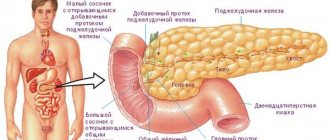
Parenchymal pancreatitis is a pathological change in the parenchyma of the pancreas, when the cells of the glandular tissue of the organ degenerate into fibrous tissue. The disease is accompanied by shrinkage of the ducts and the formation of multiple stones. From the acute form, the disease quickly turns into a chronic type of inflammatory process. The code according to ICD 10 is K86.
Parenchymal pancreatitis is a pathological change in the parenchyma of the pancreas, when the cells of the glandular tissue of the organ degenerate into fibrous tissue.
Causes
Pancreatitis of the parenchymal type occurs due to congenital pathologies of the structure and development of the pancreas and bile ducts (biliary-dependent type of disease), as well as due to the influence of external and internal factors that negatively affect the condition and functioning of the organ. Factors provoking parenchymal pancreatitis:
- chronic diseases of the digestive system;
- improper diet, regular consumption of too fatty foods;
- cystic fibrosis;
- improper functioning of the pancreatic sphincters, resulting in pathologies characterized by exocrine insufficiency;
- autoimmune diseases;
- penetration of pathogenic viruses, bacteria and pathogenic infections into the digestive tract;
- mechanical trauma to pancreatic tissue;
- previous surgical interventions on the organ;
- long-term use of medications (diuretics, estrogens);
- excessive intake of alcohol and alcohol-containing drinks;
- poisoning with heavy metals and their compounds, poisons (arsenic, mercury);
- hypercalcemia occurring in a stable form.

Pathology can develop due to the presence of gallstones if a person does not undergo treatment for a long period of time. Stones lead to blockage of the bile ducts, which is why multiple inflammatory processes begin to form in the digestive tract, including in the tissues of the pancreas (this is how biliary pancreatitis develops).
There is a hereditary factor. If one of the parents had parenchymal pancreatitis, the risk of the disease in the child increases. The likelihood of pathology is especially high with systematic poor nutrition or previous intestinal infections.
Why does fever occur with pancreatitis?
What are the symptoms of cholecystopancreatitis?
What is pancreatic necrosis? Read here.
Symptoms
Pancreatitis begins to develop slowly. In the early stages of the formation of the inflammatory process, there is no clear symptomatic picture, which is why a person does not pay attention to changes in the functioning of the gastrointestinal tract for a long time, and making a correct diagnosis can be difficult.

Nausea is the main sign of parenchymal inflammation.
Pancreatitis is often detected at the stage when the disease has provoked a number of complications, in particular diabetes mellitus. The main signs of inflammation of the organ parenchyma:
- frequent attacks of nausea;
- prolonged and profuse vomiting, after which the person does not experience proper relief;
- eating disorders, for example, aversion to fatty foods, a constant feeling of hunger (always accompanies parenchymal pancreatitis);
- bloating;
- in the abdomen (the symptom spreads to the left side under the ribs, extends to the lumbar region);
- bowel dysfunction: frequent constipation is replaced by prolonged diarrhea (this symptom appears first when pancreatitis begins to develop);
- rapid loss of body weight resulting from lack of appetite (due to frequent abdominal pain and persistent discomfort).
In addition to the symptomatic picture, indicating disturbances in the functioning of the organs of the digestive system, a person has general signs that are evidence of an ongoing pathological process in the body:
- the skin becomes pale, yellowness often appears, which is especially evident on the face;
- the patient feels depressed, constantly wants to sleep, gets tired quickly with little physical activity;
- Reddish spots appear on the skin of the abdomen.
General signs are characteristic mainly during the period of exacerbation of the disease.
When the form of inflammation is chronic, during the period of remission a person is bothered by frequent attacks of nausea after eating and dull, aching pain in the abdomen.
Manifestations of the disease
Chronic parenchymal pancreatitis manifests itself only during exacerbations. The rest of the time it is characterized by a sparse symptomatic picture and almost always normal levels of pancreatic enzymes in the blood.
During the height of the disease, intense abdominal pain appears, often of a girdling nature and intensifying after eating. Pain syndrome occurs as a result of the aggressive action of its own proteolytic enzymes and stretching of the gland capsule due to its increase in size.

