Acute or aching pain under the left rib, accompanied by nausea, diarrhea, and constipation, should serve as an immediate signal to consult a gastroenterologist. The most common diagnosis in this case is pancreatitis. You should not delay your visit, because the disease may progress to a chronic stage. Treatment of chronic pancreatitis involves significant changes in usual lifestyle and constant monitoring.
Description
Chronic pancreatitis is an inflammatory disease of the pancreas that causes irreversible damage. The course of this disease leads to gradual disturbances of varying degrees of external and internal functions of the gland. Recent years were characterized by an increase in the proportion of patients by 1.5 times. The development of chronic pancreatitis occurs over several years, reminiscent of periods (usually seasonal) of exacerbation, followed by stages of calm.
The average age of those diagnosed is 35-45 years, but there is a trend of rapid rejuvenation in developed countries. Therefore, the discovery of pancreatitis in adults is becoming common. More often, the chronic form is formed as a result of existing gastrointestinal diagnoses: cholecystitis, gastritis, duodenitis.
This disease has various forms and is classified into the following types:
- Primary chronic (usually caused by excessive alcohol consumption) pancreatitis is divided into forms of occurrence:
- latent - painless form (pain appears much less frequently or is absent);
- jaundice (jaundice, darkening of urine, discoloration of feces) is characterized by localization in the head of the pancreas;
- painful - constant pain covering the upper abdomen (flatulence is often observed with frequent constipation).
- Chronic recurrent (secondary, most common, higher than the lesion) pancreatitis, like primary, has an icteric and painful form. More often it comes due to the patient having chronic cholecystitis, which weakens the gallbladder.
Symptoms
Symptoms identifying chronic pancreatitis:
- sharp or aching pain;
- discomfort in the abdominal area;
- nausea and vomiting that does not bring relief;
- diarrhea followed by constipation, flatulence;
- weight loss, weakness, fatigue;
- temperature increase.
In chronic pancreatitis, diarrhea is most often characteristic; acute forms require parallel treatment of constipation.
Diagnostics
Symptoms alone are not enough to accurately diagnose the chronic stage of pancreatitis; immediately consult a doctor and undergo certain tests and procedures. Some methods cannot detect the disease in its early stages.
Diagnosis and treatment of chronic pancreatitis are inextricably linked - which form of the disease, such drugs are prescribed. To identify the disease, the following laboratory and instrumental tests are required:
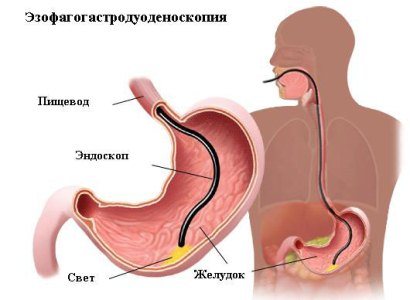
FGDS
- general blood analysis;
- biochemical blood test;
- urine;
- feces;
- Ultrasound;
- FGDS (endoscopic).
Along with traditional tests, it is typical for standards to use special instrumental ones to more accurately determine the nature of the diagnosis. Diagnosis of chronic pancreatitis does not occur in 1 day. Analyzes show the exact type of diagnosis, allowing you to decide on drugs for the treatment of pancreatitis.
Treatment of pancreatitis with enzyme preparations
Enzyme therapy is prescribed after relief of an attack of pancreatitis, characterized by severe pain. Treatment with these drugs leads to a reduction in dyspeptic syndrome, improved digestion, reduced vomiting and nausea, stabilization of body weight and cessation of diarrhea.
Enzyme group drugs are divided into two groups:
- Medicines that contain bile. Such medications are recognized as the most effective.
- Medicines without bile.
Trypsin and lipase are the main drugs for stopping pancreatic secretion. 150-300 mg of trypsin during 60 minutes in the lumen of the duodenum can normalize the secretory activity of the pancreas. Lipase can provide hydrolysis of neutral fat in amounts exceeding 20,000 units.
The above requirements meet: Creon 25,000, Creon 8,000, amylases and microspherical enzymes.
