A healthy gastrointestinal tract allows every person to fully enjoy life, since it is with food that many people truly enjoy the taste of their favorite dishes. And when stomach problems begin, unpleasant symptoms such as heaviness, nausea, bloating, and heartburn may occur throughout the day.
To prevent the occurrence of serious diseases in the form of ulcers, pancreatitis, gastritis, it is necessary to carry out stomach prophylaxis. If you ignore it, you may soon end up in a hospital ward, since a malfunction in the gastrointestinal tract disrupts the normal functioning of other organs.
Table of contents
- Causes of diseases
- What are the symptoms of stomach ulcers and gastritis Symptoms of gastritis
- Signs of a stomach ulcer
- Endoscopic signs
- Antibacterial therapy
Nervous overstrain
The cause of gastritis may not only be poor nutrition. Stomach pain often occurs during a period when a person experiences nervous tension, gets tired, and does not get enough sleep. Prevention of chronic gastritis involves healthy sleep. None of the internal organs can function fully if a person is awake at night. And the stomach is no exception.
In order to get rid of the disease, you should first of all change your lifestyle, then your diet, and last but not least, think about taking medications. This is approximately how the above-mentioned Tibetan monks reason. It's hard to disagree with their point of view. Nevertheless, many sufferers prefer to take a life-saving pill rather than follow a diet that is indispensable for the prevention of gastritis.
Causes of diseases
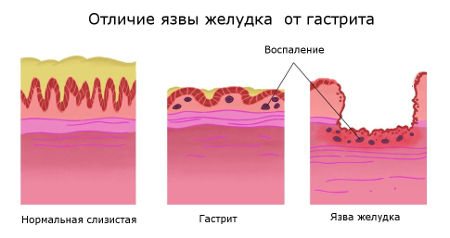
External and internal factors play a role in the development of inflammation and the appearance of mucosal defects. They lead to changes in epithelial cells, which contributes to disruption of hydrochloric acid production and changes in acidity in the stomach. But there is a difference between these states. Gastritis can have different pH levels. This is its main difference. An ulcer is characterized by high acidity of gastric juice. The duodenum is also subjected to aggressive action with the formation of lesions in the area of the bulb.
Pathological conditions arise due to the following reasons:
- Infection with Helicobacter pylori is the main etiological factor, which is detected in 80-90% of patients.
- Poor quality nutrition with consumption of harmful foods.
- Psycho-emotional stress, stress, overwork.
- Taking certain medications for a long time - non-steroidal anti-inflammatory drugs, antibiotics, sulfonamides.
- Endocrine system disorders.
- Diseases that provoke an increase in pH are carcinoid syndrome, Zollinger-Ellison syndrome, gastrinoma.
- Autoimmune pathology.
- Exposure to occupational factors - alkali vapors, acids, radiation, coal and metal dust.
- Smoking and drinking alcohol.
- Hereditary predisposition.
Causes of gastrointestinal inflammation
The stomach usually becomes inflamed due to:
- unbalanced diet;
- eating disorders;
- consumption of fast foods, hot spices;
- lack of fresh fruits and vegetables in the diet;
- taking medications;
- weakened immune system.
Eating fatty foods and fast food containing preservatives and chemical additives, irrational combinations of foods, poor lifestyle and bad habits have a negative impact on the body and lead to dysfunction of the digestive system.
Any disease associated with the stomach causes discomfort, as it is often accompanied by severe pain. Ignoring warning signs can result in death. Even ordinary gastritis does not need to be started, as it will quickly develop into an ulcer.
Preventive measures that children and adults should adhere to will help reduce the risk of developing the disease.
What are the symptoms of stomach ulcers and gastritis?
Changes in the mucosa, which are characterized by inflammation and the formation of defects, have similar clinical signs. The conditions differ in their chronic course. In recent years, classic symptoms of gastritis and gastric ulcers affecting the duodenum have been observed less frequently. Often there is a hidden form of disease. However, there are features that help differentiate the type of pathology.

