How to treat the gallbladder
This organ is susceptible to various diseases, including cholecystitis, cholelithiasis, benign and malignant tumors, and others. Treatment of the gallbladder can be either conservative or surgical, it all depends on the diagnosis and course of the disease.
Biliary dyskinesia
For biliary dyskinesia, complex therapy is carried out, including normalization of the diet, diet, treatment of foci of infection, taking antiparasitic drugs, antispasmodics and other drugs.
Cholelithiasis
This disease is quite common and is characterized by a violation of the exchange of bilirubin and cholesterol and the formation of stones of various sizes in the cavity of the bladder, liver and bile duct. GSD can occur without symptoms for a long time, but when a stone gets into a narrow duct, an attack called hepatic colic occurs.
Treatment can be either conservative or surgical. It consists of following a diet with limited animal fats, taking medications that prevent the formation of stones and promote their removal, and resort and sanatorium treatment. To relieve pain, analgesics and antispasmodics are taken, and in case of a bacterial infection, antibiotics are taken.
In cases of persistent progression, frequent relapses and ineffectiveness of therapeutic treatment, perforation and blockage of the gallbladder, and formation of fistulas, surgical intervention is indicated.
Chronic acalculous cholecystitis
This is an inflammatory disease of the inner lining of the gallbladder without the formation of stones. There are many reasons for this development:
- Bacterial infections.
- Parasitic diseases.
- Allergic reactions.
- Stagnation of bile.
- Pancreatitis.
- Hepatitis.
- Reverse reflux of bile from the intestine containing pancreatic enzymes, which, once in the gallbladder, begin to digest its walls.
Cholangin is an acute or chronic inflammation of the biliary tract, most often caused by bacteria. May occur after removal of the gallbladder. Treatment is carried out with antibacterial, antispasmodic, antiparasitic, anti-inflammatory drugs. Surgery is often required.
Malignant tumor
Cancer of this organ is characterized by high malignancy and early formation of metastases. This can be squamous cell carcinoma, adenocarcinoma and others. Most often, the oncological process develops in the gallbladder affected by a chronic inflammatory disease. Treatment consists of early surgery and chemotherapy.
Treatment
After making an accurate diagnosis, the doctor determines how to treat the disease.
- First of all, you need to follow a diet. You need to switch to proper and fractional nutrition.
- In addition, drug therapy is carried out.
- To supplement and quickly recover, you can also use traditional medicine recipes.
- If treatment does not produce any results, cholecystectomy is performed, that is, surgery to remove the gallbladder.
Traditional therapy
Let us immediately note that medications can only be prescribed by a doctor. Self-medication for gallbladder diseases is unacceptable. Traditional therapy consists of taking the following tablets:
- Choleretics (Nicodin, Cholestil, Berberine, Vigeratin).
- Antispasmodics (Drotaverine, No-Shpa, Duspatalin, Papaverine) to relieve pain.
- Choleretic drugs (Ursosan, Heptor, Holosas).
- Antibiotics (Cefazolin, Ampicillin, Oxamp).
- Preparations for normalizing digestion (Creon 10000, Creon 25000, Mezim, Pancreatin, Penzital).
- Drugs that increase the tone of the gallbladder (Xylitol, Sorbitol, Pituitrin).
- Sedatives (Motherwort, Novopassit).
In parallel with drug treatment, therapeutic procedures are carried out - DMV therapy, electrophoresis.

Treatment with folk remedies
As an addition to the main treatment, you can use folk remedies. With the help of herbal medicine, you can properly cleanse the gallbladder. We will describe only the most effective recipes for decoctions and infusions that have choleretic properties:
- Rosehip decoction. 3 tbsp. l. Pour boiling water (300 ml) over the berries and simmer for 5 minutes over low heat. Let cool and strain. Take 100 ml before meals 3 times a day.
- Beetroot decoction. Peel 2 medium-sized beets and cut into small pieces. Pour 1 liter of water, bring to a boil and cook over low heat for 5 hours. Then pass the beets through a grater and squeeze out the juice using gauze. Combine this juice with the water in which the beets were previously boiled. Take 60 ml before meals 3 times a day.
- Lingonberry infusion. 2 tbsp. l. Pour two cups of boiling water over crushed lingonberry leaves, cover with a lid and leave to steep for 40 minutes. Take 30 ml before meals 4-5 times a day.