Pain syndrome with pancreatitis
A constant symptom of parenchymal pancreatitis is nausea, which worsens after exercise and eating rough food. In addition, the disease is often accompanied by vomiting, which brings relief.
If pancreatitis occurs with exocrine pancreatic insufficiency, then frequent loose stools mixed with pieces of undigested food appear. This indicates a deficiency of enzymes that break down fiber, proteins and fats and is called malabsorption syndrome.
Dyspeptic disorders (heartburn, belching) are not typical for chronic damage to the gland and usually refer to manifestations of concomitant pathology of the digestive tract.
Frequent vomiting and loose stools over time lead to dehydration and weight loss. The patient becomes lethargic, the skin becomes pale, and lethargy and weakness appear.
The severity of the exacerbation directly depends on the general condition of the patient’s body and the prevalence of the pathological process.
We recommend reading: Is X-ray harmful: why is it dangerous for health, harm to the body
Upon palpation, the doctor detects an enlarged and sharply painful gland (pain is especially pronounced in the Shoffard area and the Mayo-Robson point). Possible bloating and tympanitis on percussion. The skin is pale and dry, the tongue is thickly coated with white coating, and a sharp sour odor emanates from the mouth.
Diagnosis of parenchymal pancreatitis
To determine the disease, its form and stage of development, a series of laboratory tests and instrumental diagnostic techniques are prescribed:
- The main method is x-ray. Often the procedure is performed simultaneously with angiography using a contrast agent. X-ray shows an increase in the volume of the head of the pancreas and a change in the condition of the duodenal loop. Angiography is used to determine the exact location of inflammation.
- Ultrasound scanning.
- MRI and CT are performed only in cases where there is a suspicion of complications (cancer, cholecystitis).
- To determine the density of the organ parenchyma, an ultrasound examination is performed.
Analyzes
The main laboratory tests that help determine the stage of pancreatitis are blood and urine. Blood shows elevated ESR levels. A urine test is necessary to determine a complication such as diabetes. The disease often occurs in the early stages of pancreatic inflammation.
A coprogram (stool analysis) is carried out to detect undigested food particles, which is evidence of dysfunction of the digestive system.
If pancreatitis occurs in a protracted, severe form, digestive enzymes are taken to study their concentration.
Treatment
When the first signs of the disease appear, you should go to see a doctor. If the pathological process is detected in a timely manner, pancreatitis can be cured through conservative therapy. It is important to understand that cure means a state of remission, because It is not possible to completely cure this type of pancreatitis.

When the first signs of the disease appear, you should go to see a doctor.
In the absence of positive dynamics from conservative therapy, or in cases where pancreatitis has provoked severe complications, and there is no way to stop the further development of the pathological process, the only method of normalizing the condition and functioning of the organ is surgical intervention.
Depending on the severity of the clinical case and the condition of the body, the operation involves partial or complete resection of the pancreas, removal of the gallbladder or stones from it. Parenchymal pancreatitis is often treated by surgery to install drainage, puncture or sphincterotomy (dissection of the sphincter muscles).
Drug therapy
During therapy, enzyme preparations are prescribed, which contain active substances secreted by the pancreas.
Pancreatitis is treated with Pancreatin.
Pancreatitis is treated with the following means:
- Creon;
- Festal;
- Pancreatin.
These medications help the pancreas function, relieving it of most of the load.
To prevent further spread of inflammation, the following are prescribed:
- Potassium Orotate;
- Cobamamide;
- Methyluracil.
These medications must be taken over a long period of time.
Diet
It is not possible to cure parenchymal pancreatitis without adjusting the diet. The therapeutic diet should always be followed by patients so that the disease remains in a stage of prolonged remission for as long as possible. List of products prohibited for consumption:
- spices, herbs, any spicy food;
- fatty meat and fish;
- marinades, pickles;
- smoked meats;
- carbonated and alcohol-containing drinks, alcohol;
- coffee, cocoa and strong tea.
Fruits, flour and confectionery products are allowed rarely and in limited quantities. Avoid foods prepared by frying.

