Causes of discomfort
The pancreas can hurt due to various ailments. Discomfort and pain are often caused by the development of pancreatitis, an inflammatory process in the gland. The acute form of pancreatitis is especially pronounced.
Factors contributing to the development of pathology may include:
- chronic inflammatory processes in nearby structures (stomach, gall bladder),
- bile stagnation,
- poor nutrition, abuse of foods that overload the pancreas,
- taking medications that interfere with the enzymatic function of the gland,
- alcoholism,
- autoimmune processes,
- abdominal trauma,
- stress,
- poisoning.
In addition to pancreatitis, pain in the pancreas can be caused by the following diseases:
- cancer,
- cystic fibrosis,
- cyst,
- insulinoma,
- pancreatic necrosis.
Sometimes the source of pain is not the pancreas. Often people suffering from chronic pancreatitis attribute any abdominal pain to this disease. But before starting treatment, you need to make sure that the pain syndrome comes from this organ.
What does a blood test for glycated hemoglobin mean and how to prepare for the test?
We have the answer! Find out how a puncture of the mammary gland is performed and what the diagnostic results show in this article.
Pain may also be caused by:
- cholelithiasis,
- biliary dyskinesia,
- stomach and duodenal ulcers,
- cholecystitis,
- gastritis,
- intestinal infection.
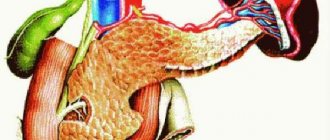
Pancreas - structure and main functions
Pain in the pancreas brings severe torment
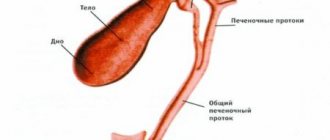
The pancreas is an organ of the digestive system located behind the stomach on the back wall of the abdomen. It is characterized by a peculiar shape, has a head, body and tail. The length of the pancreas is 16-22 cm, and it weighs about 80 g.
The pancreas has an alveolar-tubular structure. It is divided into grayish-pink lobules, each of which consists of glandular tissue and has its own system of excretory ducts. These small excretory ducts are connected to larger ones, which, in turn, are combined into a common excretory duct. The common excretory duct runs along the entire length of the organ and opens into the duodenum.
The lobules of the gland are formed from cells that produce pancreatic juice, rich in digestive enzymes. From the lobules, the secretion enters the duodenum through a common duct running along the entire gland. Between the lobules of the gland are groups of glandular cells, the so-called islets of Langerhans. These clusters of cells do not have excretory ducts; they produce insulin and glucagon directly into the blood. The pancreas is a gland of mixed type of secretion, that is, it performs both endocrine and exocrine actions:
- The exocrine function is to participate in digestion. The gland produces pancreatic juice and carries it through the ducts into the duodenum. Every day, about 500-700 ml of juice is produced, which contains the enzymes necessary for digesting food - amylase, which helps convert starch into sugar; trypsin and chymotrypsin are enzymes responsible for protein breakdown; lipase, responsible for the breakdown of fat, etc. Thus, pancreatic juice is an important digestive juice necessary for the digestion of organic components of food.
- The endocrine function of the gland is to secrete glucagon and insulin, hormones involved in the regulation of carbohydrate metabolism.
The pancreas is in close relationship with other organs of the digestive tract. Any pathological process affecting it negatively affects digestion. Without the enzymes it produces, normal breakdown of food is impossible, and without the hormones glucagon and insulin, regulation of metabolic processes in the body is impossible.
Nature of pain in the pancreas
The organ has an elongated shape. Therefore, depending on the localization of the pathological process, the resulting pain syndrome can be felt in different places. That is why doubts often arise about which organ is hurting.
Pain syndromes characteristic of the pancreas:
- Chukhrienko occurs if you press the edge of your palm with a jerky movement on the epigastrium,
- Mayo-Robson pain when pressing on the left costovertebral angle,
- Dudkevich appears when pressing 2 cm below the navel inward and obliquely upward.
Inflammation of the pancreas is often accompanied by girdles and severe pain. Its nature depends on the extent of organ damage. As a rule, pain is localized in the epigastrium and can be scattered throughout the peritoneum. When the tail or body of the pancreas is affected, it is concentrated in the upper and central part of the abdomen, and can radiate to the lower back and hypochondrium on the left. If the head of the organ is affected in the center of the upper abdomen or right hypochondrium. When the entire organ is inflamed, the pain is girdling in nature.
Tissue swelling that occurs against the background of inflammation leads to compression of nerve endings and overcrowding of the ducts with gland secretions, which causes pain.
Acute pancreatitis
Pain occurs after eating heavy food, alcoholic beverages, or overeating:
- Accompanied by fever, dyspeptic disorders (nausea, vomiting, diarrhea).
- It intensifies when pressing on the navel, during coughing, and body movements.
- The pain in acute pancreatitis subsides only in a sitting position, with a slight bend forward.
Chronic pancreatitis
The intensity and nature of pain may vary depending on the stage of the disease (exacerbation or remission). When the acute inflammatory process subsides, the pain dulls, occurs less frequently and after a while may disappear altogether.
The localization of pain in chronic pancreatitis is typical for the epigastric region, but often it radiates to the right hypochondrium, the lumbar spine. The painful sensations are aching, dull in nature. Increased pain occurs with overeating, eating fatty and fried foods, and physical activity. If the disease is not treated, the symptoms will periodically fade and worsen over several weeks or months. The intensity of pain depends on the extent of damage to the pancreas.
