Antibiotics for cholecystitis are the basis of drug therapy for such a disease. This is due to the fact that such a disorder can be caused by the pathological influence of pathogenic bacteria. In addition, the inflammatory process can often be accompanied by blockage of the bile ducts, which leads to accumulation and thickening of bile. It is this condition that leads to an increase in the number of bacteria.
- Effective antibiotics
- Rules of application
- Side effects
Antibiotic therapy is often carried out at the initial stages of acute inflammation of the gallbladder, as well as during exacerbation of the chronic form. The name, duration of the course and dosage are determined by the doctor, but, in most cases, therapy lasts no more than seven days, in rare cases – ten. Otherwise, there is a possibility of developing side effects.
Treatment of cholecystitis with antibiotics is performed with broad-spectrum substances that can destroy a large number of bacteria. In addition, such therapy involves taking vitamin complexes aimed at strengthening the immune system and drugs that prevent the development of intestinal dysbiosis.
In cases of the addition of a secondary infectious process, the elimination of such a disease with antibiotics is carried out by selecting several antibacterial agents at once.
Situations when it is necessary to use antibiotics for inflammation of the gallbladder are:
- increased leukocyte content in the blood;
- an increase in ESR, which confirms the presence of an inflammatory process;
- detection, during instrumental diagnostics, of a significant increase in the volume of the affected organ or liver;
- profuse diarrhea;
- constant nausea, which may result in vomiting;
- increase in temperature indicators;
- periodic but rather intense pain in the right hypochondrium;
- colic in the stomach.
It is worth noting that patients with a similar diagnosis should not take such medications on their own, as this may lead to the development of undesirable consequences.
Before prescribing such drugs to a patient, specialists should find out their susceptibility to the patient’s bile microflora. This is due to the fact that quite a few antibacterial agents may not have any effect on destroying the pathogen.
Indications for taking antibiotics
Antibiotic drugs are indicated for use in the following manifestations of cholecystitis:
- severe increasing pain in the area of the right hypochondrium,
- increase in body temperature to 38-39°C,
- severe digestive disorders accompanied by vomiting and diarrhea,
- pain throughout the abdominal cavity,
- complication of the disease by other processes of an inflammatory or infectious nature,
- signs of infection detected during laboratory blood tests.
How are indications for antibiotics determined?
Indications for the use of antibiotics are clarified starting with questioning and examination of the patient. Usually the patient is concerned about:
- intermittent, but rather intense pain in the hypochondrium on the right;
- colic along the intestines;
- frequent loose stools;
- nausea, possible vomiting;
- temperature increased to more than 38 degrees.
Upon examination, the doctor detects pain in the right hypochondrium, and sometimes palpates an enlarged gallbladder.
Blood tests reveal:
- leukocytosis with a shift of the formula to the left;
- increase in ESR.
The decision on the advisability of using antibiotics, the selection of dosage and route of administration of the medicine is made only by the doctor. We draw attention to the great harm of self-medication.
Antibiotic names
Below is a list of antibiotics that are most often used for cholecystitis:
- Azithromycin is produced in the form of tablets and capsules. Take the drug after meals. The average dosage is about 1 g. in one go.
- Zitrolide is a drug similar to the previous one, available only in capsules. The action is prolonged, i.e. one dose per day will be enough.
- Sumalek is an antibiotic belonging to the macrolide class. Available in powder or tablet form. For treatment, it is enough to take the drug once a day. The duration of the course of treatment is determined by the attending physician.
- Azicar - available in capsule form. The antibiotic has an expanded scope of application. Can cope with a large number of inflammatory processes, including complex and combined ones. Widely used for the treatment of cholecystopancreatitis. Take 1 time during the day after meals. Required dosage – 1 g.
- Amoxil is a compound antibiotic with combined action. The composition contains amoxicillin, qualupanic acid and other components. Antibiotic in the form of tablets and solution. The dosage option (oral or infusion) is chosen by the doctor.
- Flemoxin Solutab is a soluble tablet containing amoxicillin. The drug in the form of a solution acts much faster and more efficiently, and also has almost complete absorption in the gastrointestinal tract. This antibiotic can be prescribed to children from 1 year of age.
