phlebitis and thrombosis, which put his life at risk. Other complications include significant bleeding, pneumonia, heart attack, or stroke. During surgery, damage to the bile ducts or another organ may occur. Sometimes subsequent intestinal upset occurs. It is precisely because of health risks that the choice of clinic plays an important role. Today, every person has the right to this, although one can often encounter refusal due to the large number of patients. When choosing a place for surgery, you should take into account the fact how long you will have to stay in the hospital. In addition, during the first consultation at the clinic, it is necessary to discuss the question of whether the planned operation to remove the gallbladder is paid or not. Despite the efforts of the Ministry of Health to standardize the timing, the period of hospitalization still varies. This depends not only on the operation, but also on the approach of the particular hospital.
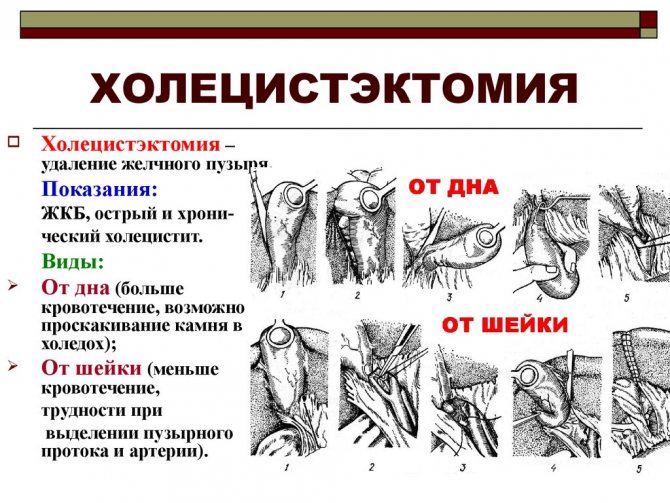
When is cholecystectomy surgery prescribed?
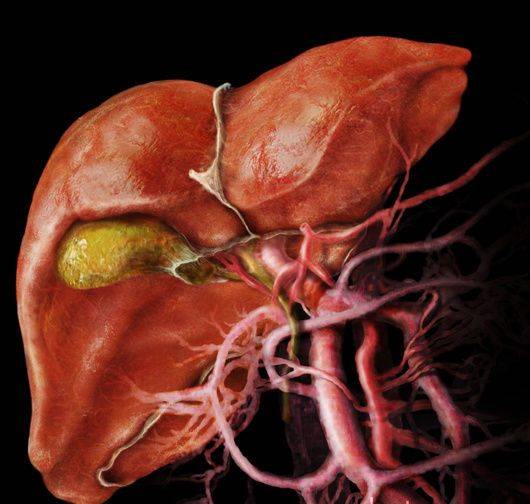
The main task of an organ such as the gallbladder is the accumulation and subsequent distribution of bile produced by the liver.
Medicine knows many diseases associated with this internal organ. For some pathologies, conservative treatment methods are successfully used (drug therapy in combination with traditional medicine and a special diet), but there are also diseases that are simply impossible to cope with without surgical treatment.
As a rule, surgery to remove the gallbladder is necessary for patients in whom this organ is affected by chronic calculous cholecystitis or in whom stones have formed in the gallbladder, causing stagnation of bile, or if a stone or large polyp threatens to block the bile ducts. It is also necessary to carry out such an operation for cancer of the gallbladder and for some types of bile duct dyskinesia. Such diseases occur mainly in women over 35 years of age, although recently there has been an increase in the number of such pathologies in young men.
All of the above pathologies cause the gallbladder to practically cease to take part in the digestive process and become a source of danger to the internal organs surrounding it. In such cases, removing this organ that has ceased to function and cleansing the bile ducts will not cause serious harm to the body, so doubts about the need for surgical intervention for such diagnoses are absolutely groundless.
