The prescription of antibiotics for pancreatitis is associated with a combination of inflammation caused by the release of excess enzymes that melt the tissue with an associated infection from the intestines and gallbladder.
In this case, the risk of infection increases significantly and pancreatitis is complicated by a septic condition, peritonitis, retroperitoneal abscess or phlegmon. Severe inflammation of the pancreas is observed in every fifth case. Only a doctor can determine which drug should be taken in a particular case.
When are antimicrobials appropriate?
Antibacterial drugs should be treated with due attention due to possible side effects and inhibition of intestinal flora. Therefore, there must be clear indications for prescribing antibiotics. These include:
- obtaining, during examination, indisputable data on the inflammatory process in glandular tissues, neighboring organs (cholecystitis), and intestines;
- bile stagnation, dyskinesia of the gallbladder and ducts;
- the risk of spreading infection and bacterial complications, which increases in the presence of cholangitis, cysts in the body of the gland, pancreatic necrosis;
- suspicion of rupture of the main duct in the glandular tissue;
- the appearance of signs of peripancreatitis (inflammation in surrounding tissues).
Currently, it is prohibited to use antibiotics for prophylactic purposes.
The pancreas is connected by blood circulation to neighboring organs; the infection can spread by contact along the common duct, bile ducts
Advantages and disadvantages of antibiotics
The selection of antibiotics requires knowledge of the mechanism of action. It is impossible to suppress pathogenic flora with other drugs. Lost time will lead a patient with acute pancreatitis to necrosis and death from severe intoxication, which is almost impossible to cope with with other medications.
Negative manifestations include:
- the possibility of developing hypersensitivity with allergic manifestations (skin rash, itching, swelling of the face, runny nose, asthma attack);
- toxic effect on the liver and kidneys when the dosage is exceeded, while the patient is taking alcoholic beverages;
- undesirable enhancement of the effect of other medications that the patient is taking (for example, blood thinners);
- dizziness, nausea, hearing impairment are often caused by the effect of antibiotics on the vestibular apparatus of the brain;
- An imbalance in the intestinal flora leads to the need to take probiotics and prebiotics after a course of antibiotics to restore digestion.
Antibiotics are a special type of medicine. They are obtained from natural or synthetic raw materials. Act on living microorganisms. Different classes differ in the mechanism of influence. The most powerful agents kill pathogenic microbes.
Others disrupt metabolism, the construction of cell membranes, and thereby disorganize metabolism to such an extent that they create conditions unacceptable for the life of the microbe.
Unfortunately, drugs can also affect the necessary microflora, cells of the nervous system, liver, and kidneys. Toxic substances hinder the functioning of human internal organs, cause poisoning and require additional cleansing of the body.
The disadvantages of antibiotic treatment include the possibility of causing resistance in pathogenic flora. Rather, this is a matter of microorganisms becoming accustomed, but as a result, entire classes of possible drugs are lost. The problem of resistance is being studied by scientists around the world.
Like other medications, antibiotics have the potential to cause an allergic reaction in an individual patient. With a high frequency of allergenicity, drugs are excluded from practice.