The dosage of enzyme preparations is determined by the attending physician individually for each patient. The standard prescription is 2-3 capsules of the medication, taken with or immediately after meals. In severe and very severe forms of pancreatitis, as well as in severe steatorrhea, the daily dose of lipase increases, reaching 55,000 - 60,000 units. In case of severe steatorrhea, it is necessary to prescribe vitamins of groups A, B, D, E, K, which have fat-soluble properties. Biliary-pancreatic insufficiency requires the prescription of drugs such as pankurmen and panzinorm. An overdose of enzyme preparations can lead to a decrease in the secretory activity of the pancreas, which can lead to the production of enzymes naturally in insufficient quantities.
Diet
Initially, it is important to adhere to the main treatment regimen for chronic forms of pancreatitis: cold, hunger, rest.
With an accurate diagnosis, the gastroenterologist prescribes the necessary medications and a mandatory diet, compliance with which guarantees a favorable outcome in the fight against the disease. Treatment of chronic pancreatitis requires considerable effort and patience. There is a diet No. 5B approved by a single standard. With a therapeutic diet, the main goal is complete or partial abstinence from the following foods:
It is forbidden:
- alcohol;
- smoked meats, fatty meats and fish (sausages, lamb, pork);
- carbonated drinks;
- spicy, very salty, sweet;
- sour fruits, berries, vegetables (for example, lemons, tomatoes, grapefruits, cranberries);
- yeast baked goods;
- strong coffee (in some cases limited consumption with the addition of milk is allowed).

Can:
- water-based cereals;
- vegetable broths (or chicken, lean beef);
- boiled or baked vegetables and fruits;
- dairy products with minimal fat content;
- lean types of meat, fish;
- rosehip decoction (an excellent folk remedy), weak brewed tea;
- bee products.
Food should be of moderate temperature; high or low temperature negatively affects the functioning of the gastrointestinal tract. During the first days (starting from the fourth), it is better to grind food, making the work of diseased organs easier. It should be prepared in accordance with the standards by boiling, stewing, baking, steaming, without getting carried away with seasonings. Compliance with this recommendation is important for constipation and diarrhea. You should eat often, in small portions, chewing your food thoroughly. Repeat the meal plan every 3-4 hours.
Treatment of chronic pancreatitis in the acute stage involves refusing to eat for 2-3 days and drinking plenty of fluids. It is recommended to use natural jelly without dyes - it coats the walls of the stomach and saturates perfectly.
It is necessary to adhere to a therapeutic diet for chronic pancreatitis for at least a month to obtain the result of the course of therapy; it is better to limit prohibited categories of foods even during the period of remission, especially alcohol and smoking. The total number of calories should not exceed 2000, minimal fat content, a large amount of vitamins, phosphorus-containing products, calcium salts. It would be a good idea to drink warm mineral non-carbonated water such as Essentuki or Borjomi. It is impossible to achieve complete remission with diet alone; be sure to take the medications prescribed by the gastroenterologist.
What to do during an attack of pancreatitis?
If you suspect an attack of pancreatitis, you should call an ambulance! The patient is hospitalized and is under constant medical supervision.
During an attack of pancreatitis and immediately after it, you should not eat. You are allowed to drink only plain water at room temperature.
Intoxication of the body can be reduced by taking Enterosgel sorbent. To reduce the painful signs of pancreatitis, you should place an ice pack on your stomach, ensure bed rest and complete rest.
Drug therapy
Drug treatment of chronic pancreatitis involves, first of all, eliminating pain, relieving inflammatory processes, and restoring damaged pancreatic tissue. Drugs prescribed for the chronic form are divided into various blocks:
Painkillers - usually used in the form of tablets, in acute forms in the form of injections: No-shpa, Spazmolgon, Novocaine. The treatment regimen with these drugs is relevant for exacerbation of pancreatitis.

