What type of anesthesia can be used and why
The main feature of laparoscopy when removing the gallbladder is the absence of large incisions on the surface of the skin. First, the doctor makes a small incision, 1-1.5 cm in size, through which the first trocar is inserted, and then the camera. Through it, a large amount of special gas enters the abdominal cavity, and intra-abdominal pressure increases. This is necessary for better visualization of internal organs, blood vessels and nerve plexuses. It also creates space in which the therapist can operate instruments, allowing room for range of motion. Increased intra-abdominal pressure negatively affects lung function.
Gallbladder surgery is very common these days.
Based on this, during laparoscopy of the gallbladder, only general endotracheal anesthesia can be used, with mandatory intubation of the patient and transferring him to artificial ventilation.
If the patient has bronchial asthma, and endotracheal anesthesia is strictly contraindicated for him, intravenous general anesthesia is performed, but subject to intubation.
If only intravenous anesthesia is used in the presence of bronchial asthma, then tracheal intubation is not performed. As a last resort, a laryngeal mask is used.
Indications for surgery
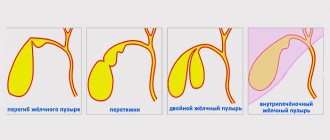
The main reason for the procedure is gallstone disease. There are two forms: painful and asymptomatic pathology. Pain signals the development of inflammation, which complicates the procedure.
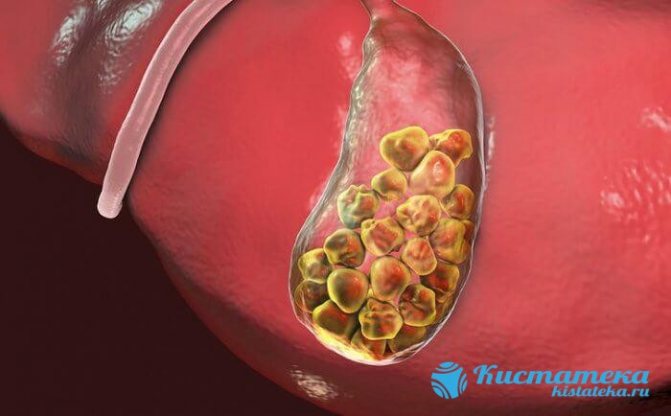
The main reason for the procedure is gallstone disease.
Other indications:
- Choledocholithiasis is a complication of the acute form of cholelithiasis, accompanied by blockage of the ducts. Drainage of the area is used during the operation;
- acute cholecystitis - develops as a result of the underlying disease. Inflammation often develops, ruptures of the mucous membrane and tissues appear, as a result of which the contents spill into the abdominal cavity;
- cholesterosis - dysfunction of the gallbladder as a result of cholesterol deposition;
- polyps are large formations, often with a vascular stalk.
The organ is completely removed in most cases, since these are severe conditions that cannot be treated conservatively.
Preparation for endotracheal anesthesia
Preoperative preparation includes a set of diagnostic tests aimed at identifying problems with the lungs. A full diagnostic complex is also carried out, as with open access surgery.

Before surgery, the patient needs to undergo examination
Examination of the patient before planned laparoscopy includes the following methods:
- General blood analysis. With it you can see:
- the presence of an infectious inflammatory process in the body: an increase in the level of leukocytes will be observed, with a shift in the leukocyte formula to the left;
- problems with blood clotting; if the platelet level is low, there is a risk of bleeding; if it is high, there is a high probability of blood clots forming during surgery;
- anemia, it will be indicated by a decrease in red blood cells, hemoglobin and color index.
- A general urine test will show the functioning of the kidneys and their excretory capacity. If there are leukocytes in the urine, this indicates an inflammatory process in the urinary system, and the presence of sediment indicates urolithiasis.
- Blood chemistry. Before removing the gallbladder, the following indicators are important: bilirubin, creatinine, urea and amylase. An increase in these indicators indicates impaired functioning of the liver, kidneys and pancreas. If these organs are insufficient, general anesthesia is contraindicated.
- A chest x-ray is needed to identify problems in the lungs.
- Electrocardiography shows the work of the heart. If the patient has atrioventricular block or atrial fibrillation, general anesthesia is contraindicated.