Consequences of antibiotic use
Antibiotics for cholecystitis are necessary, but their use in most cases is accompanied by adverse changes in the body:
- intestinal dysbiosis develops due to the death of its own beneficial microflora, accompanied by dyspeptic disorders and decreased immunity;
- oral, intestinal, vaginal candidiasis - the result of excessive proliferation of an opportunistic fungus due to dysbacteriosis and decreased immunity;
- Allergy is a common occurrence when taking antibiotics and can manifest itself as local irritation or anaphylactic shock.
The choice of drugs is made by a gastroenterologist. He also prescribes remedies to combat negative consequences. This question is usually relevant during long-term antibacterial therapy of the chronic form.
Cholecystitis, in any form, is a curable disease. But it is important to seek medical help in time and not neglect the advice of your doctor. The use of antibiotics in the treatment of the gallbladder is justified and brings the expected effect.
The effect of antibiotics for cholecystitis
Now in medical practice there are several standard regimens for treating cholecystitis with antibiotics. Depending on the course of the disease, its complexity, periods of exacerbation and other factors, the doctor may use or independently create new treatment regimens.
Standard regimens for the use of antibiotics for cholecystitis:
- Aminoglycosides in combination with ureidopenicillins and Metronidazole. Antibiotics are administered by injection: Gentamicin (up to 160 mg) in the morning and evening hours + Metronidazole 500 mg and Azlocillin 2.0 three times a day.
- Cephalosporin antibiotic + a drug from the penicillin group: Ceftazidime 1.0 (3 doses per day) + Flucloxacillin 250 mg (4 doses per day).
- Cephalosporin antibiotic and Metronidazole: Cefepime 1.0 in the morning and evening, simultaneously with Metronidazole 500 mg 3 times a day.
- Ticarcillin with Clavulanic acid 3 g 1 time every 5 hours intravenously (up to 6 injections per day).
- Penicillin antibiotics and fluoroquinolone group drugs: Ampicillin 500 mg 5-6 times a day + Ciprofloxacin 500 mg 3 times a day.
In a critical situation, when the patient's blood urgently needs to be cleared of a certain medication, hemodialysis can be performed. Paradoxical situations often arise when the occurrence of cholecystitis is caused precisely by the use of certain types of antibiotics.
This may be due to increased dosages or too long treatment.

Drugs for pancreatitis and cholecystitis
Pancreatitis is treated with antibacterial agents when there is a possibility of the inflammatory process spreading to the gallbladder or simultaneous inflammation of both organs has begun. In this case, the risk of developing peritonitis increases due to contact of the diseased organ with the abdominal wall.
In case of simultaneous organ damage, drugs from the group of penicillins and cephalosporins are prescribed. The first includes: Ampicillin, Amoxicillin, Augmentin. The second group includes: Ceftriaxone, Cefuroxime, Cefoperazone.
These substances act very quickly, within 15 minutes after use the concentration reaches a maximum, the effect of the drugs continues for 12 hours.
To enhance the effect of medications, they are prescribed in combination with:
| Enzymes | Mezim, Pancreatin. |
| Antispasmodics | Drotaverine, No-shpa. |
| Means that normalize the flow of bile | Holisal. |
| Antiemetics | Metoclopramide. |
| Antacids | Maalox, Almagel. |
Antibiotics for cholecystitis during exacerbation
If there is a risk of more serious diseases, such as peritonitis, or empyema of the gallbladder during exacerbation of cholecystitis, antibiotics are prescribed. This also applies to complications of a septic nature.
Also, antibiotics for inflammation of the gallbladder in the acute stage are prescribed optimally for a period of up to 10 days. It is best to administer the medicine intravenously: this is the most effective way to quickly deliver the drug to the site of inflammation.
In case of exacerbation of cholecystitis, Cefuroxime, Ceftriaxone, Cefotaxime , and also Amoxicillin and Clavulanate . Treatment can be carried out using cephalosporins and Metronidazole.
The regimen for prescribing antibiotics during an exacerbation of the disease is standard, but alternative options can be used. For example:
- Ampicillin 2.0 4 times a day (intravenously),
- Gentamicin (intravenously),
- Metronidazole 0.5 g 4 times a day (intravenously).
The combination of Metronidazole and Ciprofloxacin has a positive effect.

What is the danger of gallbladder inflammation?
Inflammation of the gallbladder (acute cholecystitis) is a consequence of eating large amounts of unhealthy and fatty foods and poor nutrition. In addition, intestinal infections, parasites, cancer, and metabolic disorders can cause inflammation.