Enzymatic - promote favorable digestion, relieving the load on the pancreas due to the presence of the necessary enzymes. Such enzymes are contained in Creon (the highest content, often prescribed for acute forms), Mezim and the most accessible one - Pancreatin. After completing the course of treatment, it is better to always keep these drugs nearby. Unexpectedly arising pain, a period of exacerbation or eating unhealthy food will smooth out any of them, being a universal first aid for a diseased organ.
Reducing stomach acidity - also relieves inflammation, reliably enveloping the stomach. The most popular medication in this segment is Almagel A. During treatment, it is recommended to use it 30 minutes before meals. The advantage of Almagel over similar medications is the presence of benzocaine, which is also an analgesic. The presence of sorbitol improves the functioning of the biliary tract, which is necessary for cholecystitis.
Antibiotics are used if chronic pancreatitis enters the acute stage.
These are not all of the medications listed; only an experienced doctor will make an exact list individually for each patient with pancreatitis of various forms.
Medicines prescribed for the course of treatment are usually taken for 10-14 days. In case of chronic pancreatitis, the home medicine cabinet should always be full, first of all, of enzyme-containing preparations. Full compliance with the diet and medication will lead to successful treatment of a serious illness.
Pathogenesis of the disease
After inflammation of the pancreas, patients with pancreatitis suffer from pain in the epigastric region and the left half of the abdomen. As a rule, pain appears after eating. This phenomenon is due to the fact that after eating food, pressure increases in the pancreas ducts. The gland secretes an excess amount of pancreatic juice, which injures the inflamed walls and tissues. The secretion is released under the influence of external regulation. Hydrochloric acid directly triggers hypersecretion in the gland. This is why it is so important to reduce the level of gastric aggression. To do this, you can use drugs from the Omeprazole group (proton pump inhibitors), or you can use antacids. We'll talk about the effects of these medications below.
Traditional methods
Treatment of chronic pancreatitis at home must be coordinated with a doctor in order to avoid complications. Traditional recipes are used mainly in combination with the instructions of the attending physician. Treatment at home provides many variations using the gifts of nature (herbs, pine pollen, bee honey). Treatment of pancreatitis with herbs involves making decoctions and tinctures using Golden Us and Celandine. The drug use regimen should be followed with great caution, given that Celandine (without the addition of milk) is toxic in large doses. Preparing tinctures or decoctions at home does not require large expenses, limiting yourself to one trip to the pharmacy.

Celandine
The most successful variants of traditional methods for coping with chronic pancreatitis are identified:
- Method according to Neumyvakin.
- Treatment with bees.
Each method should be considered in more detail.
According to Neumyvakin
The famous professor of medical sciences devoted many years of his life to the study of diseases, symptoms, and treatment methods. The findings he identified do not require the use of a wide range of medications.
The pillars of his technique are periodic cleansing of the body, changing lifestyle, drinking soda and hydrogen peroxide. The basic principles for developing standards for treating the pancreas are ordinary baking soda.
A very affordable remedy, familiar to every housewife, you should start using a minimum dose (1/5 teaspoon), gradually accustoming the body, increasing the dosage to 1 teaspoon. It is recommended to take soda on an empty stomach half an hour before meals. The obvious benefit of baking soda-based products is to regulate the acidity of the stomach, because soda is an alkali that, due to its chemical properties, can neutralize hydrochloric acid. It is strictly not recommended to take it for a long time - the body may get used to receiving alkali from the external environment.
Treatment with bees
The healing function for the body in case of chronic pancreatitis is provided by the waste products of ordinary bees. The most popular products are:

- flower pollen contains a huge fund of biologically active substances. It is recommended to consume pollen one teaspoon at a time, holding it under the tongue until completely absorbed. The use of flower pollen can be replaced with pine pollen, while reducing the dosage by three times;
- honey - used in many ways, especially often diluted with warm water or mixed with soda, drunk on an empty stomach;
- bee bread is a product created by bee pollen that surpasses it in energy value. The application is identical for both products;
- propolis - the most commonly used tincture of propolis. Relieves inflammation and acute sharp pain.