- Ultrasound diagnostics of the abdominal organs helps the doctor determine the scope of the operation. If there is a suspicion of a malignant neoplasm, open abdominal surgery is performed.
How should a patient prepare before surgery?
If the operation to remove the gallbladder is not performed as an emergency, but as planned, preparation should consist of the following actions:

You need to carefully prepare your body for surgery.
- The last meal should be no later than 6 pm on the day before surgery.
- You can drink water until 10 pm the same day.
- 2 days before the upcoming laparoscopy, you need to stop taking anticoagulants and warn your doctor about this.
- In the evening, on the eve of the operation, you need to do a cleansing enema and repeat it in the morning.
- All women over 45 years old have their legs tightly bandaged or compression stockings put on before surgery. For men, this procedure is performed according to indications if there are varicose veins.
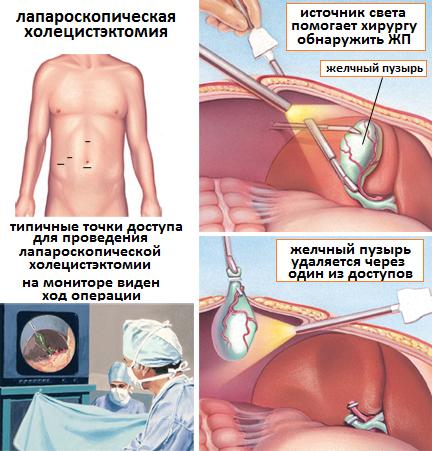
Progress of the operation
Laparoscopic cholecystectomy is considered a more popular method of gallbladder removal. The advantage of this method is that the abdominal incision is minimal. Laparoscopic surgery allows removal of the gallbladder with minimal blood loss. Recovery is quick and painless compared to classic abdominal surgery.
In some cases, the technique is not available. For example, surgery using this technique is rarely performed on elderly patients or people with a complicated course of the disease. Often, during the intervention process, the surgeon has to decide to change the technique and perform laparotomy instead of laparoscopy. The decision is made when complications in the form of adhesions and infiltrates are detected.
List of the main advantages of laparoscopic technology:
- detailed visualization of the operated area on the screen;
- absence of severe pain in the patient during the recovery period;
- minimal damage to abdominal wall tissue;
- short period of hospitalization (for young people – up to 4 days, for older people – 7-10 days);
- reducing the risk of hernia formation and the development of adhesions;
- rapid restoration of working capacity.
It is not worth declaring that this method is completely safe. As with classical laparotomy, there is a risk of infection and bleeding during the intervention. If there is insufficient competence, the surgeon can pierce the internal organs with instruments. The method does not allow the release of bile ducts blocked by stones.
Patient preparation
If the intervention is planned, it is preceded by some preparation. The patient must take laboratory tests and undergo the following instrumental examinations:
- general blood test and biochemistry;
- general urine analysis;
- chest x-ray or fluorography;
- electrocardiography or ultrasound of the heart;
- blood clotting test;
- testing for HIV, syphilis and hepatitis.
It is recommended to take all tests 1-2 weeks before surgery. If the patient is in a hospital, the clinic staff will prepare him, ensuring that he attends all the necessary procedures.

A week before surgery to remove the gallbladder, the patient must observe certain restrictions. Foods that can increase gas formation in the intestines are removed from the menu: cabbage, legumes and grains, carbonated water, kefir and other fermented milk. Your doctor may recommend taking digestive enzymes and anticoagulants. If the patient takes any medications on an ongoing basis, he should inform the doctor about this.
12 hours before surgery, the patient follows a strict diet and refuses water and food. If you are very thirsty, it is only permissible to rinse your mouth. Such restrictions are associated with the use of general anesthesia; if there is content in the stomach, the patient may vomit. The day before surgery, hair is removed from the abdomen, immediately before the intervention, the area is washed with antibacterial soap.