Where is it located?
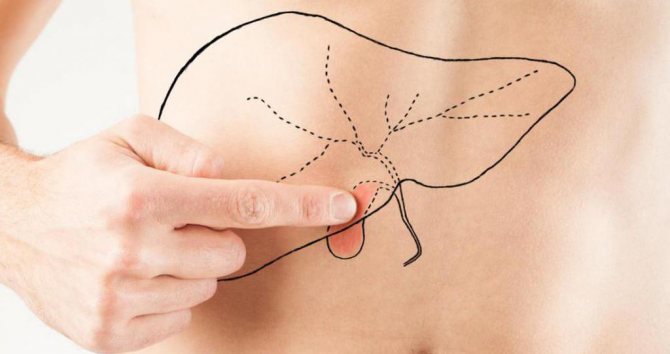
How to find out where the gallbladder is located? It's actually quite simple. First you need to connect the upper edge of the right armpit and the navel with a conditional line. Then find the point of intersection of this line with the costal arch. In this way, doctors determine the point where the organ is located. When a patient is examined, the examination involves palpation of the gallbladder in the right hypochondrium, that is, palpation. With normal sizes, the doctor will not be able to palpate it in the right hypochondrium, since the organ has a soft consistency and protrudes from under the liver by a maximum of 1 cm.
However, in some conditions it is possible to palpate the gallbladder. These are conditions in which the size increases or the consistency changes, for example:
- dropsy;
- stone formation;
- purulent inflammation (empyema);
- benign tumors;
- malignant neoplasms.
For various diseases, the doctor can palpate specific changes. For example, if the cervix is blocked by a stone, then a tuberosity can be felt. If there is, for example, dropsy, then a smooth formation of elastic consistency is palpated. You can feel a solid cancer formation.
However, even in these conditions, you may not be able to palpate the organ, but it is possible to identify a number of symptoms. For example, pathology may be indicated by pain on palpation. There are many symptoms and techniques for identifying gallbladder pathology that the doctor uses during an objective examination. First, the doctor asks about complaints, then examines the patient, and then prescribes treatment.
The most informative will be laboratory and instrumental examinations of the anatomical and functional state of the organ. The most common and accessible today is ultrasound (ultrasound examination), which will show normality or pathology. The examination will show the size of the gallbladder, its shape, and the presence of any formations in the body itself or in the cervix. The length of the gallbladder in an adult is from 7 to 14 cm, width from 3 to 5 cm, and capacity from 40 to 70 ml, the length of the cystic duct is 3-4 cm. It should be noted that the normal dimensions of the gallbladder change from birth to adulthood . Age characteristics are taken into account when the doctor does an ultrasound, but pediatricians are more closely involved in this.
In any case, if you notice discomfort, pain, heaviness in the right hypochondrium, yellowness of the skin and mucous membranes, if your relative or friend complains, then you should suspect a problem with the gallbladder and seek medical help.
Specifics of pancreatic functions
Pancreatic juice (up to 2 liters per day) contains more than 20 enzymes, classified into three groups:
- Lipases break down fats.
- Proteases break down proteins.
- Amylases are involved in the breakdown of carbohydrates.
These enzymes remain inactive until they interact with gallbladder secretions.
Bile ducts
The most important common bile duct is formed as a result of the fusion of the cystic (departs from the neck of the bladder) and hepatic ducts. In turn, the common bile duct consists of 4 sections:
- Retroduodenal - located behind the upper horizontal region of the duodenum (duodenum);
- Supraduodenal - localized above the duodenum;
- Intramural - in the wall of the vertical part of the duodenum;
- Retropancreatic - posterior to the head of the pancreas.
The mechanism of bile excretion is as follows:
- Bubble contraction;
- Opening of the bladder valve;
- Opening of the sphincter of Oddi;
- Influx of bile into the duodenum.
What if I delete it?
Cholecystectomy is the name given to resection (removal) of the gallbladder. In severe cases of pathology, it becomes the only way to save the patient’s life. The function of the gallbladder will be taken over by the duodenum. But with this option, bile will constantly enter it, which will lead to a disorder of the microflora in the intestines, constipation or diarrhea.
When resection of the pancreas or part of it, the patient is prescribed replacement therapy with glucose-lowering drugs or enzymes. Impaired secretion of insulin by the gland requires adherence to a strict diet for a very long time, sometimes throughout life (table 9 for diabetes, table 5 for pancreatitis).