Before using an antibiotic, it is necessary to perform a sensitivity test to prevent possible allergies.
Possible side effects
The antibiotic is usually well tolerated by patients at any age, so side effects occur in rare cases. Individually, with long-term use of the drug, the patient may experience nausea, diarrhea, and pain in the abdominal cavity. This is due to the fact that the medicine not only effectively fights pathogenic bacteria, but also disrupts the intestinal microflora. To restore normal microflora after taking Amoxiclav for pancreatitis, it is recommended to take probiotics.
When using the drug, fungal growths may occur on the skin, mucous membranes and oral cavity. Women may develop thrush. Also, like any other medical product, an allergy may occur to the drug. It can manifest itself as skin rashes, urticaria, and dermatitis. In this case, you need to stop taking Amoxiclav for pancreatitis and consult a medical specialist.
source
Rules for the use of antibiotics
Treatment of pancreatitis with antibiotics is carried out in accordance with the general rules of therapy. If there is no data on the microorganisms that caused the inflammatory process, broad-spectrum drugs are prescribed. Upon receiving the conclusion of the flora analysis, the most optimally effective antibiotic is used.
Before use, an intradermal test is performed to identify increased sensitivity of the body and prevent an allergic reaction. The dosage is calculated based on the weight and age of the patient.
Antibiotics for pancreatitis in adults and children are prescribed in a course of 7–10 days; by independently shortening or extending the treatment period, patients cause irreparable harm to their body, since sensitivity to the chosen drug is lost.
It is necessary to take into account the compliance of the form of administration with the patient’s condition; in severe cases, only the injection method is recommended (intramuscular and intravenous) due to vomiting, low absorption in the intestine; patients drink tablet medications when their condition improves.
The frequency of doses is due to the need to maintain a constant sufficient therapeutic dosage in the body, so the doctor is guided by data on the rate of accumulation and elimination. The principle of drug interaction, strengthening or opposite direction of influence is taken into account.
Antibiotics that have a high toxic effect on the liver and kidneys are not used. Antibacterial drugs are used in a comprehensive treatment regimen.
The doctor can judge the presence of an infectious complication by the patient’s fever and increased pain.
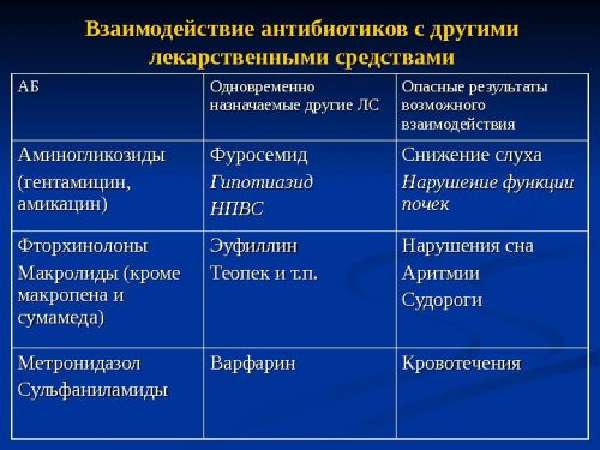
Prescription of several drugs must be monitored for their combined effect
Dosage form
Causes
This type of pancreatitis is rare. It accounts for only 3% of acute cases. Children and people suffering from HIV infection are at risk.
Antibiotics act on the gland. However, it is impossible to say with 100% certainty that the use of a particular drug will lead to the development of an acute course.
The following drugs may be the culprits of the disease:
- antibiotics from the cephalosporin group, as well as metronidazole;
- diuretics;
- antihypertensive drugs;
- proton pump inhibitors;
- antiviral agents for the treatment of HIV infection;
- some other medications.

The above drugs have an autoimmune, direct cytotoxic effect, which determines their ability to damage the pancreas. The development of the disease cannot be predicted. It occurs when taking medications in normal dosages.
Symptoms
Manifestations after taking antibiotics vary and are determined by the severity of the pathology. Usually there is a slight swelling of the organ with insignificant clinical signs, but a necrotic version of the disease often develops. As a rule, the pathology is acute.
The symptoms are similar to the clinical picture of the acute type of the disease. Most often, a person complains that he has pain in the upper segment of the abdomen, the left hypochondrium. The severity of pain varies: from discomfort to intense pain that subsides only with a certain position of the body.

Pain with pancreatitis
Many patients experience symptoms of dyspepsia (nausea, diarrhea, vomiting). Sometimes asthenic manifestations are observed: loss of strength, dizziness, headache.
Symptoms of the disease can occur both during therapy and after its completion, which is due to the accumulation of harmful substances in the body. Some drugs lead to damage several months after their discontinuation, others after a single dose.
In case of acute injury (medicated), the pain is localized in the navel area, but can spread to the stomach area. The pain radiates to the back or lower back. If the patient takes a horizontal position, the discomfort increases.
Due to the consumption of alcoholic beverages and food, the patient's condition usually worsens. There is no relief after vomiting. This distinguishes this symptom of pancreatitis from a similar one that develops against the background of high blood pressure or food poisoning.
If you experience pain or other signs of pancreatitis, you should consult a doctor as soon as possible. To alleviate your condition, you can temporarily stop drinking water and food, and put an ice pack on the area of the body where pain is observed. It is recommended to take a forced position, rising on your knees and elbows. It is best to tuck your knees towards your chest.
Diagnostics
Identifying drug-induced injury is not an easy task. This is due to the fact that the time intervals through which the disease develops vary. In addition, there are no specific signs indicating the nature of inflammation of the pancreas.