Surgical measures
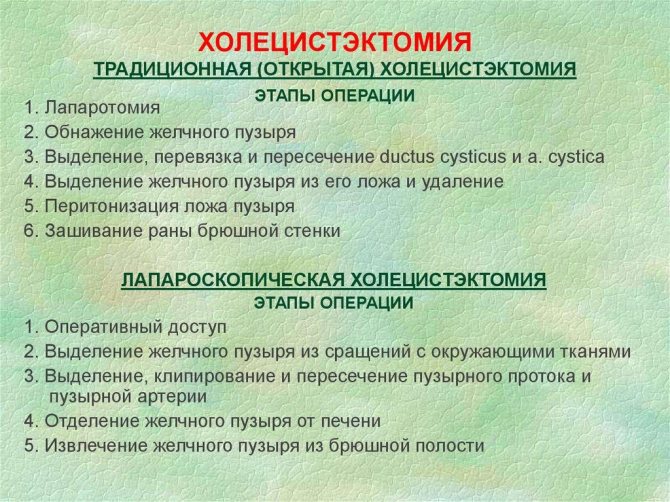
Laparoscopic cholecystectomy is performed in a sterile operating room under general anesthesia. Main stages of the event:
- A probe is placed in the stomach and a catheter is placed in the bladder. To prevent blood clots, special underwear is worn on the legs.
- Carbon dioxide is artificially pumped into the abdominal cavity to simplify the surgeon's work.
- Punctures are made at 3-4 points on the peritoneum to insert special instruments and a video scanner for control.
- The bubble is removed from the tissue, the hepatic duct is blocked and the artery is clamped with staples.
- The gallbladder is excised and removed through the incision. Damaged tissue is removed, the vessels are coagulated.
- The cavity is washed with an antiseptic.
- Remove tools from holes.
- The resulting incisions are closed by placing stitches on the outside and between the layers of skin.
The procedure is considered safe. All stages of laparoscopic cholecystectomy are monitored using a microscopic camera placed in the abdomen. Despite the high accuracy, complications sometimes occur and are quite serious. Learn more about how laparoscopic surgery to remove the gallbladder occurs in the video.
Organ removal
The affected gallbladder is removed through 3-4 incisions up to 1 cm in length. Such incisions are called punctures, which are necessary to insert the surgeon’s instruments into the abdominal cavity. After the postoperative period is completed, the incisions are covered with a scar, which is barely noticeable. The cholecystectomy itself lasts no more than one and a half hours. The operating time may increase significantly if stones are detected in the bile ducts.
What drugs are used for anesthesia
For endotracheal anesthesia, during laparoscopy of the gallbladder, the following medicinal anesthetics can be used:
- Droperidol;
- Fentanyl;
- Ftorotan;
- Nitrous oxide.
If the patient has bronchial asthma, intravenous anesthesia is used using the following drugs:
- Ketamine;
- Propofol;
- Calypsol;
- Hexinal.
Which of these medications to choose is decided directly by the anesthesiologist after reviewing the patient’s test results.
How is gallbladder surgery performed using laparoscopy?
The operation is performed by a surgical team.
The results of all manipulations inside the abdominal cavity are displayed on the monitor. How is laparoscopy of the gallbladder done:
- A needle is inserted above or below the navel to inject gas into the abdominal cavity.
- A trocar for the laparoscope is inserted and a visual examination of the internal organs is performed.
- Another 2–4 instrumental trocars are inserted - the exact number is determined for the specific situation.
- The gallbladder is disconnected from nearby organs.
- The cystic duct and its artery are isolated, clipped and divided.
- Separation of the gallbladder from the walls of the liver.
- Removal of the gallbladder - in cases of wall defects, it is placed in a plastic bag to prevent stones from entering and leakage of bile into the abdominal cavity.
- The subhepatic space is washed with saline solution.
- The wound channels are washed with an antiseptic solution.
- The muscle tissue is sutured with 1–3 stitches.
- The abdominal cavity is again filled with gas for a follow-up examination.
At the end of the manipulations, the puncture sites and seams are processed. The bandages are attached with medical glue and adhesive tape.