If you have any serious pathology of the gallbladder and/or biliary tract, in which your attending physician strongly advises you to agree to a cholecystectomy, there is no need to despair. Agree before your doubts lead to sad consequences for the body, and pathology does not make you even worse. Your well-being will significantly improve, you will no longer be tormented by pain, and healthy organs, even if the gallbladder is removed, will cope with the increased load.
If you do not promptly operate on the gallbladder affected by pathology (if there is a prescription from medical specialists), this can greatly affect the intensity of the disease, and also lead to the appearance of serious concomitant pathologies of other organs.
Doctors classify some diseases characteristic of this organ as precancerous, as a result of which there is a high risk of uncontrolled growth of malignant cells in the patient’s body. And remember - gallbladder cancer can be cured only at the very initial, first stage of this malignant pathology.
Almost always, cholecystectomy is not a whim of a medical professional, but an urgent need or the only hope for recovery.
Indications and contraindications
At first, cholecystectomy was only indicated for patients with extremely serious problems. Gradually, the indication expanded, and today this operation can be used in more than 90% of patients with gallstones.
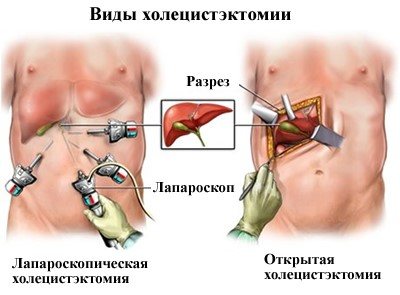
Today there are 2 types of cholecystectomy:
Traditional operation
- traditional operation;
- laparoscopic surgery.
If it is not possible to safely complete cholecystectomy laparoscopically, it is recommended that the operation be converted to traditional surgery. The need to convert laparotomy to classical surgery is reported in approximately 5% of cases. We can talk about a necessary transformation, when the complication that has arisen cannot be quickly and safely resolved using laparoscopy (severe bleeding, etc.), or a rational one, when the surgeon rejects the laparoscopic method started due to difficulties or doubts regarding the safe completion of the operation within the established time limit (unfavorable anatomical variants, progression of the pathological process).
Currently, gallbladder carcinoma and portal hypertension are considered absolute contraindications for laparoscopic cholecystectomy. Relative contraindications take into account previous epigastric surgeries. It is dangerous to use this method in a patient whose sonography shows signs of fibrosis in the d.cysticus and lig. hepatoduodenal.
How to detect this pathology in time?
Many people are interested in the question of how to promptly detect a disease of this organ and what external signs serve as a signal that they should seek medical help.
Characteristic symptoms indicating gallbladder pathology (in both male and female patients), which may persist after its removal, are:
- pain syndrome of varying intensity and nature, manifesting itself in the area of the right hypochondrium;
- in case of acute intoxication caused by a disease of this organ, an increase in temperature and chills may occur;
- various dyspeptic disorders (problems with stool and change in its color to yellow-green or black, nausea, vomiting, bloating, flatulence (after removal of the gallbladder is also possible));
- a feeling of bitterness in the mouth;
- constant air belching (after removal of the gallbladder, it may bother the patient for some time).
If you have such signs of pathology, consult a doctor as soon as possible. The sooner a diagnosis is made and proper treatment begins, the greater the chance that the disease can be cured without any special consequences.
Read also: How do liver stones form without a gallbladder?

Cholecystectomy is prescribed in the following cases:
- high risk of blocking the bile ducts with stones;
- chronic course of the inflammatory process in the tissues of this organ, causing serious discomfort in the patient;
- chronic calculous cholecystitis, the treatment of which is impossible with medications.