Surgical intervention
Therapy for pancreatitis rarely leads to the operating table, being limited to a therapeutic diet and medications. Surgery becomes a necessary method of treatment for persistent pain after completing a course of drug treatment. What is eliminated during surgery:
- purulent lesions;
- blockage of the biliary tract;
- stenosis of the sphincter of Oddi for favorable bile and pancreatic duct. This operation is called sphincterotomy, which requires widening and cutting the opening through which the pancreatic duct passes;
- removal of the whole or partial gallbladder - in case of irreversible damage to the bile duct;
- partial cutting off of the stomach;
- removal of pancreatic stones.
The operation is scheduled for the next day after careful preparation. Most often, surgery is determined for purulent neoplasms that secrete toxic decay products, leading to intoxication of the body.
How do antacids work?
Antacids neutralize the aggressive effects of hydrochloric acid. Almagel-type preparations contain aluminum and magnesium hydroxides. We know from chemistry course that such substances react with acids to form salts and water.
For effective action, the pH of gastric juice should be less than 3 most of the day. When this value increases above 3.5, antacids absorb excess hydrogen ions and inhibit the aggressiveness of the acid. In addition, antacids do not affect the parietal cells of the stomach, which produce HCL. They simply neutralize even the gastric juice that has already been released into the intestinal lumen.
Almagel contains aluminum and magnesium bases. It is a non-absorbable antacid. Consequently, after taking it, the development of the “ricochet” phenomenon does not occur. After all, absorbed antacids form carbon dioxide upon contact with hydrochloric acid. It stretches and irritates the stomach wall, causes belching and flatulence, and stimulates the repeated release of acid.

Inflammation of the pancreas requires a rapid and prolonged reduction in the aggression of gastric juice. Magnesium preparations ensure rapid action, and aluminum salts maintain the duration of the product’s operation. Also, for pancreatitis, the form in which the drug enters the stomach walls is important. Gel and suspension are the best options here. They form large drops on the mucous membrane, which increases the area of action of the drug.
Prevention
For chronic pancreatitis, treatment boils down to taking medications and following a diet. The healing process can take a long time, while periods of remission may be replaced by periods of exacerbation. Failure to comply with the instructions of the attending physician is highly likely to lead to complications that inevitably require drastic surgical decisions. Therefore, prevention is important, requiring:
- unquestioning adherence to the instructions of the gastroenterologist;
- maintaining a diet even after undergoing a course of treatment;
- giving up alcohol;
- physical activity;
- walks in the open air;
- smoking cessation;
- regulating sufficient amounts of minerals and vitamins in food;
- drink plenty of water (regular purified water without gas);
- annual check-up with a doctor.

Methods for preventing chronic pancreatitis are relevant even for those who are healthy, because chronic pancreatitis occurs in a large number of the adult population.
Compliance with a diet, observation by a doctor, and preventive measures can relieve the symptoms of chronic pancreatitis for many years. The course of the disease will become invisible and mild, allowing you to enjoy life without unnecessary fears for your health.
Gordox: indications and recommended dosages
Antienzyme drugs for pancreatitis: a wide choice
The drug is a complete analogue of Kontrikal. The main active ingredient is aprotinin.
Read: Domperidone: drug analogues and contraindications
Indicated in the treatment of various forms of pancreatitis, including those caused by trauma and surgery.
To relieve a primary attack in adult patients, 0.5 million units of the drug are used. The antienzyme is administered by infusion.
When the patient's condition normalizes, the maintenance dose is 200 thousand units every 6 hours, but not less than 1 million per day. If general indicators improve, the dosage regimen is 0.5 million units per day.
Side effects during treatment with Gordox develop extremely rarely. Most often, hypersensitivity reactions occur, a decrease in blood pressure, and the appearance of dyspepsia are possible.
The drug is prohibited for use in the first 12 weeks of pregnancy. Further treatment is carried out according to vital indications and under the supervision of a doctor.
Important! The drug should not be taken during treatment with drugs containing dextran. This increases the risk of developing an allergic reaction.