Possible problems with the gallbladder and causes of its pain
The following signs and symptoms are characteristic of diseases of the gallbladder and its duct.
- Painful sensations. They arise in the right hypochondrium and can radiate to the area of the right shoulder and scapula.
- Yellowness of the sclera and skin.
- Itchy skin.
- Dyspeptic disorders: nausea, feeling of heaviness and fullness of the stomach, heartburn, belching, etc.
- Increased pain and dyspepsia after eating hot, spicy and fatty foods, as well as after physical activity or stress.
All these signs should make a person wary of diseases of this organ. Let's consider the main pathology of the bladder and its ducts and how it manifests itself.
1. Biliary dyskinesia
A pathology in which the motor activity of the bladder and its duct changes. This is due to a violation of its contractile function and uncoordinated work of the excretory duct. The causes of the problem are considered to be emotional and mental overload, stress, changes in diet and excess weight. Dyskinesia itself is not a problem, but it leads to stagnation of bile and is a prerequisite for inflammation of the gallbladder or the formation of stones. The disease may not bother the patient for a long time, but sometimes the disease manifests itself with the following symptoms:
- discomfort in the right hypochondrium or aching dull pain;
- problems with appetite;
- sleep disorders;
- emotional lability.
Jaundice and skin itching do not occur with this disease. The diagnosis is made on the basis of a characteristic ultrasound picture.
2. Gallstone disease
The disease is accompanied by the formation of calculi (stones) in the bladder itself or its ducts. These stones are clots of bile on which bacteria (during inflammation), desquamated epithelium and other components are layered. Among the main risk factors for this disease are:
- genetic predisposition;
- eating disorder;
- excess weight;
- disruptions of hormonal regulation, for example, during pregnancy;
- sedentary lifestyle, etc.
Symptoms and pain associated with this disease depend on the location and number of stones. Patients may complain of:
- pain in the right hypochondrium;
- feeling of fullness in the stomach, flatulence;
- problems with stool and appetite.
A reliable clinical sign of stones is an attack of hepatic colic - a condition in which a stone completely obstructs the mouth of the bile duct. When the doctor asks how it hurts and where, the patient will point to the right hypochondrium. In this case, sharp and intense pain may be accompanied by nausea and vomiting. After an attack of hepatic colic, the patient may have discolored stool and dark urine, which is associated with a temporary lack of bile in the intestines. The diagnosis is made on the basis of ultrasound signs. Treatment is conservative or surgical.
3. Acute and chronic cholecystitis
Acute or chronic inflammation of the organ wall is associated with the pathogenic effect of a bacterial infection. Dyskinesia and the presence of stones in it contribute to the development of the disease; protozoa, for example, Giardia, can play a certain role in the development of inflammation.
The acute form is accompanied by severe pain in the liver area, stool disturbances, nausea and a rise in body temperature. With illiterate treatment and the presence of factors that support inflammation, the acute process becomes chronic. Chronic cholecystitis occurs with periods of exacerbation and remission.
4. Gallbladder neoplasms
Benign (polyps) and malignant neoplasms of the gallbladder in the early stages are asymptomatic. As they grow, they lead to pain, jaundice and indigestion. The clinical picture depends on the type of tumor and its extent.
The gallbladder may bother the patient for various reasons. Most often, the problem is caused by errors in diet and poor lifestyle; less often, the disease is caused by tumors and polyps. To clarify the diagnosis and select a treatment regimen, you should visit a specialist.
https://youtube.com/watch?v=Y6AEZiaKIWI
Gallbladder
Gallbladder (vesica fellea)
(Fig. 1.2) appears in early embryogenesis as a sac-like protrusion of the hepatic diverticulum.
In an adult, the gallbladder, which looks like an elongated flask with varying capacities (25–70 cm3 ),
is located in the anterior segment of the right longitudinal groove (gallbladder fossa).
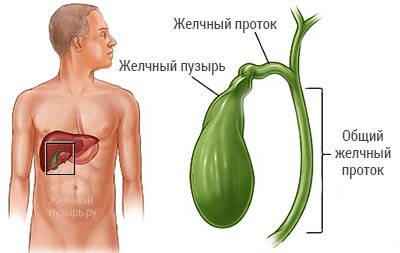
It distinguishes between the bottom, body and neck, which gradually turns into the cystic duct (ductus cysticus).