Complications and risks
With traditional surgery, intraoperative injuries of the bile ducts in the postoperative period mean a deterioration in the quality of life (45% of cases), subsequent stenosis of the biliary tract, narrowing formed by biliodigestive anastomosis with relapses of cholangitis. Repeated acute cholangitis can lead to destruction of the liver parenchyma and, as a consequence, to severe biliary cirrhosis with the need for liver transplantation. The risks of intraoperative bile duct injuries for patients are represented by the following factors:
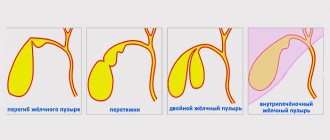
- dangerous anatomy - an unexpected anatomical variant of the biliary tree or an abnormal vascular network;
- dangerous pathology - the presence of a chronic or acute inflammatory process during surgery, as well as portal hypertension;
- dangerous surgeon - there is a risk associated with the inexperience of the surgeon, poor or unprofessional surgical technique, incorrect surgical approach and overestimation of surgical parameters.
Methods for carrying out such surgical intervention
This operation is performed in two ways - using traditional abdominal surgery and laparoscopically. Almost all planned operations of this kind are performed using the laparoscopic method (if the patient has no contraindications to such intervention).
For example, menstruation during gallbladder surgery is a contraindication, since during this period the level of hemoglobin in women’s blood increases and blood clotting worsens. In addition, the risk of postoperative complications also increases. Pathologies of the cardiovascular and respiratory systems may also be contraindications to laparoscopy.
Laparoscopy is the most optimal and least traumatic method of surgical intervention for the patient, since during such an operation the gallbladder is removed through a small (compared to abdominal surgery) incision. The laparoscopic method of removing this organ during planned operations is currently given the greatest preference, since the complications of laparoscopy of this organ are minimal.
If a laparoscopic operation is successfully performed, as a rule, the rehabilitation period is significantly reduced and the patient’s ability to work is fully restored much earlier than after removal in the traditional way. When removing the gallbladder in this way, titanium clips are a type of clamp and replace a surgical thread, which allows you to reliably block the cystic duct and cystic artery, which supplied this organ with blood. Therefore, the risk of internal bleeding or leakage of bile into the abdominal cavity is minimal. Sutures placed on the wound after laparoscopy of the gallbladder practically do not cause pain and dissolve on their own.
Since laparoscopy of the gallbladder minimizes complications after surgery, in most cases, after laparoscopy of the gallbladder, the operated patient is discharged from the hospital on the third or fourth day. After cholecystectomy with abdominal intervention, the period of inpatient postoperative treatment ranges from a week to ten days.
Why is the gallbladder removed and how to move on?
The etiology of the disease is completely unknown. Over the past 10 years, patients with cholelithiasis have almost doubled. Scientists have only been able to establish some factors leading to the disease.
According to many statistics, females are much more likely to experience stone formation disease. Men suffer almost 3–5 times less from this disease.
Excess weight is a significant factor in the formation of stones. The majority of patients tend to be overweight and have excess body weight. Age affects the appearance of stones no less. Among people over 70 years old, almost every third person has gallstones.
Causes
What are the most common causes of gallstones?
- Anatomical features of the structure of the body.
- Biochemical changes in the composition of bile, as a result of which the amount of cholesterol increases.
- Impaired motor function of the gallbladder. Which makes it difficult for the further movement of bile.
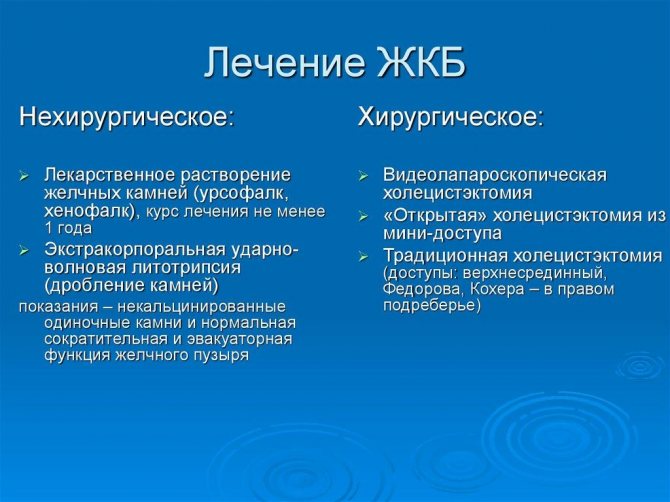
After collecting hardware data and laboratory tests, doctors prescribe treatment. Depending on certain factors of the disease, treatment may be therapeutic or surgical. With the therapeutic method, you need to take medications. Surgical treatment requires one thing - removal of the gallbladder.