Symptoms of gastritis
Chronic inflammation of the gastric mucosa has distinctive signs. Depending on the pH level, patients experience different symptoms of gastritis. Hypersecretion of gastric juice causes reflux and inhibits intestinal motility. When epithelial cells are destroyed, secretion ceases to be produced, and a hypoacid state occurs. Low production of hydrochloric acid leads to difficulty digesting food and impaired absorption of vitamins and nutrients. The pathology variant can be distinguished by symptoms independently.
Manifestations of gastritis with high acidity include:
- aching pain in the upper abdomen;
- burning in the epigastrium;
- belching with a sour taste, with bile reflux - with an admixture of bitterness;
- frequent vomiting after eating;
- feeling of heaviness in the stomach;
- increased saliva production;
- disruption of intestinal function in the form of constipation.
A decrease in pH in the stomach can be suspected if the following signs are present:
- nausea after eating;
- belching with an unpleasant putrid odor;
- metallic taste in the mouth;
- feeling of fullness in the stomach;
- discomfort or dull abdominal pain that occurs 20-30 minutes after eating;
- bloating;
- unstable stool, diarrhea;
- dry, brittle hair and nails;
- anemia.
The progression of the pathology leads to nutritional deficiency and loss of body weight. There is general weakness, decreased performance, and lethargy. There is a violation of vascular tone, which leads to the formation of hypotension. Therefore, when the disease worsens, loss of consciousness occurs.
Signs of a stomach ulcer
Constant exposure of the mucous membrane to an aggressive environment leads to the appearance of defects. The lesions come in different sizes - from 0.3 cm to 5 cm in diameter. They can be localized in the stomach and duodenum. Depending on the clinical variant of the disease, certain signs of a stomach ulcer are observed. The pathology is characterized by a chronic course with periodic relapses. In severe cases, there are complications such as:
- bleeding;
- perforations;
- penetration - when the process can spread to adjacent organs;
- stenosis;
- malignancy.
The main manifestations of peptic ulcer disease are:
- belching with sour contents;
- heartburn;
- pain that occurs mainly at night or on an empty stomach;
- vomiting and nausea after eating;
- progressive weight loss;
- anemia – if there is bleeding from a peptic ulcer.
If complications occur, other symptoms appear that reflect damage to the corresponding organ. Given the disruption of the outflow of gastric juice, chronic duodenitis, biliary tract dysfunction and secondary pancreatitis develop in adults. Destruction of the mucous membrane leads to perforation (rupture). This is an acute condition that requires emergency surgery. Modified tissues of a peptic ulcer can degenerate with the formation of stomach cancer.
What is the difference between an ulcer and gastritis?
The mechanism for the development of inflammation and the formation of a mucosal defect has common features. Focal changes in the stomach are a consequence of excessive exposure of the epithelium to hydrochloric acid. Therefore, the diseases are similar not only in pathogenesis, but also in manifestations. However, patients often have a question: how to distinguish gastritis from an ulcer?
Pathological conditions can be identified by symptoms. Features are reflected in Table 1.
Table 1. How gastritis differs from a stomach ulcer
| Signs | Gastritis | Stomach ulcer |
| Pain syndrome | After eating 20-30 minutes | Intensifies at night and on an “empty stomach” |
| Belching | Sour, bile - with excess production of gastric juice, with a putrefactive odor - with low pH | Sour |
| Character of the chair | Alternating constipation and diarrhea | Constipation |
| Anemia | Most often hypochromic due to deficiency of nutritional iron | Most often normochromic due to bleeding |
| Asthenic syndrome | Moderately expressed | Progressing |
| Bleeding (stomach) | Not marked | Occurs during periods of exacerbation |
Diagnostics: how to check the stomach for gastritis and ulcers
Examinations for pathology of the digestive system are carried out in accordance with the protocol. The appearance of unpleasant symptoms from the gastrointestinal tract is an indication to consult a gastroenterologist. The specialist clarifies the patient’s complaints, medical history and assesses the objective status in order to distinguish gastritis from an ulcer. The next stage is additional diagnostics.
The following methods are prescribed:
- General clinical blood test with mandatory determination of hemoglobin, red blood cells, hematocrit.