The wall of the gallbladder consists of: mucous membrane with submucosa; poorly developed muscular with a predominantly circular direction of the bundles and serous with a slightly pronounced subserosal base. The mucous membrane of the fundus and body has peculiar folds, giving it the appearance of shagreen skin, and in the neck and in the cystic duct the folds of the mucous membrane usually have a spiral course (spiral fold). In the hepatic and common bile ducts the mucosa is smooth. The serous membrane covers most of the gallbladder, the rest fuses with the fibrous capsule of the liver through loose fiber. The hepatic and common bile ducts are located in the thickness of the hepatoduodenal ligament.
Rice. 1.3. Lymphatic vessels of the diaphragmatic surface of the liver.
Rice. 1.4. Perivascular lymphatic vessels of the liver parenchyma.
Topographic anatomy of the liver and gall bladder. The liver is in contact with many organs: most of its diaphragmatic surface is adjacent to the diaphragm and a smaller part is adjacent to the anterior wall of the abdominal cavity. Adjacent to the internal surface of the liver on the right are the right kidney with the adrenal gland, the duodenum and the right flexure of the colon, and on the left are the esophagus and the fundus of the stomach.
The highest point of the upper border of the liver is projected onto the right fifth rib along the midclavicular line. From here, the upper border steeply descends to the right and down to the right tenth intercostal space along the mid-axillary line, and to the left it follows horizontally to the left fifth intercostal space along the parasternal line. The lower border of the liver coincides with the oblique connecting the two lower points of the upper border. The gallbladder is adjacent to the initial part of the upper part of the duodenum, the pyloric part of the stomach, the right flexure of the colon and, in a stretched state, to the anterior wall of the abdominal cavity.
The blood supply to the liver is carried out by branches of the own hepatic artery. In addition, venous blood from the portal vein enters the liver. Venous blood from the liver parenchyma mixes with the blood of the portal vein and, together with the latter, flows through the hepatic veins and the inferior vena cava. There are no lymphatic capillaries inside the liver lobules; they are concentrated in the perivascular fibrous capsule both inside and on the surface of the organ (Fig. 1.3, 1.4). The efferent lymphatic vessels go to the hepatic, celiac, right gastric, diaphragmatic and posterior mediastinal lymph nodes. Innervation of the liver and biliary tract is carried out by branches of the hepatic plexus (vagus and phrenic nerves, sympathetic trunk).
Structure of the gallbladder and ducts
To imagine where the gallbladder is located and what the “bile storage” looks like in the body, the easiest way is to imagine a small pear-shaped pouch 8–14 cm long, 2–5 cm wide, and with a volume of up to 70 cubic cm. The following sections are usually distinguished in the structure of cholecystis :
- body - it is located between the neck and the bottom;
- neck - located in the narrowest part of the body and ends with the exit (or entrance) to the cystic duct;
- the bottom is round in shape - located in the widest part of the bag.
The walls of the bladder deserve special attention, because they help thicken the bile and make it more concentrated. It is this bile that is the first to enter the duodenum during the digestion of food, so it must have greater strength and ability to start the digestive process in the intestines.
How walls work
In order for more bile to fit into the cholecystis and for it to be more concentrated, cells on the inner surface of the walls of this organ reabsorb fluid from the bile. Therefore, the bile in the bladder is thicker and darker (almost black) than the fresh bile secreted by the liver into the hepatic ducts.
In addition, the walls of cholecystis are covered with a layer of muscle tissue, which is capable of contracting, compressing and in this way pushing bile into the ducts and further into the intestine.
There is another layer on the wall of the cholecystis, more precisely, on its neck - the circular muscles. They make up the muscle tissue of the valve, or sphincter, which opens and closes the entrance to this organ.
- mucous membrane - a thin folded layer lined with epithelium;
- muscular layer - a circular layer of smooth muscles that pass at the end of the neck into the shutter valve - Lutkens sphincter;
- adventitia - a layer of dense connective tissue consisting of elastic fibers.
Structure and location of ducts
Now that the question of where the gallbladder is located can be answered even in a dream, let’s look at the location of the ducts. Let us consider only those of them that are located outside the liver parenchyma, although microscopic ducts are present in each liver cell that synthesizes bile.