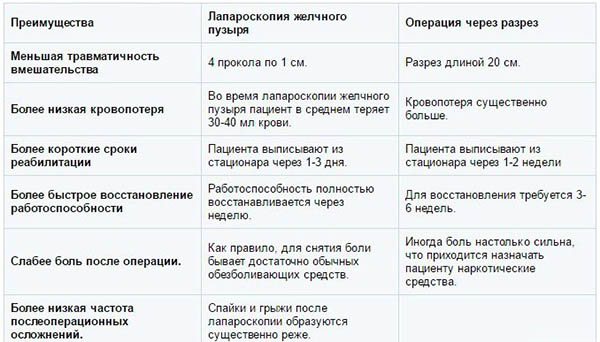
Advantages of gallbladder laparoscopy over incision surgery
Complications and consequences of general anesthesia
After laparoscopy of the gallbladder using endotracheal anesthesia, the following complications may occur:

Sometimes after anesthesia the patient feels unwell
When performing laparoscopy of the gallbladder, the anesthesiologist constantly remains in the operating room, monitoring the concentration and depth of anesthesia.
When the operating surgeon tells him that the operation is being completed, he slowly reduces the concentration of anesthetics and the patient gradually begins to wake up. The patient fully wakes up after four hours, but nausea, headache, and weakness can persist for 24-36 hours.
You should not be afraid of general anesthesia during laparoscopy of the gallbladder. With proper preparation for this surgical intervention, the negative consequences and complications are minimal. The anesthesiologist selects medications and their dosage individually for each of his patients, and tries to make the recovery process as short and painless as possible.
Diseases of an organ such as the gallbladder rank third in the world in terms of frequency of diagnosis (after diseases of the cardiovascular system and diabetes mellitus). Unfortunately, not all such pathologies can be cured with conservative methods. Quite often, doctors have to resort to surgery to remove this organ, which is called cholecystectomy.
- Surgical techniques used in gallbladder removal
- What anesthesia is used to perform laparoscopy of the gallbladder?
- Endotracheal anesthesia - preoperative preparation
- Preparing the patient for gallbladder removal
- What drugs are used for this type of anesthesia?
- Possible complications after endotracheal anesthesia
Surgical techniques used in gallbladder removal
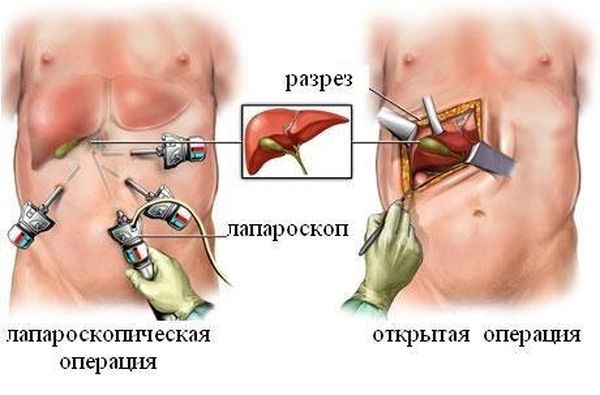
Currently, two well-established techniques are mainly used: traditional abdominal surgery and laparoscopy. Their main difference is the method of access to the organ being removed.
The traditional technique involves providing access to the operating area through a sufficiently large incision in the abdominal wall. In this case, the surgeon has direct visual contact with the organ being removed. The main disadvantages of such an intervention include:
- large size of the postoperative scar, causing aesthetic discomfort;
- quite a long rehabilitation period;
- high risk of postoperative complications.
In this regard, such operations are performed mainly in emergency cases and when, for some reason, laparoscopic surgery is contraindicated for the patient.
For planned operations in the absence of contraindications, the laparoscopy method is used.
The essence of this surgical intervention is that access to the operated organ is provided through three to four small (up to one and a half centimeters) punctures in the peritoneal wall. Through one of these punctures, a laparoscope is inserted (hence the name of the technique - laparoscopy) with a flashlight and a video camera attached to it, the image from which is displayed on the monitor and allows the surgeon to control the progress of the operation (without direct visual contact). Through the remaining punctures using special hollow tubes (trocars) special surgical instruments are introduced, with the help of which resection of the gallbladder is performed.
To ensure free access to the operating area, the abdominal cavity is pumped with gas (usually carbon dioxide) before surgery. In addition, this allows for much better visualization of internal organs, blood vessels and nerve plexuses in the area of the intervention.