- Biochemical examination.
- Identification of the pathogen - carrying out a respiratory urease test for Helicobacter, microscopy of mucus smears for quantitative analysis, qualitative research using PCR, immunohistochemistry.
- pH metering - to determine the acidity in the stomach.
- Analysis of feces for occult blood with a coprocytogram.
- X-ray examination with contrast of the stomach and intestines.
- Fibrogastroesophagoduodenoscopy with biopsy and subsequent histology of the material.
Important!
General clinical data indicate the severity of the pathology. Instrumental studies help determine how gastritis differs from a stomach ulcer.
Ultrasound diagnostics is used as an auxiliary method. However, an ultrasound will not show changes in the mucous membrane. Such an examination reveals concomitant pathologies and complications of the underlying disease.
Endoscopic signs of gastritis and ulcers
Visualization of the mucosa using FGS is the main research method. Signs of gastritis and stomach ulcers cannot always be distinguished by symptoms. However, endoscopy allows a definitive diagnosis. There are diagnostic features to differentiate diseases.

Endoscopic photo shows signs of gastritis and stomach ulcers
Table 2. Endoscopic signs of gastric ulcers and gastritis
| Criteria | Signs of gastritis | Signs of an ulcer |
| Nature of folds | Evenly spaced, easily expanded with air, thickened in the presence of edema and infiltration | Concentrated near the pathological area of the mucosa |
Mucosal color | Red in color, in places with small dotted inclusions similar to enanthema in scarlet fever - in a hyperacid process. Pale gray or cyanotic color, sometimes alternating light and pink areas that resemble a mosaic with the formation of “false” hyperemia | Hyperemia in the area of inflammation, in places there are scars of connective tissue, initially red and then pale |
| Presence of defects | No | A rounded lesion with an edematous ridge, a depression in the center, covered with a gray or yellow coating |
| Bleeding | Determined when the instrument comes into contact with inflamed and swollen mucosa | Marked at the bottom or edges of the ulcer |
| Vascular pattern | Clearly visible during the atrophic process; not detected in hyperacid gastritis | Moderate in remission, not detected during exacerbation of the disease |
How to properly prepare for gastric endoscopy
Just about health: how to prevent gastritis and can it be cured?
The food each of us eats in a lifetime weighs about the same as one adult blue whale, the largest animal on Earth. It is not always correct and of high quality.

© CC0/pixabay/michaelform
Just about health: osteoporosis is a “silent robber” of the body
About 80% of people have experienced an episodic manifestation of acute infectious/non-infectious gastritis at least once in their lives.
According to statistics, gastritis is a disease of the middle class, white collar workers and residents of big cities. The poorest population of the Earth, the wild tribes of Africa, amaze with mortality statistics from epidemics of fever, typhoid fever, AIDS... but with constant malnutrition and an incomprehensible diet, cases of gastritis or ulcers are rare among them. The same cannot be said about WHO statistics on gastritis in developed countries!
What is gastritis? Let’s look at it from a physiological point of view.
Our stomach is part of the body's digestive system. It is needed to digest food, from which we obtain building material for our cells, energy for life and a complex of vitamins and minerals for proper biochemical reactions in the cells of all organs and systems.
The digestive system is autonomous, it lives in its own rhythm and at its own speed. A person does not feel or control when and how food passes from the stomach to the duodenum.
What causes gastritis?
According to most physiologists, gastritis begins with food and oral hygiene.
The quality of the products and the composition of the dishes also matter.

© CC0/pixabay/mirceaianc
Just about health: why is vitamin D so important?
Hands and utensils in which food is prepared and eaten must be clean. The bacteria that cause gastritis are transmitted through the oral and oral-fecal routes.
We have taste buds in our mouths, through which we determine the good quality of food. Therefore, oral hygiene is very important!
The digestion process begins with thorough chewing of food - this way it is easier and more abundantly moistened with saliva. This is also important because only saliva contains enzymes that break down glucose and bactericidal substances. Well-chewed food is qualitatively broken down in the stomach, but large pieces are not completely digested due to the shallow penetration of enzymes and, when passing further along the digestive tract, can injure the sphincters, which also affects gastroesophageal reflux. If this happens sporadically, then a big problem will not happen, but if this is a way of eating, then problems cannot be avoided!