Other organ pathologies
Like pancreatitis, most other diseases of the organ are accompanied by pain of a different nature, depending on the stage of development of the pathology.
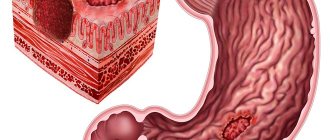
Pancreatic cancer may not manifest itself in the early stages. Sometimes, if the diet is disrupted, nausea and fatty stools may occur. Depending on the location of the tumor and the stage of the cancer, pain can be either episodic or constant. An increase in size of the formation leads to its germination into surrounding tissues. As a result, the nerve fibers are pinched and sharp, throbbing pain occurs. A person may assume a hooked position due to discomfort in the abdomen.
The cyst may not produce symptoms for a long time. As it grows, dull, mild pain may appear from time to time. The large size of the cyst, squeezing neighboring tissues and stretching the pancreatic capsule, causes severe pain. If the cyst is located in the head of the organ, the pain covers the right epigastrium, in the tail the left part.
Pancreatic necrosis is a disease that occurs with pronounced pain in the epigastrium or retrosternal region, radiating to the back and collarbone. Sometimes a person may lose consciousness from painful shock.
Preventive measures for pancreatic disease
Healthy food
A set of preventive measures against pancreatic disease is aimed at improving the quality of life, nutrition, and creating a healthy lifestyle. You should avoid taking alcoholic beverages, tobacco, and aggressive foods (salt, acid, smoked foods, fats). It is important to maintain moderation when eating, as overeating can contribute to the development of the disease. The patient needs systematic physical activity and walks in the fresh air. It will not be superfluous to maintain emotional balance and peace of mind, since depression and stress only provoke the course of the disease. Herbal medicine with chamomile, lingonberries, blueberries, rosehips and other useful herbal preparations should be carried out regularly. It is good if the patient eats about five times a day in small portions. This diet will allow the stomach to rest from time to time after work. Diseases and visits to doctors cannot be ignored, because only under their constant guidance can the disease be diagnosed and immediate treatment begin.
Diagnostics
If pain occurs in the abdominal cavity, you should immediately seek help from a specialist so as not to miss the progression of life-threatening conditions. It is important to carry out a differential diagnosis of pancreatic diseases with lesions of other organs.
The doctor interviews the patient and palpates the painful area in different positions (lying on his back, on his side). Laboratory studies involve measuring the level of pancreatic (amylase, trypsin, lipase) and liver enzymes (ALT, bilirubin, phosphatase). Stool is examined for the determination of trypsin, chymotrypsin, and lipids. To identify a carbohydrate metabolism disorder, the patient must donate blood for sugar.
Instrumental diagnostic methods:
- Ultrasound of the gland and abdominal organs,
- CT, MRI,
- radiography.
Ways to eliminate pain
The tactics for eliminating pancreatic pain will be based on the diagnostic results and the causes of the pathological condition. In case of exacerbation of pancreatitis, first of all, it is necessary to provide the patient with rest and complete abstinence from food for the first 2-3 days, until the acute pain subsides. It is allowed to drink alkaline water and rosehip decoction. Treatment of acute inflammation is best done in a hospital.
On a note! You can alleviate the condition by taking a knee-elbow position and applying cold to the abdominal area. It is advisable to move less.
Medications
Antispasmodics are used to relieve pain:
- No-shpa,
- Baralgin,
- Drotaverine.
If the pain is severe, you may need to use more powerful medications:
- Tramadol,
- Morphine.
To prevent irritation of the mucous membranes of the gastrointestinal tract, neutralize the effect of hydrochloric acid, and reduce enzymatic activity in the initial stages of the inflammatory process, it is recommended to take antacids (Almagel), H2-blockers (Ranitidine, Zoran), proton pump inhibitors (Omez, Otsid).
After the acute attack has stopped, enzyme therapy for the pancreas is prescribed.
In order to improve the functionality of the pancreas and improve digestion, it is recommended to take with meals:
- Festal,
- Mezim,
- Creon.
In some cases, it is necessary to resort to surgery on the pancreas. The indications are:
- blockage of ducts,
- gland cyst,
- pancreatic cancer,
- insulinoma,
- stones in the gland or gall bladder,
- pancreatic necrosis.
What is acute pancreatitis?
Acute pancreatitis is a complex disease that is not always easy to diagnose. Acute inflammation can take various forms. The severity of acute pancreatitis can be determined as follows:
- interstitial – acute pancreatic edema. It proceeds quickly and in a relatively mild form. Conservative treatment
- necrotic - leads to death of pancreatic tissue. The disease is severe. Patients experience severe pain, frequent vomiting, and skin color changes. Long-term treatment
- purulent - occurs as a result of changes in the integrity of the pancreas: vessels, ducts of glandular tissue. High risk of mortality.
Lost time leads to severe forms of the disease with pancreatitis. In addition, “concomitant” diseases may develop, because the pancreas has a serious impact on the processes of food digestion in the intestines. The lack of enzymes does not allow the body to process foods conscientiously.
The hormones produced by the pancreas, insulin and glucagon, regulate the biochemical changes that occur in the cells of the human body. Therefore, at the first symptoms of the disease, you should not resort to self-medication, but you should urgently consult a doctor.