Indications for cholecystectomy
There are few clear parameters leading to the operation. In the world of medicine, the question of whether surgery is necessary is often controversial.
We can only highlight some indications for which surgery is necessary:
Severe complications after acute cholecystitis, peritonitis, perforation of the gallbladder, etc. also lead to surgical intervention. Each organism is individual, so there are individual factors that do not fall under the main causes, but require urgent surgery.
Surgical intervention can be of two types:
- Standard procedure.
- Application of laparoscopic technique.
Laparoscopic method
The main indication is chronic calculous cholecystitis. It is important to know that the size and number of stones do not have much influence on the choice of method of operation.
Main indications for the laparoscopic method:
- Chronic calculous cholecystitis.
- Acute cholecystitis.
- Chronic acalculous cholecystitis.
- Gallbladder polyps.
- Minimal scarring on the right side.
- In some cases, there are no visible incisions on the abdominal wall.
- The patient's recovery period is much faster.
- Rapid restoration of intestinal passage.
- Unpleasant consequences occur less often after surgery.
- The operation is considered difficult to perform.
- Therefore, it requires professional skills in execution.
- Not every hospital can afford to perform such operations.
Complications
Symptoms of “postcholecystectomy syndrome”
After a certain period, after removal of the gallbladder, attacks of hepatic colic, pain in the side, and obstructive jaundice may begin.
Treatment of the complication can be conservative or surgical. The first option is aimed at treating diseases that were the cause of cholecystectomy. If this does not cure the consequences after surgery, then surgery is indicated.
Nuances of the postoperative period
How does the body work after gallbladder removal? There are a number of features that every patient who is prescribed such an operation needs to know about:
- since after removal of the gallbladder, bile has nowhere else to accumulate until the moment of eating, it is constantly present in the intestine, causing irritation of its walls, which can cause disruption of intestinal motility;
- if food and medication recommendations are not followed, concomitant diseases of various types may appear (for example, gastritis, colitis, enteritis and esophagitis);
- According to reviews of patients who had their gallbladder removed, many of them, for some period of time after cholecystectomy, experienced symptoms of the disease that led to the removal of this organ (in medicine they are called “residual”).
Residual sensations after gallbladder removal:
- a feeling of bitterness in the mouth;
- belching air;
- heartburn;
- slight but noticeable discomfort in the right hypochondrium;
- nausea that occurs after eating fatty foods.
These problems after removal of the gallbladder, as a rule, are more psychological than pathological in nature, and have nothing to do with the actual condition of the patient. Such false manifestations of diseases of an organ that no longer exists in the body disappear a month or a couple of months after the operation.

Postoperative period
Reviews
Four years ago, after an examination, my husband was found to have stones in his bile ducts. It was decided to perform abdominal surgery. At first, his temperature was around 40 degrees. However, gradually it began to subside and his health returned to normal. Now he feels good and can afford everything he likes to eat.
Sveta
Two weeks ago I had my gallbladder removed. Despite my fears, everything went well for me. The doctor turned out to be a great professional. For now I'm sitting at home. I eat according to diet number 5. I assess my condition as stable, although at times I experience weakness and attacks of nausea . However, most likely the reason for this is the products. You just need to strictly follow your doctor’s recommendations and pay attention to how your body reacts to a particular food.
Irina
About 8 months ago I underwent surgery in Moscow to remove my gallbladder. I went to an experienced surgeon Vadim Vladimirovich Danich. He had to solve a very difficult problem - not only did my gallbladder burst in the peritoneum, but on top of that, by the time the operation began, gangrenous peritonitis had developed. But, fortunately, everything ended well. I am very glad that I came across such attentive, qualified medical staff.