© CC0/pixabay/mrsbrown
The main cause of gastritis is poor diet.
The digestive tract contracts at the right rate, allowing food to undergo the correct process of fermentation and digestion. You can’t eat “on the go,” you can’t rush while eating, because, in addition to swallowing excess air, which then comes out in the form of belching, we disrupt the speed of physiological motility of the digestive tract.

© Sputnik / Viktor Tolochko
Just about health: how to understand why your heart hurts
From the digestive tract, food enters the stomach, a muscular organ. The process of disinfection and further fermentation of food occurs in it.
Gastritis is an intense/long-lasting inflammation of the gastric mucosa.
The stomach produces hydrochloric acid, a very caustic substance. A razor blade can easily dissolve in human gastric juice! To prevent acid from damaging the stomach, its walls are covered with special parietal cells that secrete protective mucus.
Hydrochloric acid is very important; it determines the level of acidity in the stomach. Any deviation from the norm has its consequences, including in the form of inflammation of the mucous membrane.
Can a person somehow influence this process?
There is a popular expression: “don’t eat dry food.” And it appeared for a reason.
The formula of hydrochloric acid is HCL. There are cells in the stomach that produce chlorine compounds, but it can only become acidic if there is water (liquid) in the food. If a person with normal acidity eats dry food, over time he will develop dyspeptic disorders.
Signs that may indicate gastritis:
- feeling of heaviness or discomfort in the abdomen;
- decreased and worsening appetite;
- nausea and bloating;
- vomit;
- decreased performance;
- pain in the stomach;
- belching and unpleasant taste in the mouth;
- heartburn;
- diarrhea.
All of these symptoms may be the consequences of a simple disorder of the gastrointestinal tract. However, if there is a combination of two or more of these conditions or this repeats a couple of times a week for three months, you should definitely consult a therapist or gastroenterologist, because not only gastritis, but also many serious diseases can masquerade as dyspepsia.

© CC0/Pixabay/skeeze
Just about health: arthrosis, arthritis and other joint diseases
Unfortunately, in case of stomach problems, most often a person’s first assistant is a pharmacist, not a doctor. By self-medicating, you can miss the onset of a serious illness, so after relief of symptoms, be sure to consult a doctor.
The tricky thing about gastritis is that it can be painless.
There is always a distinction between the concepts of “functional dyspepsia” - this is a clinical diagnosis and “gastritis” - a diagnosis that is made only on the basis of a morphological study.
Today there are several classifications of gastritis. At the congress in Kyoto (Japan), new aspects of the classification of gastritis were adopted:
- autoimmune (type A);
- infectious associated Helicobacter Pylori;
- bacterial (enteroccoci, mycobacterial, secondary syphilitic);
- viral;
- parasitic;
- fungal.
If left untreated, acute gastritis can become chronic.
External causes that may influence the development of gastritis:
- abuse of strong alcoholic drinks;
- irritation of the gastric mucosa by chemicals and drugs (non-steroidal anti-inflammatory, steroid and glucocorticoid hormones);
- sudden change in the acid-base balance of the stomach (due to the use of substances with a pronounced pH factor, such as vinegar);
- questionable quality of food.
Gastritis is a precancerous condition, so it should be taken very seriously.
Dangerous bacteria
30 years ago, the bacterium Helicobacter Pylori was discovered, which leads to chronic gastritis, and subsequently to stomach cancer. To date, treatment protocols have been developed that lead to good results, but not everything is so simple here.
According to various sources, 87%-95% of the population are carriers of this bacterium, but not everyone gets sick.
For this bacterium to cause a disease, certain conditions must be created, in particular, an active decrease in immunity, changes in the functioning of the immune system.
© Sputnik
A rural doctor writes a video blog about healthy lifestyle and fitness.