The main symptoms of inflammation are:
Low-grade fever
- feeling of heaviness in the stomach;
- heat;
- belching;
- heartburn;
- flatulence;
- feeling of fullness in the area of the right hypochondrium;
- abdominal cramps.
The danger of inflammation of the pancreas is that, in the end, various liver pathologies can develop, as well as chronic pancreatitis.
If you feel unwell, you should immediately seek help from a medical facility. Self-medication can only worsen the general condition of the patient. The sooner proper treatment is started, the more effective it will be.
Antibiotics for chronic cholecystitis
For cholecystitis in the chronic phase, antibiotic treatment can be used for active inflammation in the biliary system. Antibacterial therapy takes place during the period of exacerbation of the underlying disease, and it is necessary to simultaneously prescribe choleretic and antiseptic agents. Among them are the following:
- Erythromycin 0.25 g four times a day,
- Oleandomycin 500 mg four times a day after meals,
- Rifampicin 0.15 g three times a day,
- Ampicillin 500 mg four to six times a day,
- Oxacillin 500 mg four to six times a day.
Benzylpenicillin intramuscularly, Phenoxymethylpenicillin tablets, Tetracycline (250 mg) 4 times a day, Metacycline (300 mg) twice a day and Oletetrin (250 mg) 4 times a day will also be effective

Use of combination treatment
Even modern drugs of the II and III generation cephalosporin class are not always sufficiently effective for severe cholecystitis. The threat of the formation of empyema (ulcer) in the gallbladder, peritonitis with a breakthrough into the abdominal cavity necessitates the use of combinations of antibiotics with other anti-inflammatory drugs or two drugs from different groups.
Thus, cephalosporins form active combinations with Metronidazole:
- Cefoperazone;
- Ceftriaxone;
- Cefotaxime;
- Cefuroxime;
- Ciprofloxacin.
Another option: Ampicillin + Gentamicin + Metronidazole. In this case, some drugs are administered intravenously, others intramuscularly. Instead of Gentamicin, Sizomycin is used, since nosocomial strains of microorganisms provide up to 90% resistance to Gentamicin.
In order to eliminate the side effects of aminoglycosides, combinations of third generation cephalosporins and the newest penicillins are recommended:
- Ceftazidime (can be replaced with Fortum or Tasicef) + Flucloxacillin.
- Cefipime (belongs to the IV generation of cephalosporins) can be replaced with Maximim and used in combination with Metronidazole.
Antibiotics for calculous cholecystitis
Gallstones interfere with the outflow of bile and at the same time irritate the walls of the bladder and ducts, provoking painful sensations and inflammatory processes in the gastrointestinal tract. The latter are much more difficult to treat, due to their localization in close proximity to the gastrointestinal tract.
The infection can enter the biliary system along with the bloodstream. It is this factor that leads to the fact that patients suffering from diseases of the urinary system and intestinal diseases automatically begin to suffer from cholecystitis.
Calculous cholecystitis requires complex treatment using broad-spectrum antibiotics.
Among such antimicrobial agents, the following are most often prescribed:
- Ampioks,
- Erythromycin,
- Ampicillin,
- Lincomycin,
- Erycycline.
These drugs are taken 4 times a day, the dosage is selected individually for each patient. Oletterin and Metacycline are also often used for chronic disease.

Rules of antibacterial therapy
Not all antibiotics can cure the disease. Some drugs have a very narrowly targeted effect and are active against a limited number of microbes.
When choosing antibacterial agents, doctors are guided by the following rules:
- The medicine must be sensitive to the identified microflora.
- It is necessary that the active substances penetrate the walls of the bladder and accumulate in the liver.
- Medicines should not have a significant toxic effect on the liver.
- The dosage is calculated according to the characteristics of each patient: weight, height, severity of the disease.
- Treatment is prescribed for the acute stage of the disease.
- It is advisable to take the drugs in injection form so as not to irritate the gastric mucosa.
- The optimal course of treatment is 8-10 days. Do not interrupt therapy or take medications for a long or too short time. This leads to the formation of resistance.
- It is mandatory to take vitamins B and C, they enhance the effect of medications.
- To prevent dysbiosis, probiotics are prescribed.
- If mixed microflora is detected, then several antibacterial agents are used, taking into account their compatibility.
Consequences of treatment
It's no secret that antibiotics leave a negative mark on the liver or can cause allergic reactions.