Lyudmila
Consequences and possible complications after gallbladder removal
It is necessary to understand that the gallbladder is only a reservoir for bile, and its absence will in no way affect its chemical composition. Bile is produced by the liver, which remains in place. The operation is intended only to rid the body of the source of pathology. So what happens after gallbladder removal and how does the body work without a gallbladder?
In a number of operated patients, as a consequence of removal of the gallbladder, the development of so-called biliary insufficiency began (the liver and gallbladder are the biliary system). With such insufficiency, the process of bile circulation through the gastrointestinal tract may be disrupted.
In most cases, with biliary insufficiency, the volume of bile produced by the liver increases, and it begins to exert its splitting effect not only on the food a person takes, but also on the mucous membrane of the stomach and organs of the digestive system. If this process is not stopped in a timely manner with the help of special medications, then excess bile can cause serious harm to the body, because if the mucous membrane “felt” the impact of an aggressive environment, then the organ seeks to get rid of it.
Read also: How are polyps in the gallbladder treated in a child?
Diabetes mellitus after removal of the gallbladder proceeds the same way, and the operation has practically no effect on the course of this disease. Cholecystectomy for diabetes mellitus only imposes additional requirements for compliance with a therapeutic diet, but it itself is not capable of triggering the occurrence of this disease. But the opposite situation, in which this disease can cause stone formation and thereby bring the patient to the operating table, is quite possible.
There is an assumption that the compensatory dilation of the bile ducts after removal of the gallbladder is a consequence of the fact that the gallbladder was excised. However, most practicing surgeons do not agree with this opinion. Examinations of 105 patients were carried out, the first one before such an operation, the second one a year after it. Enlargement of the bile duct channel has been recorded in only a few people.
Similar dynamic studies of the 31st patient, conducted by another group of researchers, showed that if the diameter of the bile duct before cholecystectomy was normal, then after it it remained unchanged. Based on these data, it can be argued that if, after removal of the gallbladder, a patient is diagnosed with dilatation of the common biliary tract, then this is not a consequence of the surgical intervention, but a pathology that arose before it was performed.
In women, after removal of the gallbladder, the menstrual cycle may be disrupted, but over time (subject to all medical recommendations) it will return to normal. In addition, during menstruation, pain may occur in the operated area, which is also normal and resolves over time.
The procedure for preparing for laparoscopic cholecystectomy in a hospital
The first thing you need to do is warn your doctors about any allergies you have to any medications.
Before performing this operation, the anesthesiologist and surgeon must talk with the patient. During this conversation, specialists should tell the patient about the upcoming operation, the anesthesia used, and also inform him about the possible complications and consequences of gallbladder resection. In addition, the patient should be informed about the special regimen and diet that he will need to follow after cholecystectomy. The end of such a conversation is the patient signing consent for laparoscopic intervention and the use of general anesthesia.
It is best to begin preparing for gallbladder resection even before admission to the hospital. As a rule, it consists of following diet No. 5 and therapeutic exercises.
These measures make it possible to better prepare the body for the upcoming surgical intervention, and, therefore, the operation itself will be easier to endure.
Read also: Why is a tube (drainage) placed in the gallbladder?
It is recommended that three to four days before hospitalization you switch to eating foods that prevent flatulence. The basis of the diet should be low-fat fermented milk products, dietary meats (chicken, turkey, rabbit or veal) and lean fish. Foods that can cause fermentation (fruits, vegetables, legumes, grain products and bread) should be excluded from the diet.
Before the operation, the doctor must know everything about:
| № | Helpful information |
| 1 | the patient has allergic reactions to any medications, including anesthesia and antiseptic drugs |
| 2 | cases in which the patient has experienced blood loss or is taking medications that increase bleeding (for example, warfarin or aspirin) |
| 3 | pregnancy (current or planned) |
In the hospital, preparation for this operation is as follows:
Immediately after hospitalization, the patient is prescribed a light diet. The last dinner is at seven in the evening on the day before cholecystectomy. After this, you can no longer eat anything.