FGDS and other research methods
Gastritis caused by Helicobacter Pylori is in first place in terms of prevalence. But in order to determine it in the body, an integrated approach to diagnosis is required.
The gold standard in diagnosing gastric diseases is fibrogastroduodenoscopy (FGDS). A special probe is lowered into the esophagus, stomach, and duodenum.
Many people are afraid of this study due to the strong activation of the gag reflex and other phenomena associated with it. But today, almost everywhere, this study is carried out under sedation. Everything goes quickly and painlessly and takes no more than 10 minutes.
During FGDS, gastric material is collected for examination. This can include gastric juice and scraping (biopsy) of ulcerated areas of the digestive system. The biopsy material is examined by pathologists, they determine whether the same Helicobacter pylori is present at the site of ulceration. For reliability, as a rule, material is taken from five sections.
FGDS refers to endoscopic research methods, taking a biopsy refers to histological methods. There are also laboratory research methods: a blood test for the presence of specific bodies for Helicobacter pylori. It is given once in a lifetime and cannot serve as a control during treatment. There is also a breath test for the presence of Helicobacter pylori; if there are prerequisites, a blood test is prescribed on the gastropanel. They may prescribe a stool test for occult blood and an ultrasound of internal organs - gastritis also involves nearby organs, such as the pancreas.

© Pixabay
Just about health: how to understand what causes a headache
Also, in case of unclear etiologies, additional tests are performed to exclude helminthic infestations (ascorids, giardia).
How is gastritis treated?
Depending on the etiology and form of gastritis, treatment is prescribed.
For infectious gastritis, the main treatment is aimed at the destruction (eradication) of Helicobacter pylori. It includes several components: an antacid drug, two antibiotics, an antimicrobial drug and a bismuth drug.
With chronic gastritis, a person should visit a doctor and undergo examination at least once a year.
For atrophic gastritis with intestinal epithelial metaplasia - at least 2 times a year with mandatory endoscopic monitoring.
Is the diagnosis of gastritis a death sentence?
The epithelium of the mucous membrane and glands of the stomach are renewed quite quickly, and it is not difficult to normalize the condition of the mucous membrane. But with proper nutrition and lifestyle.
Often people do not want to change their psychological attitudes (nervousness, stress), give up bad habits (alcohol, smoking), or maintain food hygiene, so the illness remains with them forever... If you manage to change yourself, you can say goodbye to the diagnosis.
An exception is atrophic gastritis, an autoimmune gastritis in which the death of mucosal cells occurs. All that can really be achieved in this case with the help of treatment is to prevent the degeneration of areas with atrophied cells into a malignant tumor.
Gastritis is largely a disease of poor nutrition. To avoid problems, children must be taught from childhood to eat proper food and to accept it culturally.
Treatment of gastritis and stomach ulcers with drugs
After making a final diagnosis, the doctor draws up an action plan that includes diet, medication and alternative methods. Treatment of gastritis and ulcers involves an integrated approach. This promotes rapid recovery and reduces the likelihood of disease recurrence. The protocol helps the specialist to navigate and prescribe the optimal treatment for the patient. The treatment regimen for gastritis and stomach ulcers is practically the same; the drugs are suitable in both cases. The list is presented by the following groups:
- Antibacterial substances – for step-by-step therapy to eradicate Helicobacter pylori.
- Proton pump blockers - which reduce the secretion of hydrochloric acid.
- Antagonists of H2-histamine receptors.
- Antacids - in order to reduce the aggressive effect of gastric juice on the mucous membrane.
- Bismuth preparations are an antiulcer medicine that can create a protective film and have a bactericidal and cytoprotective effect.
- Antispasmodics – eliminate spasms and reduce pain.
- Alginates – prevent the development of reflux due to a gel barrier on the surface of the mucosa.
Attention!
The tactics of the gastroenterologist is to prescribe medications to reduce acidity and antibiotics at the same time, based on the data obtained after examining the patient.
Antibiotics for gastritis and stomach ulcers
The main drugs used to treat pathology are antibacterial agents. This approach is necessary to destroy Helicobacter pylori, a bacterium that causes inflammation in the digestive tract. The scheme provides for stepwise therapy; the list of medications is presented in Table 3.