It is not possible to cure parenchymal pancreatitis without adjusting the diet.
The basis of the diet is porridge and lean broths, lean meats and fish, steamed vegetables, baked fruits. All products must be crushed to a porridge state. Only during the period of remission is a slight relaxation, expansion of the diet, and consumption of foods in pieces allowed.
Proper consumption of food is important: you need to eat fractionally, up to 8 times a day, but in small portions.
Structure
The parenchymal organ is dense and compact and consists of stroma and parenchyma.
The main part of the organ consists of it - many cells that perform basic functions. The consistency is soft.
Main distinctive features:
- A large amount of fleshy substance.
- Large but compact look.
- Not round, but elongated, slightly flattened.
- The presence of a large number of excretory ducts secreting secretions.
- The presence of a serous membrane that holds the parenchyma and gives the organ its shape.
Stroma also has a translation from Greek - “litter”.
The stroma supports the organ, forming, protecting, supporting and feeding it with necessary substances. A network of blood vessels and nerve endings runs along this membrane. It is not only located on top, but also grows inside the organ. In medicine, such partitions are called trabeculae.
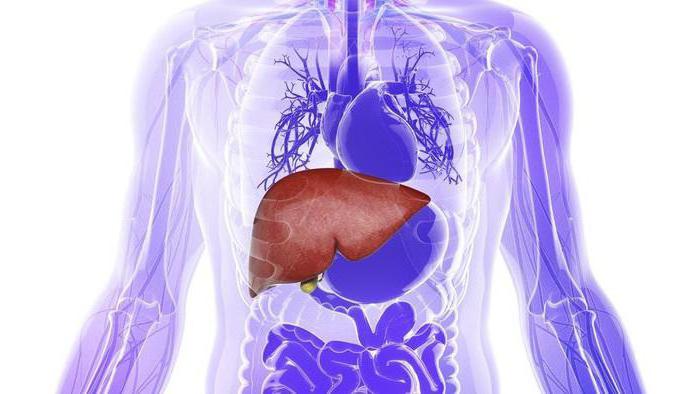
Complications
Parenchymal pancreatitis rarely occurs without complications. Improper production of enzymes, poor digestion of food and blockage of the bile ducts lead to a total disruption of the digestive process. The pathological process begins to gradually cover the entire parenchyma, leading to irreversible changes in the pancreas and spreading to neighboring internal organs.
Cancer
In the absence of timely treatment, pancreatitis leads to the formation of an oncological neoplasm in the tissues of the organ.

In the absence of metastases to neighboring organs, the disease is treated by removing the pancreas.
In the absence of metastases to neighboring organs, the disease is treated by removing the pancreas and administering chemotherapy. If metastases have already started, therapy is prescribed to stop their further spread.
Inflammation of the parenchyma
When inflammation spreads throughout the parenchyma, pancreatitis leads to complete atrophy of the pancreas. The organ stops working. The treatment method is removal of the gland.
Diabetes
The most common complication that occurs quite quickly. The reason is a violation of the digestion process of food, dysfunction of the bile ducts. Treatment: medication, aimed at normalizing and maintaining blood glucose levels, strict adherence to diet.

Diabetes mellitus is the most common complication that occurs quite quickly.
Gastric erosion
Pancreatitis provokes the reflux of pancreatic enzymes into the stomach, which leads to irritation of its mucous membrane and the formation of erosion in it. The disease is characterized by a painful symptomatic picture. Treatment: symptomatic; therapy is required to normalize the functioning of the pancreas.
The role of hormones for men
- FLG promotes testosterone production and affects sperm maturation.
- LH regulates the production of testosterone by Leydig cells and takes part in the production of proteins that bind sex hormones. Improves the permeability of the testes.
- Testosterone is responsible for the development of secondary sexual characteristics and the formation of the skeleton and muscle development. Normalizes the emotional state and regulates the functioning of the sebaceous glands.
- Prolactin regulates water-salt balance and stimulates the high-quality maturation of sperm.
- SHBG is a glycoprotein that takes part in the distribution of sex hormones.
Reviews
Oksana, 55 years old, Novosibirsk: “Parenchymal pancreatitis was discovered by accident. It’s good that I saw a doctor on time, so I avoided surgery. She was treated with medications containing pancreatic enzymes and followed a diet. The doctor said that now the diet is permanent, or there will be an exacerbation.”
Marina, 44 years old, Saratov: “I went to the doctor when pain and nausea appeared. Pancreatitis of the parenchymal type was determined. There was an operation (partial removal of the pancreas). Now I have to take a course of pills frequently to prevent a relapse.”
Sergey, 56 years old, Chita: “My pancreatitis was caused by diabetes. Now I'm on pills and a diet. It’s good that they didn’t schedule surgery. Now every six months I go for examinations, the doctors said that if there is a deterioration, they will remove the gland.”