At the first manifestation of an allergy, you should inform your doctor and change the drug. After all, allergies can act in the form of anaphylactic shock, skin lesions, Quincke's edema and a number of other complications. To avoid any type of complications, you should not self-medicate. All appointments and consultations must be carried out by a qualified specialist. Then the treatment will be effective and safe.
Sulfa drugs
Antibiotics prescribed by the attending physician to the patient will significantly alleviate the condition at the beginning of the course and get rid of the infection by the end of the course.
The duration of treatment will be about 10 days (a longer course of taking antibacterial agents is fraught with the appearance of dysbacteriosis and thrush).
Antibiotics are divided into several groups based on their effect on the affected cell (violate its integrity or carry out protein metabolism inside).
The first group consists of the following drugs:
- Cefazolin is considered a first-generation drug; it acts on a wide range of microorganisms. The medicine is contraindicated for infants in the first month of life; during pregnancy it can be used under the strict supervision of a doctor.
- Penicillin accumulates in large quantities in bile, for this reason it is considered one of the most effective remedies for cholecystitis.
- Cephalexin is prescribed for acute disease. A broad-spectrum antibiotic is contraindicated in children under 12 years of age and in patients with chronic kidney and liver diseases.
The second includes:
- Levomycetin is prescribed only if the causative agent of cholecystitis is dysentery bacteria, salmonella or typhoid fever.
- Erythromycin is effective in exacerbation of cholecystitis.
- Tetracycline is prescribed if cholecystitis was caused by enterococcus, streptococcus or Escherichia coli.
- Gentamicin is used for severe etherococcal infections.
It is of great importance that the drug is prescribed by a doctor, since each of them has an individual spectrum of effects.
In a large percentage of cases, cholecystitis develops against the background of infection of the body with streptococci, enterococci, and E. coli.
In such cases, it makes sense to take a course of the following antibiotics:
- Cephalexin;
- Tetracycline;
- Levomycetin;
- Gentamicin;
- Ampicillin;
- Cefazolin.
In addition to their effect on the infected cell, antibiotics for cholecystitis are distinguished depending on the place of concentration of the active substance in the body of the patient and the method of its release.
Experienced doctors agree that Ampicillin, Tetracycline and Penicillin are most effective in treating cholecystitis. Their effectiveness is due to the fact that most of the medicinal substance accumulates directly in the bile.
Inflammatory processes of the gallbladder can develop in any person, including those for whom the above-mentioned drugs are contraindicated. Alternatively, the following may be prescribed:
- metronidazole;
- tetracycline;
- aminoglycoside (gentamicin).
All these active ingredients are effective against gram-negative microbes, which most often provoke cholecystitis. On the other hand, they have many disadvantages, for example, metronidazole does not accumulate in the wall of the gallbladder, only in its lumen. Aminoglycosides and tetracyclines are toxic to the liver, kidneys and auditory nerve.
Antibiotic treatment of cholecystitis, both acute and chronic. The use of antibiotics must be justified and carried out correctly in order to achieve the desired effect.
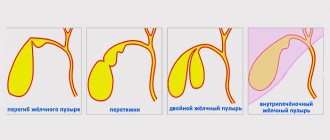
Cholecystitis is a disease characterized by inflammation of the gallbladder.
As a rule, it develops as a result of a violation of the outflow of bile from this organ, located on the right side of the peritoneum, under the liver.
There are two variants of the disease, the symptoms of which differ slightly from each other. We are talking about acute and chronic cholecystitis.
Symptoms characteristic of this type of disease such as acute cholecystitis:
- sudden increase in body temperature, chills;
- severe, jerking pain localized in the right side of the peritoneum and radiating to the upper chest;
- constant nausea, profuse vomiting;
- sometimes - jaundice and severe skin allergies caused by toxic poisoning of the body.
In acute cholecystitis (as in pancreatitis and other abdominal pathologies that have an acute course), hospitalization is indicated.
A patient suffering from an acute form of the disease must be constantly under the supervision of doctors and take the necessary medications to ensure his treatment, which not only fight cholecystitis, but also relieve the load on the heart, liver and other internal organs.
If acute cholecystitis cannot be blocked within a short time, then doctors may initiate abdominal drainage of the gallbladder and even abdominal surgery.