Additionally, other drugs are used to eradicate the bacteria. The duration of therapy is from 10 to 14 days.
Table 3. Groups of antibiotics used for gastritis and ulcers
| Group | Drug name |
| Penicillins | Amoxicillin 1000 mg 2 times a day |
| Macrolides | Clarithromycin, Fromilid, Klacid 500 mg 2 times a day |
| Imidazole derivatives | Metronidazole, Trichopolum, Tinidazole 500 mg 2 times a day |
| Tetracyclines | Tetracycline 500 mg 4 times a day |
| Fluoroquinolones | Levofloxacin 500 mg once daily |
| Rifampicin group | Rifabutin 300 mg once daily |
The combination drug Pilobact Neo is presented on the pharmaceutical market. Each package contains three first-line substances for the treatment of gastritis and ulcers. For most patients, this is the best medicine for ease of use and cost benefits.
Painkillers for gastritis and stomach ulcers
Along with antibacterial substances, additional drugs are prescribed that eliminate hypersecretion and reduce discomfort. Excess hydrochloric acid irritates the mucous membrane, which is manifested by pain and heartburn. Auxiliary therapy is aimed at pain relief for gastritis and gastric ulcers. The following medications are used for these purposes.
Table 4. Drugs used to relieve pain from ulcers and gastritis
| Groups of medications | Name |
| Proton pump blockers | Omeprazole, Omez, Nolpaza 40-80 mg per day in 2 divided doses |
| Histamine H2 receptor antagonists | Ranitidine, Famotidine 1 tablet 2 times a day |
| Bismuth preparations | De-nol, bismuth subcitrate 120 mg 4 times a day |
| Antacids | Phosphalugel, Maalox (liquid forms) 2-3 packets per day, but no more than 6; Sucralfate – tablets 1 piece 4 times a day |
| Antispasmodics | No-spa, Riabal, Dicetel 1 tablet 2-3 times a day |
Carefully! Antipyretics and traditional painkillers (Analgin, Paracetamol, Solpadeine) are not used to eliminate pain. Because they are non-steroidal anti-inflammatory drugs and can increase the production of hydrochloric acid.
Diet and features of therapeutic nutrition
The success of treatment largely depends on proper diet. The diet for gastritis and stomach ulcers is aimed at reducing the irritating effect of food. The frequency of meals is increased to 5-6 times a day. In the acute stage of the disease, products must be consumed after heat treatment. You can boil, bake or steam food. You need to eat regularly and avoid fasting. What you can eat and what you can’t eat is shown in Table 5.
Table 5. Allowed and prohibited foods for gastritis and stomach ulcers
| Allowed | Limit or exclude |
| Lean meat products (beef, pork, chicken breast) | Fatty meats, lard; By-products (skin, cartilage, liver) |
| Lean fish pelengas, pike perch, perch | Fatty fish mackerel, salmon, belan |
| Milk porridge | Bean dishes |
| Fruits and vegetables (neutral) bananas, peaches, pumpkin, potatoes, beets, carrots | Fruits and vegetables (sour) apples, berries, plums, tomatoes, white cabbage, radish, turnip, garlic |
| Spices cinnamon, ginger, thyme, curry, turmeric | Spices hot red and black pepper |
| Low-fat milk, yogurt, non-sour cottage cheese, hard cheeses | Dairy with a high percentage of fat content cream, fermented baked milk, fatty cheeses, kefir |
| Vegetable soups | Sour borsch; meat, mushroom, fish broth |
| Compotes, jelly | Sour fruit juices, fresh juices, carbonated drinks, coffee |
| Unfortunate bread | Baking with yeast |
The list of products for inflammatory diseases of the stomach corresponds to diet No. 5.
What foods are good for the stomach?
Folk remedies
Along with medication, alternative prescriptions are used. In most cases, folk remedies for gastritis and stomach ulcers contain substances of plant origin. Non-traditional methods practically do not cause any side reactions or complications. Therefore, they remain widely in demand among patients. The most famous medicinal products based on natural ingredients are presented in Table 6.