On the day of the operation, in addition to eating, you should also refrain from drinking. The absence of food in the stomach minimizes the risk of vomiting during and after the intervention.
If the patient is taking any medications, it is imperative to consult with a doctor about the possibility of taking them on the day of surgery. Since people with weak abdominal muscles or excess weight are often prescribed to wear a bandage after surgery, it is better to take care of purchasing one in advance.
The evening before the day of surgery and the morning of the day of surgery, the patient is given cleansing enemas. The evening before and the morning of the intervention, you need to bathe with special antibacterial soap and shave your stomach and pubis.
Before placing the patient in the operating room, you need to make sure that he has removed all jewelry, contact lenses, glasses, and removable dentures. Before the operation itself, medical personnel must bandage the lower limbs of the patient being operated on with elastic bandages (from the fingers to the very inguinal folds). This will avoid thromboembolic complications.

Having my gallbladder removed - what medications should I take?
If the analysis shows that the bile contains a large number of components that provoke gallstone formation, then a course of special medications that contain a lot of bile acids is necessary. These medications include: “Cholenzim”, “Liobil”, “Allohol”, “Osalmid” and “Cyclovalon”. Most of these drugs also have a good choleretic effect.
In addition to the medications listed above, patients without a gallbladder are prescribed special medications with a high content of ursodeoxycholic acid (for example, Ursosan, Enterosan, Hepatosan and Ursofalk). This acid is absolutely safe for the body, but allows you to normalize the bile composition. After removal of the gallbladder, tablets must be taken strictly according to the prescribed regimen.
For the first time after surgery, patients will have to take antibiotics that disrupt the intestinal microflora. After this, you must take medicine to restore it. Such drugs include: “Linex”, “Bifidobacterin”, “Bifidum” and so on.
Possible pain syndrome is well relieved by antispasmodic drugs, such as No-shpa, Buscopan, Duspatolin and others, available in the form of capsules and tablets.
Increased gas formation and belching are well eliminated by the drugs “Meteospasmil”, “Espumizan”, “Sab-simplex”, etc.
To stimulate the motility of the gastrointestinal tract, Motilium, Cerucal and Debridat are usually prescribed.
In addition, the list of necessary medications may include general strengthening and enzyme-containing medications (for example, Creon, Essentiale Forte, Festal) and a multivitamin complex.
And remember: if the gallbladder is removed, only the attending physician decides what medications to take. Self-medication can cause serious harm to your health!
After surgery to remove the gallbladder, all patients, regardless of gender and age, need a significant change in diet and diet. The food after such an intervention should be healthy and dietary, and you will have to constantly monitor what you eat and drink.
The consumption of fried, fatty and spicy foods, as well as sour juices, carbonated drinks and alcohol is contraindicated. If such a diet is not followed, large gallstones may appear in the bile ducts, which can lead to blockage of the bile ducts, and this is very dangerous for the body.
Read also: Where does bile go after gallbladder removal?
In order to prevent relapses of pathological processes, which result in bile stagnation and stone formation, it is necessary to follow a few simple medical recommendations, namely:
| № | Helpful information |
| 1 | During the year after surgery to remove the gallbladder, you must limit your physical activity and avoid intense sports activities. |
| 2 | Swimming and walking are recommended to maintain your physical fitness. |
| 3 | If a patient who has undergone cholecystectomy is overweight, then for several months after removal it is recommended to wear a special support bandage in order to prevent possible hernia formation |
| 4 | Physical therapy exercises under the guidance of experienced health workers are very beneficial |
| 5 | special types of massage stimulate bile flow well |

Physical therapy classes
Biliary tract injuries
Injuries to the biliary tract and blood vessels are usually associated and very serious.
We recommend reading:
Is it possible to do tubage with the gallbladder removed?