In the second form of the disease – chronic cholecystitis – slightly different symptoms are noted:
- quiet, muffled, but constant pain in the right side of the abdomen, radiating to the lower back and appearing ten to fifteen minutes after eating;
- nausea in the absence of vomiting;
- colic in the liver;
- yellowness of the sclera of the eyes and skin.
Medicine for nausea is used not only to eliminate this symptom of numerous diseases, but also to prevent it. A feeling of discomfort appears in the epigastric region and then spreads to the esophagus.
The cause of the development of nausea and vomiting is the vagus and splanchnic nerves. It is their irritation that provokes excessive salivation, chills, arrhythmia, arterial hypotension, and dizziness.
These negative signs of deterioration in health almost always accompany nausea. Before taking the pill, you need to determine the cause of the pathological symptom.
How to choose the right drug
Brief overview of the main drugs
Ampicillin ®
The drug belongs to the semisynthetic aminopenicillins. Amycillin ® is highly effective against cholecystitis caused by Escherichia coli, Enterococcus, Proteus, staphylococci and streptococci. The drug accumulates in bile in high concentrations, even in severe cholestasis. The disadvantages of the antibiotic include the fact that it is completely destroyed by bacterial enzymes beta-lactamases, therefore, if it is suspected that the inflammation is caused by beta-lactamase-producing strains, it is recommended to prescribe an inhibitor-protected version: ampicillin + sulbactam.
Ampicillin ® is prescribed intramuscularly at 0.5-1 grams every 6 hours. In severe cases, the daily dosage can be increased to six grams, divided into 4-6 injections.
For children over 6 years of age, the drug is prescribed at 100 mg/kg per day. The daily dose is divided into 4-6 injections.
For patients with renal dysfunction, the dosage is adjusted according to the glomerular filtration rate.
The antibiotic is contraindicated in patients with mononucleosis, lymphoproliferative diseases, severe kidney and liver dysfunction, and beta-lactam intolerance.
Ampicillin can be prescribed to pregnant women. If it is necessary to use the product during breastfeeding, breastfeeding should be temporarily stopped.
Oxamp ®
For severe staphylococcal cholecystitis caused by penicillinase-forming strains, a combination of ampicillin and oxacillin is used. Oxacillin ® also belongs to the penicillin series, but unlike ampicillin, it is not destroyed by bacterial enzymes.
For adults and children over 14 years of age, Oxamp ® is prescribed 500-1000 milligrams four times a day. Patients over seven years of age are prescribed 50 milligrams per kilogram per day.
Contraindications to the use of antibiotics are similar to those for the use of ampicillin.
Cefazolin ® (Kefzol ® )
The drug belongs to the first generation cephalosporin antibiotics. Cefazolin ® is highly active against a wide range of microorganisms, including all major causative agents of cholecystitis.
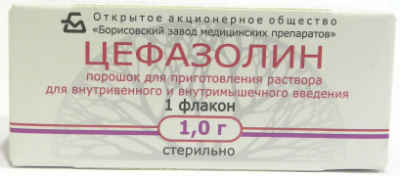
The drug is contraindicated in patients with allergies to beta-lactams and in patients younger than 1 month of life. An antibiotic may be prescribed to pregnant women if the expected benefit outweighs the possible risk.
For adults, Cefazolin ® is prescribed 500-1000 milligrams twice a day. In severe cases, the antibiotic can be used one gram three times a day.
Children are prescribed 25-50 mg/kg per day. The daily dose is divided into three to four administrations. In severe cases of the disease, the daily dose can increase to one hundred milligrams per kilogram.
Ciprofloxacin ®
Fluoroquinolone antibiotic with a wide spectrum of antibacterial activity. The antibiotic accumulates in high concentrations in the bile and acts on all the main causative agents of inflammation of the gallbladder.
Ciprofloxacin ® for cholecystitis is used if the patient has allergies or other contraindications to the use of beta-lactam antibiotics.

Ciprofloxacin ® is prescribed in a dose of 0.5 to 0.75 grams twice a day.
Like all fluoroquinolones, ciprofloxacin ® is not prescribed to children under 18 years of age, women carrying a child or breastfeeding, patients with glucose-six-phosphate dehydrogenase deficiency, severe kidney and liver dysfunction, as well as intolerance to fluoroquinolone antibiotics or tendon inflammation associated with history of taking these drugs.
With extreme caution, the drug can be prescribed to patients with pathologies of the central nervous system and mental disorders, cerebrovascular accident (cerebrovascular accident), and elderly patients.