- The liver consists of the right and left lobes, from which the right and left hepatic ducts branch, respectively. Having merged, they form the common (joint, main) hepatic duct.
- The main hepatic duct goes to the duodenum.
- On the way to the duodenum, the cystic duct, emerging from the cholecystis, joins the main hepatic duct.
- The fused cystic and hepatic ducts form the common, or joint, bile duct.
Any disturbances in the production and excretion of bile lead to serious disruptions in the functioning of the entire biliary system, pathological thickening of bile, the formation of stones and, as a consequence, the appearance of bile-hepatic colic and other unpleasant symptoms.
What is the gallbladder and where is it located, photo
The gallbladder is a small hollow organ, measuring from 4 to 7 centimeters, located at the lower edge of the liver in a specially designated recess. Its main task is to store and accumulate bile produced by the liver. In addition, it is a kind of filter that removes water from less abundant bile, thereby increasing its saturation.
A duct emerges from the gallbladder - a three-centimeter tube connecting the organ with the common hepatic duct. This is followed by the pancreatic outlet and the duodenum, the first lobe of the small intestine.
From 700 to 1200 grams of bile passes through the gallbladder per day. The amount may vary depending on the amount of fluid you drink, diet, and even the state of the nervous system.
Bile contains substances such as organic acids, cholesterol and bilirubin to a greater or lesser extent. The latter gives the bile a specific reddish tint.
Bile begins to be actively produced after each meal. The nervous system encourages the gland to work. Bile is needed to help food digest. This is especially true for fats, which are practically not broken down by gastric juice. In addition, bile, together with pancreatic juice, which is produced by the pancreas, perform a protective function, neutralizing the negative effects of gastric juice on the intestinal walls.
Diagnostic measures
If symptoms of gallbladder disease appear, you should consult a doctor. The specialist will prescribe the necessary laboratory and instrumental tests and determine treatment tactics.

To identify gastrointestinal diseases, instrumental and laboratory studies are carried out
Using a blood test (general and biochemical) you can identify an inflammatory lesion or a disorder in the functionality of the gallbladder. The disease can be indicated by an increase in the concentration of leukocytes, a change in ESR (erythrocyte sedimentation rate), and an increase in the amount of bilirubin.
During duodenal intubation, the patient is inserted into the duodenum. This is necessary to collect bile and examine it. Using this diagnostic method, you can determine the composition of bile and the presence of white blood cells (leukocytes) in the mucus. These indicators indicate inflammation. In addition, it is strongly recommended to carry out bacterial culture of liver secretions to identify the causative agent of the infectious disease.
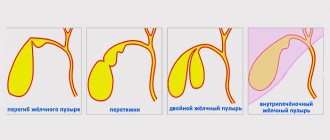
Using ultrasound, congenital anomalies (for example, a bend of the gallbladder) and neoplasms are detected. Precise equipment will show the thickness of the organ, its diameter, location, etc. Sometimes the gallbladder is not visible on the image, then there is a suspicion of a disabled gallbladder.
A biopsy (sampling of tissue cells) can detect gallbladder cancer.
If pain occurs on the right side under the ribs, an x-ray using a contrast agent is often prescribed. Using the study, the dimensions of the organ are assessed and deformation is identified. X-ray examinations are prescribed if a disconnected gallbladder is suspected.
Using computed tomography and magnetic resonance imaging of the abdominal organs, the size and location of the organ, various tumors, stones (even small ones), and polyps are revealed. These diagnostic methods are used for stagnation of liver secretions in the gallbladder.
Diagnostic methods
The presence of pathological processes in the gallbladder should not be ignored. It is necessary to undergo a consultation and diagnostic examination with an oncologist. Based on the patient’s complaints at the time of contacting the clinic, his general examination, the following diagnostic measures are prescribed:
- general and chemical blood test;
- fibrogastroduodenoscopy to determine the type of infection that provoked the pathology;
- cholecystography (x-ray examination using a contrast agent);
- Ultrasound of the gallbladder, determining the degree of deformation of the organ, its thickening;
- cholegraphy with a contrast component to assess the functional capacity of the biliary tract;
- radiography, which determines the size and functional abilities of the organ;
- MRI, CT, helping to recognize changes in tumor formations.

Based on the examination results, doctors prescribe appropriate treatment.