This type of injury is called complex biliary tract injury and most often occurs during laparoscopic attempts to stop large bleeding from the artery and portal vein, which, with insufficient visibility of the surgical field and the inexperience of the operating team, causes damage to the bile ducts. Patients with vascular trauma are at risk of arterial damage, and then - liver ischemia and failure of its function due to disruption of the hepatic artery, ischemia of the liver lobe with the need for resection of the affected part, the development of liver abscesses or the development of ischemic stenosis of the bile ducts.
Gallbladder injuries
Bile duct injuries are serious injuries in themselves. The prognosis for patients with such injuries depends on the extent of the injury and timely detection.
Compensation for a severe type of injury - complete transection of the bile ducts - always belongs to the hands of specialists. In any case, it is not performed by the surgeon whose actions led to the injury. The fate of the patient largely depends on timely, thorough and correct treatment.
In what cases is cholecystectomy prescribed?
Indications for cholecystectomy surgery:
- cholelithiasis (the presence of stones in the bladder cavity that cannot be removed naturally);
- choledocholithiasis (stones in the bile ducts);
- acute cholecystitis (inflammation of the walls of this organ);
- chronic calculous cholecystitis;
- pancreatitis (inflammation of the pancreas);
- other pathologies that are fraught with serious complications.
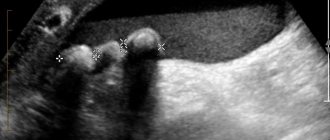
The most common reason for cholecystectomy is cholelithiasis. The essence of this pathology is the formation of stones (calculi) in the cavity of the bladder, the material for which is the so-called biliary sludge (a suspension consisting of precipitated crystals of cholesterol or bile pigment (bilirubin) with an admixture of calcium salts).
The main danger of the growth of such stones is that they are able to migrate into the bile ducts, clogging them. If the lumen of the duct is completely blocked, immediate surgery is necessary. If the stones are large or there are many of them, a planned cholecystectomy is also recommended, the purpose of which is to prevent possible serious complications.
Read also: Pros and cons of using milk thistle for the gallbladder
Cholecystectomy techniques
There are 3 approaches to removing the gallbladder, which are used with equal frequency by surgeons:
- Traditional open. It is used in cases where the organ is infected, inflamed or there are large stones in its cavity. For the intervention, a standard surgical instrument is used; an incision is made with a scalpel in the right hypochondrium (15 centimeters). Tissue and muscle are retracted, and the liver is displaced to provide access to the gallbladder. Arteries, cystic ducts, and vessels are cut out from it, only after that the organ itself is removed. A mandatory procedure is to check the common bile duct to identify stones in it. The patient is given a drainage tube, which is removed a few days after the operation. The incision in the peritoneum is sutured.
- Minimally invasive open. The technique is identical to the previous method of performing the operation, but all manipulations are performed through a mini-incision in the peritoneum (right hypochondrium area), which is less than 7 cm in length. This allows traditional intervention to minimize trauma to the anterior abdominal wall. The recovery time for patients after minimally invasive surgery is longer than after laparoscopy, but shorter than after the traditional open method of surgery.
- Laparoscopic. Laparoscopic access can be used to perform two different operations on the bladder:
- complete removal of the organ;
- removal of stones from the gallbladder.
Organ laparoscopy is an endoscopic intervention performed through 4 mini-incisions in the peritoneum. The punctures have a diameter of no more than 1 cm, so after the intervention the scars remain invisible. Carbon dioxide is supplied through the incisions using a special pump, which allows you to create free space for the operation. After introducing trocars and a laparoscope (video camera with a miniature flashlight) into the peritoneum, the surgeon sees the organ on the screen, which allows him to accurately carry out surgical manipulations. When performing laparoscopy, the cystic duct and artery are first crossed with a laser beam. Then the gallbladder is separated from the liver with a laser; similar manipulations are performed through a trocar. In Russian clinics, a laser (high-energy radiation device) and an IRE Plus laser unit are used for laparoscopy. Such equipment can reduce the percentage of postoperative complications, reduce the amount of damaged tissue and stimulate cells to recover. Removal of stones occurs due to their crushing with a laser, then their small particles are released through the bile ducts. However, if there are a lot of stones in the organ cavity, then it is not advisable to remove them, since the gallbladder is already pathologically changed. Therefore, laparoscopy is performed with complete removal of the bladder. If the goal is to get rid of small stones, then crushing them is not necessary. For this purpose, litholic therapy is used with drugs based on ursodeoxycholic acid - Ursofalk, Ursosan. After the course of treatment, the stones become small and spontaneously come out of the bladder.