The patient must transfer to the gastroenterologist the medications he took before the illness. This will allow the specialist to understand whether the antibiotics have affected the pancreas. It is important to exclude organ damage as a result of alcohol abuse and the presence of cholelithiasis.
Discontinuation of the drug that provoked the development of the inflammatory process leads to an improvement in the condition.
Laboratory diagnostics involves determining the level of C-reactive protein, which in the medicinal form does not increase as much as in an acute form of the disease of a different origin.
If the pathology is of a medicinal nature, then a clinical blood test shows leukocytosis, an increase in the erythrocyte sedimentation rate. Blood biochemistry shows an increase in the amount of amylase, LDH and G-GTP, and sometimes glucose. Signs inherent only to drug-induced pancreatitis are not visible on ultrasound; only general symptoms of the inflammatory process are observed.
We recommend that you read:
- pathology of the head of the pancreas due to drug overdose;
- probiotics after taking antibiotics, especially for adults.
Antibiotics for acute pancreatitis
Pathological changes in acute pancreatitis begin with stagnation of secretions containing powerful enzymes inside the glandular tissue and the development of self-digestion of the organ. In response, immune cells accumulate in the peritoneum, providing aseptic (without the participation of microbes) inflammation to limit the process.
Pancreas examination
But conditionally pathogenic microorganisms (Escherichia coli) located nearby in the intestine, taking advantage of the weakening of their protective properties, turn into serious causative agents of infectious inflammation and complicate the course of pancreatitis.
The human body requires additional efforts to fight, which it does not have. In such a situation, only antibacterial agents can help. Broad-spectrum drugs are used. They are administered intravenously and intraperitoneally.
In an acute process, the effectiveness of treatment and the outcome of the disease largely depend on the initiation of antibiotic treatment. Delayed use threatens the patient's life.
Pharmacological action of the drug

The main effect of the drug is to normalize the intestinal microflora and support the functioning of beneficial bacteria. Thanks to this effect, Linex helps not only to improve the functioning of the intestines, but also to improve the absorption of useful elements by its walls, to activate the digestion of proteins, which has a beneficial effect on the entire body as a whole.
Live lactic acid bacteria, which are contained in Linex, maintain the balance of microflora in all parts of the intestine, contribute to the inhibition of the vital activity of pathogenic microorganisms, improve the absorption of vitamins B, PP, K, E, ascorbic and folic acids, and replenish biotin reserves in the body. Bacteria also produce lactic acid, which contributes to better absorption of iron and calcium.
The beneficial bacteria that make up the medication take part in the breakdown of proteins, carbohydrates, fats, and the metabolism of bile acids.
They help infants digest proteins, which is especially important for lactose intolerance. Thanks to these properties, the drug helps to normalize the processes of digestion and metabolism.
Microorganisms contained in the capsules of the drug produce:
- dairy;
- vinegar;
- propionic acid.
They normalize the acidity of intestinal contents, creating unfavorable conditions for the life and reproduction of pathogenic, conditionally pathogenic bacteria. Thanks to this action, the balance of positive microflora is restored in the intestines.
Thus, the action of lactic acid bacteria contained in Linex leads to the following results:
- Restoration of beneficial intestinal flora.
- Improving the absorption of nutrients from incoming food.
- Activation of the processes of breakdown of proteins, fats, carbohydrates, normalization of digestion and metabolism processes.
- Suppression of the activity of pathogenic bacteria.
Therefore, Linex helps strengthen the immune system, as well as relieve symptoms of dysbacteriosis such as flatulence, bloating, nausea, increased gas formation, and colic.
Cost and release form