Advantages of laparoscopy over conventional abdominal surgery:
- scars after such an intervention are almost invisible;
- since the impact on other internal organs is minimal, the likelihood of postoperative complications is significantly reduced;
- The recovery time for the body after such a minimally invasive intervention is much shorter than after a traditional one (often the patient is discharged from the hospital on the second or third day after gallstone laparoscopy).
It is worth saying that in the event of any unforeseen complications during laparoscopic intervention, the operation can be interrupted and continued in the traditional abdominal manner.
Modern medical science does not stand still, and currently there are already surgical techniques in which incisions in the peritoneal wall are not needed at all. This is the so-called transgastric (through the mouth) and transvaginal cholecystectomy. However, currently these methods of removing the gallbladder are at the stage of clinical testing, so we will not dwell on them in detail.
A very important point when performing not only cholecystectomy, but also any surgical intervention, is anesthesia.
Let's say right away - cholecystectomy does not imply local anesthesia, and is always performed under general anesthesia (and during laparoscopy, too).
This is due to the fact that the use of local anesthesia does not give the surgeon the necessary freedom of action, since the organs of the patient who are not immersed in sleep remain in a tense state.
What anesthesia is used to perform laparoscopy of the gallbladder?
As mentioned above, now the most common method of performing surgery to remove the gallbladder is laparoscopy. This method of surgical intervention is the least traumatic, minimizes the risk of complications after surgery and allows the patient to quickly recover after organ resection. However, the gas used for this operation significantly increases the level of intra-abdominal pressure, which negatively affects the functioning of the lungs.
In this regard, anesthesia for laparoscopy of the gallbladder is mainly used endotracheal. In this case, the patient must be intubated and connected to mechanical ventilation equipment (artificial pulmonary ventilation).
If the patient has problems with the respiratory system (for example, bronchial asthma), this is an absolute contraindication to the use of endotracheal anesthesia. In such cases, it is possible to use intravenous general anesthesia, however, even in this case, it is necessary to connect the operated patient to a ventilator.
Postoperative period
Recovery after laparoscopy of the gallbladder does not take more than 7 days. The period includes daily observation in the intensive care unit - during this time the patient wakes up from anesthesia, and complications are obvious. It is recommended not to move for at least 7 hours after surgery to allow the body to fully adapt.

Do not drink or eat for at least 6 hours.
Do not drink or eat for at least 6 hours. In the future, you can drink a teaspoon every 15 minutes. You need to get up only in the presence of medical personnel. In addition, you need to avoid intestinal upset, stop exercising and not lift anything heavier than 5 kg for 6 months.
Physical activity is prohibited for six months, sometimes up to a year. This is especially true for performing exercises that affect the abdominal muscles: this can cause the development of a hernia.
Overweight people are advised to wear a bandage at all times after laparoscopy.
Exercises
With normal recovery dynamics, the attending physician allows passive exercise 2-3 months after removal of the gallbladder. First exercise: simple walking for at least 30 minutes a day. This allows you to normalize the metabolic process and improve the flow of bile. If your health improves after walking, then a set of hygienic gymnastics is allowed.
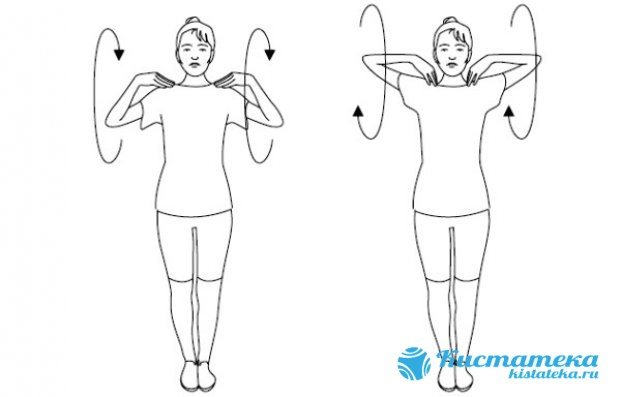
Hygienic gymnastics consists of simple exercises aimed at improving well-being. In fact, this is an ordinary exercise during which you can breathe arbitrarily. Several minutes are allotted to perform the exercises, and 5 repetitions will be enough, followed by an increase up to 10 times. The base consists of the following set of classes:
- Spread your legs shoulder-width apart, gently turn your torso in different directions. It is recommended to spread your arms, try not to move your hips and pelvis - only the torso turns. Inhale as you turn, exhale as you return to the starting position. Hands can also be placed on the belt.