Drug treatment
Despite the seriousness of surgical intervention in the body, the main role in treatment after it is given to diet. Medicines are prescribed if there are complications . To eliminate the risk of such complications occurring within three postoperative days, the patient is prescribed antibacterial therapy.
In the future, the doctor will prescribe antibiotics only if there is any inflammation of the organs. If the operated patient feels pain, he can take painkillers based on analgin for two to three days. If this does not help, you can take no more than a ten-day course of antispasmodics (drotaverine, no-spa and others).
Even though surgery completely removes the gallbladder, the liver continues to produce bile and may continue to form stones. Bile with such an unpleasant property is called lithogenic. To avoid this process, it is necessary to take special products containing ursodeoxycholic acid. Such drugs change the ratio of bile components, which reduces the likelihood of stone formation. But to achieve better effectiveness, the drug will have to be taken for quite a long time - from six months to two years.
Is surgery necessary?
The main reason for the appearance of gallstones is metabolic disorders. Failure leads to changes in the composition of bile, its stagnation and inflammation of the walls of the gallbladder. The result of pathological changes is stones. They vary in composition, shape, and size. All indicators are taken into account when choosing therapy.
Various techniques can be used to treat stones:
- Taking medications that contain bile acids is prescribed to dissolve small cholesterol stones. A positive effect is not guaranteed, but is possible after a long course of medication along with nutritional correction.
- Contact dissolution of stones - the solution is injected directly into the cavity of the gallbladder.
- Large gallstones are crushed using a shock wave or laser. But small fragments rarely leave the digestive tract on their own, so they have to be additionally dissolved with medications.
The cost of removing gallstones depends on the type of stones and type of procedure.
At the initial stage, with biliary sludge in the gallbladder, changes in eating habits and lifestyle are sufficient. In the future, diet therapy helps slow down the process of formation of gallstones, but the disease cannot be cured with diet and medications.
Even if the stones were successfully removed from the gallbladder, relapses occur in 100% of cases. Experts say that once the pathological process is started, it is impossible to stop it. In most cases, it is recommended to remove the affected organ with stones, because even an operation to dissolve the stones while preserving the gallbladder will not solve the problem - the stones will appear again and again.
How is the operation performed?
Laparoscopy of gallstones is performed under general anesthesia. The patient is under full control of the anesthesiologist. The maximum duration is 120 minutes - 2 hours, but surgeons often complete the procedure in an hour or less. The first step is to create pneumoperitoneum through marked punctures - the abdominal wall is raised to make the operated area accessible. Next comes inspection and removal.
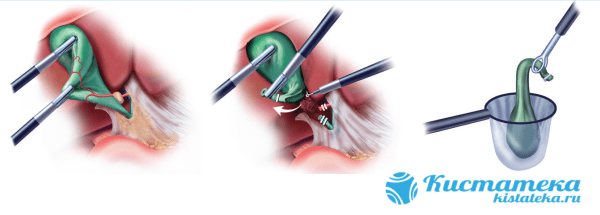
The figure shows steps 2, 3 and 4.
Technically, the procedure consists of several stages:
- The connective tissues that attach the organ to the human body dry out.
- The ducts and blood vessels are ligated to avoid spillage of bile and extensive bleeding.
- The organ is cut off from the liver.
- The bladder is removed through the umbilical foramen.
- The ducts are sutured directly from the liver to the small intestine.
Damaged vessels are soldered using an electric hook to stop bleeding. Other nuances depend on the condition of the gallbladder. So, if it is enlarged, then the stones are removed first, and only then the organ.