The drug is produced in the form of capsules, as well as drops and sachets for children. The manufacturer of the drug is Switzerland, so the drug is not in the budget category.
The cost of a package of 14 capsules is 420-527 rubles, the price of seven Linex Forte capsules is 341 rubles, the cost of 20 children's sachets is 663 rubles, the price of a children's bottle with 8 ml drops. is 590 rub.
Compound
Linex capsules contain white powder. It is a collection of lyophilized lactic acid bacteria, which are the active component of the drug. The following are used as additional substances in the manufacture of the medicine:
- gelatin;
- potato starch;
- lactose;
- magnesium stearate;
- titanium dioxide.
Why are antibiotics needed for chronic pancreatitis?
Chronic pancreatitis is less severe, but each exacerbation is accompanied by increased activity of pathogenic microflora and invades new areas of the pancreas. In this case, the gallbladder, ducts, duodenum, stomach, and liver are involved in the inflammatory process.
The surrounding tissues are the first to be affected (peripancreatitis). In such cases, it is necessary to provide active counteraction to microorganisms.
Drugs are prescribed in the acute stage:
- Ampioks,
- Augmentin,
- Amoxicillin,
- Amoxiclav,
- Levomycetin,
- Cefoperazone,
- Cefuroxime,
- Cefixime.
The effectiveness is judged by the normalization of temperature, absence of pain, and restoration of stool. Before use, it is advisable to isolate the most significant pathogen or mixed microflora by bacteriological method to select the optimal antibiotic. Sowing of bile and gastric juice is carried out. Sensitivity to the drug must be confirmed.

If there is no evidence of infectious inflammation, then there is no point in prescribing antibiotics; treatment is carried out with enzyme and other drugs
Characteristics of the most used antibiotics
The choice of form (tablets or injections) is determined by the severity of the patient’s condition. Other features are taken into account when individually prescribing the drug. For acute inflammation, the most powerful antibiotics are used.
Cefotaxime is a semi-synthetic cephalosporin of the third generation, available only in bottles in powder form for dilution and administration intramuscularly or intravenously, the effect begins after 30 minutes and lasts 12 hours, destroys bacteria by blocking vital enzyme systems, has a negative effect on blood clotting, and is therefore contraindicated with a tendency to bleeding.
Doxycycline - available in tablets, capsules and ampoules, suppresses protein synthesis in bacteria, belongs to the group of tetracyclines, is more active and less damaging to normal intestinal flora, enhances the toxic effect on the liver, therefore is not used for manifestations of liver failure, causes side effects with impaired hearing, vision, nervous system.
Ceftriaxone is available only for injection, like Cefotaxime, it is part of the group of third-generation semisynthetic cephalosporins; among the negative effects, one should take into account the effect on hematopoiesis (synthesis of blood cells), increased deposition of salts in bile, and intestinal inflammation.
Ampiox is available in capsules and vials for injection, the active ingredient is a combination of Ampicillin and Oxacillin, it is part of the group of penicillins, and accordingly has a negative effect on hematopoiesis and enhances the effect of anticoagulants.

In combination with diuretics, the negative properties are more pronounced
All of the listed drugs are contraindicated during pregnancy, lactation, and are not prescribed to small patients. They are used for emergency indications, but after treatment they will require restoration of intestinal digestion.
Among tableted antibiotics used for chronic pancreatitis, they can be considered effective. Azithromycin is a synthetic derivative of Erythromycin that inhibits protein synthesis in various types of bacterial cells. However, it can cause nausea, vomiting, blurred vision, and inhibition of the production of blood lymphocytes in humans. After stopping use, it remains in the patient’s blood for another 5–7 days.
Abactal is a drug that belongs to the group of fluoroquinolones, acts on the DNA of microorganisms, and has a wide spectrum of damage. Prescribed with caution to patients with atherosclerotic lesions of cerebral vessels, previous cerebrovascular accident, epileptic syndrome, renal and liver failure, contraindicated under the age of 18 years, with hemolytic anemia.
Sumamed - the active component of the drug is azithromycin dihydrate, respectively, all properties are preserved and enhanced, it is prescribed to children after 12 years of age, depending on weight, the dosage is carefully selected for patients with arrhythmias, heart failure, myasthenia.
Ciprolet A is a combination of Tinidazole and Ciprofloxacin. Indicated for mixed infection. Prescribed with caution for atherosclerosis of cerebral vessels in the elderly, mental illness, and epilepsy. Contraindicated in acute porphyria, blood diseases, under the age of 18, and pregnant women.