Table 6. Folk remedies for the treatment of gastritis and ulcers
| Folk remedy | Mode of application |
| Water-based propolis elixir | Ready-made extract of beekeeping products – 7-10 drops of liquid 3 times a day 30 minutes before meals |
| Infusion of cinquefoil | 1 tablespoon of crushed raw materials is poured into 200 ml of boiling water in a thermos. Leave for 2 hours. Drink 1/3 cup of tea 1 hour before meals |
| Sea buckthorn with honey | Brew 3 tablespoons of berries in a glass of boiling water, strain, add 3 tablespoons of honey. Take 1 teaspoon on an empty stomach |
| Infusion of yarrow and buckthorn | A mixture of equal parts of herbs is poured into 1 liter of boiling water. Leave for 2 hours. Drink 1 glass in the morning on an empty stomach |
| Licorice root infusion | 2 teaspoons of crushed root are poured into 1 liter of boiling water. Leave for 24 hours and filter. Take 100 ml 3 times a day before meals |
| A mixture of chamomile, yarrow and celandine | Dry grass is poured with 1 liter of boiled milk and infused in an enamel bowl for 2 hours. Take small sips throughout the day |
How to drink potato juice for gastritis
Modifications: 1A and 1B
Diet table No. 1 has two modifications: No. 1A and 1B. For table No. 1A, all dishes are prepared in liquid and porridge form or in the form of mashed puree. It is recommended to eat 6-7 times a day, while vegetables in any form, as well as fruits and bread are strictly prohibited. Such a strict diet is prescribed in the first two weeks of exacerbation of a peptic ulcer, acute or chronic gastritis, as well as a week after gastric surgery.
Table 1B differs from table 1A in the ratio of proteins, fats and carbohydrates and calorie content. Dishes are also prepared in liquid or porridge form, and you need to eat 5-6 times; vegetables, fruits and bread are prohibited. Table No. 1B is prescribed after completion of the course of treatment using table No. 1A.
Prevention of gastritis and stomach ulcers
Prevention of relapse of the disease is the main task of the gastroenterologist. Prevention of gastritis and ulcers includes a number of measures aimed at restoring the full function of the digestive organs and eliminating unpleasant symptoms. The main stages of patient rehabilitation can be noted:
- Elimination of provoking factors.
- Proper nutrition.
- Taking medications to prevent exacerbations.
- Phytotherapy.
- Physiotherapy.
- Spa treatment.
Secondary prevention includes taking medications that restore the functioning of the gastrointestinal tract and promote tissue healing. Unlike the acute stage, antibacterial substances are not used during remission. Recommended medications are presented in Table 7.
Table 7. Drugs for the prevention of exacerbation of ulcers and gastritis
| Means | Therapeutic effect |
| Histamine receptor blockers – Ranitidine, Kvamatel | They exhibit antisecretory effects. Prescribed for a long period of 2 to 5 years at half the therapeutic dose |
| Cytoprotectors – Methyluracil, Potassium orotate, Solcoseryl | Do they have a clamp? Previous article Is it possible to eat baked meat if you have an ulcer... Next article Treatment of duodenal ulcers: medications how to take Advice for every day “Exclude tablets from the diet whose purpose you are not sure of.” Page visited today 71 times TOP 5 authors
|
Causes of the disease
Gastritis develops under the influence of factors either external or internal. Exogenous causes include overeating, eating poor quality food, consuming very fatty and spicy foods, alcoholic beverages, and so on.
When preventing chronic gastritis, first of all, it is worth remembering the rules that even a healthy person must follow. The inflammatory process in the mucous membrane is often provoked by poor chewing of food.
Everyone knows the expression “fill your stomach.” And especially the uncomfortable sensations that come after a hasty, fast meal. Tibetan lamas may not be concerned about the treatment and prevention of gastritis, but for some reason their philosophy is based on rules, following which one can hardly experience the symptoms of gastrointestinal diseases. They chew even liquid food. This is probably the secret of the long youth and longevity of the Tibetan sages.