Spread your legs shoulder-width apart, gently turn your torso in different directions. - Place your hands on your shoulders and rotate them one by one without removing your hands.
Rotation of the brushes. - Lie on your back, raise your legs up. Bend your knees and try to imitate riding a bicycle. Be sure to straighten your toes when stretching your leg.

Bend your knees and try to imitate riding a bicycle. - Remain lying down, put your right hand on your stomach, extend your left along your body. Slowly bend your legs one at a time, trying to reach your knee to your stomach while inhaling.
Slowly bend your legs one at a time, trying to reach your knee to your stomach while inhaling.
Exercises after removal of the gallbladder by laparoscopy are performed only after the recommendation of the attending physician.
You should not rush and increase the permissible number of approaches, as this may cause pain. The main thing is to accustom the body to stress and tone it up.
Diet
The diet after removal of the gallbladder by laparoscopy is aimed at alleviating the patient’s condition and reducing the risks of developing consequences. The liver continues to synthesize bile, but now there is no bag and it descends uncontrollably into the small intestine. Such nutrition is aimed at reducing the production of bile and debugging the digestion process.
Meals must be fractional: small portions at least 5 times a day. All food is strained through a sieve for at least two months. Eat food only warm; too hot or cold can harm the digestive system.
Prohibited foods: legumes, smoked and fried foods. Strong drinks should be avoided: alcohol, coffee and even tea. It is not recommended to consume baked goods in large quantities.
You should completely avoid eating fast food, mushrooms and fish dishes.
The diet should include fermented milk products, preferably low-fat. Be sure to include boiled and steamed vegetables in your daily diet and eat porridge. The doctor will prescribe a diet based on the individual characteristics of the patient. All you need to do is follow the instructions.
Endotracheal anesthesia - preoperative preparation
Preparation for anesthesia before laparoscopic cholecystectomy is a whole complex of instrumental and laboratory diagnostic measures, the purpose of which is to determine the current state of the respiratory system. In addition, it is mandatory to carry out in full all diagnostic measures that are carried out before traditional abdominal surgery.
The range of such events includes:
If cholecystectomy is planned, the procedure for such preparation is as follows:
- The patient should eat the last time on the day before surgery no later than 18:00;
- you should stop drinking water at 22:00 the same day;
- two days before laparoscopy of the gallbladder, you should stop taking anticoagulant drugs, which you must notify your doctor about;
- in the evening before cholecystectomy, the patient must undergo a cleansing enema, and in the morning the procedure should be repeated;
- All women over 45 years of age undergoing surgery must have their legs tightly bandaged before such an operation (compression stockings may be used). For male patients, this procedure is performed in the presence of varicose veins.
Endotracheal anesthesia during laparoscopic cholecystectomy involves the use of the following drugs:
- nitrous oxide;
- droperidol;
- fluorotane;
- fentanyl.
If endotracheal anesthesia is contraindicated for the patient, then for intravenous use use:
- hexinal;
- propofol;
- ketamine;
- calypsol.
Diseases of an organ such as the gallbladder rank third in the world in terms of frequency of diagnosis (after diseases of the cardiovascular system and diabetes mellitus). Unfortunately, not all such pathologies can be cured with conservative methods. Quite often, doctors have to resort to surgery to remove this organ, which is called cholecystectomy.
Surgical techniques used in gallbladder removal
Currently, two well-established techniques are mainly used: traditional abdominal surgery and laparoscopy. Their main difference is the method of access to the organ being removed.
The traditional technique involves providing access to the operating area through a sufficiently large incision in the abdominal wall. In this case, the surgeon has direct visual contact with the organ being removed. The main disadvantages of such an intervention include:
- large size of the postoperative scar, causing aesthetic discomfort;
- quite a long rehabilitation period;
- high risk of postoperative complications.
In this regard, such operations are performed mainly in emergency cases and when, for some reason, laparoscopic surgery is contraindicated for the patient.