Metronidazole ®
Nitroimidazole derivatives are prescribed in addition to the main antibiotic if a mixed aerobic-anaerobic infection is suspected.
The drug is not prescribed to patients in the first trimester of pregnancy, patients with diseases of the central nervous system, blood, or severe liver damage.
In the second and third trimester, metronidazole ® can be used if absolutely necessary. Natural feeding is stopped for the duration of treatment.
For cholecystitis, metronidazole ® is prescribed 0.5 grams intravenously every six hours.
For children, antibiotics are prescribed at 7.5 milligrams per kilogram every 6 hours.
Useful video about the treatment of cholecystitis
Cholecystitis is a nonspecific inflammatory disease of the gallbladder. It is customary to distinguish acute and chronic stages of the disease.
Chronic cholecystitis often develops gradually as an independent pathology. The main cause of the disease is the pathological outflow of bile in the biliary tract, which develops against the background of cholelithiasis.
With timely contact with gastroenterologists, conservative treatment of cholecystitis is possible. Antibiotics for cholecystitis form the basic basis of drug therapy.
Why?
What antibiotics should you take for cholecystitis?
Definition of cholecystitis
Inflammation of the gallbladder can occur as an acute or chronic, calculous or acalculous process. Non-calculous chronic cholecystitis is a local inflammation of the bladder walls, accompanied by dysfunction of the biliary tract and disturbances in the properties of bile.
Most gastroenterologists consider acalculous chronic cholecystitis to be the main stage in the development of cholelithiasis in patients.
In order to start talking about medications for pancreatitis, you must first understand the concept of “pancreatitis”, its types and some features of the course of the disease, since these components fundamentally influence the choice of the best medicine for pancreatitis.
What is pancreatitis
Pancreatitis is an acute or chronic inflammatory-destructive process in the tissue of the pancreas, characterized by the phenomena of autolysis (self-digestion) and the development of dystrophic processes.
Principles of therapy
If an acute form of pathology with pain, inflammation and infection is detected, then antibiotics are taken for cholecystitis. The doctor selects drugs that accumulate and concentrate in the bile.
In the chronic course of the pathology, the outflow of fluid is disrupted and spasms are observed. In this case, it is recommended to treat cholecystitis with symptomatic and pathogenetic drugs.
To improve the outflow of fluid from the gallbladder and reduce pain, take medications such as:
- Riabal;
- Papaverine;
- Baralgin.
The above products are available in the form of suppositories or tablets. In severe cases of the disease and severe pain, injections are prescribed. If cholecystitis is accompanied by hypotonic dyskinesia, and the gallbladder secretes fluid sluggishly and weakly, then take choleretic tablets (Allohol, Cholenzym).
Drugs for the acute period of the disease
The acute process is usually caused by an infection, which occurs against the background of a violation of the normal outflow of bile.
In case of cholelithiasis, when the obstruction is caused by blockage of the duct by a stone, cholecystitis is treated with the use of choleretic drugs (when tests indicate the possibility of the stone passing on its own).
Treatment of inflammation should be carried out even if the formation is successfully released and the process of bile outflow is stabilized, since during this period pathogenic microflora can join in any case.
In the acute course of the disease, antibiotics are necessary to prevent the development of a purulent process. Otherwise, there will be a need for resection or cholecystectomy at the stage of a phlegmonous, purulent or gangrenous process, which will be the result of an exacerbation stage.
It is imperative to treat cholecystitis with antibiotics, since a bacterial infection is present even when an aseptic process has been identified. It just joins the disease later, when damage to the organ mucosa occurs, caused by increased levels of lysolecithin. The following types of drugs are often used:
- “Ampioks”, “Gentamicin” and cephalosporins, since they have a wide spectrum of action, “Furazolidone”, which is known as a means of extensive antimicrobial action, can be used;
- erythromycins, which can accumulate in bile secretions, that is, they go directly to their destination (“Spiramycin”, “Azithromycin”, “Roxithromycin”);
- tetracycline and penicillin drugs also accumulate in the bile and are used for reasons of expediency: they are effective against the most common infections in cholecystitis - enterococci, streptococci, E. coli;
- "Amoxicillin" is combined with clavulanic acid - this combination is present in "Augmentin", "Amoxiclav", "Flemoclav".
The best option for cholangitis and other related complications is the use of multicomponent medications that contain various antibacterial drugs.