The drug is not compatible with nutritional mixtures for parenteral nutrition or steroid hormones.
Medicines for pancreatitis in adults: drug prevention with drugs
The development of pancreatitis in adults is not uncommon. Such a disease of the pancreas can occur not only due to poor diet, alcohol abuse, but also due to an unhealthy lifestyle and many other reasons. The presence of the above factors in combination with chronic diseases such as diabetes mellitus leads to the appearance of a disease that requires treatment.
Symptoms of pancreatitis
What symptoms can be observed in adults when the disease appears? When the pancreas is inflamed, the patient may experience frequent and severe pain in the back and abdomen. The pain may be accompanied by vomiting and nausea. The patient may also complain of fatigue, drowsiness and weakness.
To detect pancreatitis, the doctor prescribes blood and urine tests and an ultrasound of the pancreas to determine how enlarged the internal organ is. Also, if necessary, the patient undergoes an X-ray examination, and based on the results obtained, the doctor determines what medications should be taken to treat the pancreas.
It is necessary to undergo examination and begin treatment not only for the inflammatory process, but also if there is an increase in the size of the pancreas.
This may be a consequence of some inflammatory process of an internal organ. The standard dimensions of a healthy pancreas in adults are 15-22 cm in length and 3 cm in width. But in the case when a deviation is detected, the affected organ needs to be treated.
Treatment of pancreatitis
For pancreatitis in adults, you must strictly follow a therapeutic diet. But if the disease has acquired a chronic form, dietary nutrition becomes a way of life for patients, otherwise, at the slightest deviation, serious complications may develop that will have to be treated for a long time.
At the first signs of pancreatitis in adults, the doctor usually prescribes a three-day fast. At this time, when the pancreas is being restored, it is necessary to drink plenty of clean drinking water in order not only to completely replenish the lack of fluid in the body, but also to prevent exacerbation of pancreatitis as much as possible.
Treatment of pancreatitis in adults is a very long process, for which you need to be prepared. To treat this pancreatic disease, you must not only take medications prescribed by your doctor, but also follow a therapeutic diet. Preventive measures will help avoid progression of the disease in the event of an inflammatory process.
Treatment is aimed primarily at restoring the functionality of the pancreas and its ability to produce pancreatic juice normally. But the patient must take all necessary measures to prevent impaired glucose tolerance, which leads to the development of diabetes mellitus.
Restoring the ability to secrete pancreatic juice helps to avoid eating disorders and food allergies, which can develop in a patient due to incompletely broken down nutrients entering the blood vessels. Destruction of the pancreas and scarring can be prevented by restoring the normal tone of the muscles of the digestive tract and stopping the active production of digestive juice enzymes.
Treatment of pancreatitis in adults is allowed only under the supervision of a doctor, when the disease is accurately diagnosed. The fact is that the symptoms of pancreatitis are often similar to the signs of other diseases.
But if pancreatitis is detected, treatment and prevention of the disease is carried out throughout life. It is necessary to follow all the doctor’s dietary recommendations, regularly take prescribed medications to eliminate the symptoms of the disease, and properly treat pancreatitis with medications.
Thus, medications for pancreatitis help patients:
- Relieve pain;
- Eliminate pancreatic insufficiency;
- Treat the inflammatory process in the damaged organ;
- Prevent the development of complications.
If the patient's condition worsens, treatment with drugs is intensified and the diet becomes strict. If the condition improves, the patient is allowed to expand the diet, increase physical activity, reduce treatment and replace drugs with weaker ones.
Features of diet and treatment
Strict adherence to a therapeutic diet can reduce the load on the affected organ during inflammation of the pancreas and helps recovery from the disease.
- In any form of pancreatitis, the patient should not eat spicy, fatty, smoked, salty foods, foods with a high content of spices, food colors, or flavors. This includes not drinking alcoholic beverages of any strength.
- In the chronic form of pancreatitis, it is necessary to avoid eating large amounts of fats and proteins. You need to eat often in small portions, and the food is often pureed. If an acute form develops, the patient is fed intravenously, and the doctor prescribes fasting.