For planned operations in the absence of contraindications, the laparoscopy method is used.
The essence of this surgical intervention is that access to the operated organ is provided through three to four small (up to one and a half centimeters) punctures in the peritoneal wall. Through one of these punctures, a laparoscope is inserted (hence the name of the technique - laparoscopy) with a flashlight and a video camera attached to it, the image from which is displayed on the monitor and allows the surgeon to control the progress of the operation (without direct visual contact). Through the remaining punctures using special hollow tubes (trocars) special surgical instruments are introduced, with the help of which resection of the gallbladder is performed.
To ensure free access to the operating area, the abdominal cavity is pumped with gas (usually carbon dioxide) before surgery. In addition, this allows for much better visualization of internal organs, blood vessels and nerve plexuses in the area of the intervention.
Advantages of laparoscopy over conventional abdominal surgery:
- scars after such an intervention are almost invisible;
- since the impact on other internal organs is minimal, the likelihood of postoperative complications is significantly reduced;
- The recovery time for the body after such a minimally invasive intervention is much shorter than after a traditional one (often the patient is discharged from the hospital on the second or third day after gallstone laparoscopy).
It is worth saying that in the event of any unforeseen complications during laparoscopic intervention, the operation can be interrupted and continued in the traditional abdominal manner.
Modern medical science does not stand still, and currently there are already surgical techniques in which incisions in the peritoneal wall are not needed at all. This is the so-called transgastric (through the mouth) and transvaginal cholecystectomy. However, currently these methods of removing the gallbladder are at the stage of clinical testing, so we will not dwell on them in detail.
A very important point when performing not only cholecystectomy, but also any surgical intervention, is anesthesia.
Let's say right away - cholecystectomy does not imply local anesthesia, and is always performed under general anesthesia (and during laparoscopy, too).
This is due to the fact that the use of local anesthesia does not give the surgeon the necessary freedom of action, since the organs of the patient who are not immersed in sleep remain in a tense state.
What anesthesia is used to perform laparoscopy of the gallbladder?
As mentioned above, now the most common method of performing surgery to remove the gallbladder is laparoscopy. This method of surgical intervention is the least traumatic, minimizes the risk of complications after surgery and allows the patient to quickly recover after organ resection. However, the gas used for this operation significantly increases the level of intra-abdominal pressure, which negatively affects the functioning of the lungs.
In this regard, anesthesia for laparoscopy of the gallbladder is mainly used endotracheal. In this case, the patient must be intubated and connected to mechanical ventilation equipment (artificial pulmonary ventilation).
If the patient has problems with the respiratory system (for example, bronchial asthma), this is an absolute contraindication to the use of endotracheal anesthesia. In such cases, it is possible to use intravenous general anesthesia, however, even in this case, it is necessary to connect the operated patient to a ventilator.
Is laparoscopy safer than open surgery?
Despite the obvious advantages of the laparoscopic method, it carries certain dangers, like any surgical intervention. The causes of injury or damage during laparoscopy are anatomical anomalies during adhesions, inflammatory changes, as well as carelessness in the introduction of trocars. LCE is a “jewelry” operation that requires the surgeon to have skills in working with manipulators and a good understanding of the nuances of the topographic-anatomical characteristics of the intervention area.
There are three categories of dangers of laparoscopy:
- Resulting from filling the abdominal cavity with gas:
- does not threaten the patient’s life - gas enters the preperitoneal space, under the skin;
- massive gas embolism: acute hypoxia, death - when gas penetrates into the vessels of the venous system.
- Mechanical damage:
- aorta, iliac vessels, vena cava - high probability of death;
- vessels of the anterior abdominal wall - not dangerous;
- intra-abdominal bleeding is not dangerous and is eliminated during laparoscopy.
- Thermal damage:
- impaired blood supply, coagulation of thin vessels are difficult to diagnose and difficult to reconstruct.
Attempts to stop bleeding in conditions of limited visibility cause additional injuries.
The difference between laparoscopy and open surgery Cases of bile duct injuries during laparoscopy of the gallbladder are 2-3 times more common than with open surgery - but this is 0.2-0.6% of the total. The percentage of damage to the bladder, liver, stomach, and intestines does not exceed 1.