- The patient is also given enzymatic drugs that suppress the production of pancreatic juice. This allows you to reduce pain in the left hypochondrium and improve the general condition of the body. If the condition improves, the diet may change, but enzyme preparations continue to be taken for quite a long time, in several courses.
- To eliminate pain in chronic pancreatitis in adults, cold is placed in the left hypochondrium area, which helps eliminate swelling of the pancreas. The doctor also prescribes special medications, which include anti-inflammatory drugs, analgesics, drugs that relieve spasms, and blockers of histamine receptors in the gastric mucosa.
- On their own, the patient can only take drugs such as butpa, papaverine and other known antispasmodics. Other medications can be taken only after consulting a doctor.
Treatments for pancreatitis
The following medications are prescribed to relieve symptoms and pain:
- Antispasmodic drugs. For acute pain in the abdominal area, the patient takes antispasmodics and analgesics, including butpa, analgin, paracetamol, baralgin. If the pain during an exacerbation of the disease is very severe, it is recommended not to take pills, but to administer the drug by injection.
- H2-blockers of histamine receptors. To reduce the production of pancreatic enzymes, drugs such as ranitidine and famotidine are used.
- Antacid drugs. If exocrine insufficiency is observed, which can lead to disruption of the functionality of the duodenum, the doctor prescribes drugs or mixtures such as Phosphalugel, Almagel and other medications.
Enzyme preparations include lipase, amylase and trypsin. The most well-known medications are Creon 8000, Creon 25000, Mezim, Pancreatin, Festal, Enzyme Forte, Ferestal.
Since all these products are similar in composition and have identical functions, you should consult a doctor before taking medications. At the same time, many patients choose cheaper Russian-made drugs, for example, Pancreatin.
You usually have to take medications for pancreatitis for several years. The first positive results from the treatment can be seen after one and a half to two months. You will be able to get rid of the main symptoms no earlier than in six months. For this reason, the patient can independently decide which medications to purchase. Based on your financial capabilities - more expensive or cheaper.
When treating pancreatitis, the following are prescribed:
- sedatives;
- choleretic drugs;
- hormonal agents;
- calcium;
- coating medications.
Vitamins of group B, A, D, K, E are also effective in treatment, which make it possible to compensate for the lack of nutrients in the patient’s body. To stop the inflammatory process, Aspirin or Diclofenac is prescribed.
They also help, similar to the drug but spa, to reduce pain and get rid of spasms.
Features of treatment
Acute pancreatitis is a fairly serious and dangerous disease, the treatment of which should be carried out by a highly qualified doctor - a specialist in the field of gastroenterology. It is important in such situations to avoid self-medication and timely contact a medical facility, since there is no time to waste with this disease. Lack of proper treatment can lead to the development of gland necrosis or peritonitis.
Drug therapy for this disease is carried out only as prescribed by a doctor. It is important to follow the dosage and take all medications prescribed by the doctor.
Attention! In addition to taking medications, you need to follow a strict diet, and in the acute period, stop eating altogether.
When the disease is advanced or the treatment was carried out incorrectly, drug therapy will not bring the desired results. In such cases, the doctor usually prescribes surgical treatment.
Optimal dosage of Enterosgel

It is recommended to take Enterosgel for pancreatitis in the same dosage as for the treatment of intoxication:
- newborns up to 1 year – 1/5 tsp. (2-3 g) 3 times a day;
- children from 1 to 5 years old – 1 tsp. (5-6 g) 3 times a day;
- children from 5 to 14 years old – 1 tsp. (10-12 g) 3 times a day;
- children over 15 years old and adults – 1 tbsp. (15-20 g) 3 times a day.
The duration of the course of treatment is determined by the doctor individually. Occasional treatment of pancreatitis with Enterosgel is allowed (to reduce stomach pain).
The medication is available in the form of a gel and paste, which, when ingested, do not break down and are not absorbed into the gastrointestinal tract. Therefore, substances are excreted from the intestines in their original form.











