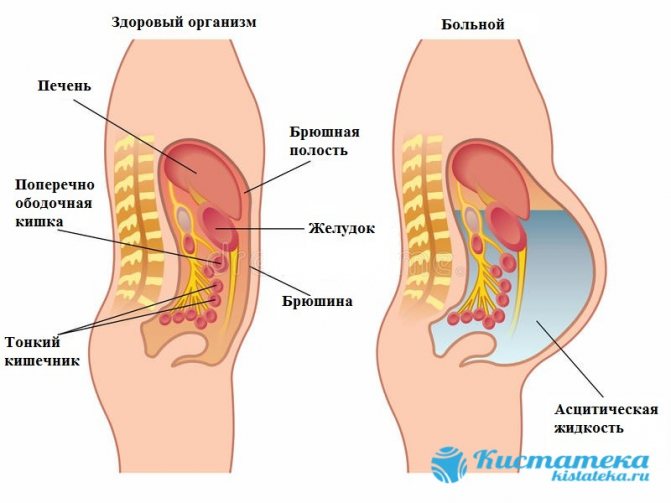
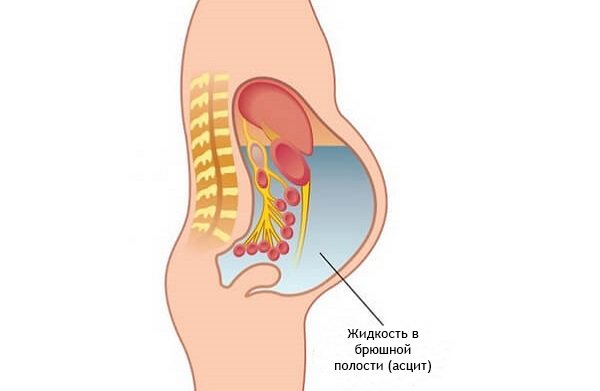
Abdominal ascites is a pathology characterized by the accumulation of fluid in the abdomen. Such a disorder is considered a complication of a number of extremely life-threatening diseases. Ascites usually occurs in a progressive form. If the volume is small, the fluid in the abdomen may resolve on its own if treatment of the primary disease is effective.
In severe forms of this disorder, more than 15 liters of transudate may accumulate in the abdomen, which will no longer be able to find a way out on its own.
[toc]The reasons why this phenomenon occurs can be very diverse. For example, ascites can develop against the background of fungal, tuberculous and parasitic lesions of the abdominal cavity.
Gradually, the accumulation of fluid in the abdominal cavity not only causes mechanical compression of organs, but also predisposes to a number of dangerous complications. Often, patients with a severe form of edematous-ascitic syndrome develop obstruction due to intestinal compression, as well as peritonitis, since transudate, the amount of which increases in the abdomen, is an ideal nutrient medium for microflora.
Etiology of abdominal ascites
Many diseases can cause pathological fluid accumulation. Men who are susceptible to alcohol addiction often suffer from this disorder. Alcohol cannot directly provoke edematous-ascitic syndrome, but its breakdown products quickly destroy the liver. This organ is a multifunctional natural laboratory. It is the liver that is responsible for the production of proteins that regulate the degree of permeability of both blood and lymphatic vessels. Frequent consumption of alcoholic beverages contributes to the destruction of the tissues of this organ. Most people who have suffered from alcohol addiction for many years are diagnosed with severe forms of cirrhosis. In this case, the liver tissue is so destroyed that it cannot cope with its functions.
Specifics of the disease
In some cases, ascites is associated with profuse swelling. If the disease occurs against the background of an acute inflammatory process, the development of ascites-peritonitis, an extremely dangerous, life-threatening condition, is possible. It can be recognized by the results of an analysis of intra-abdominal fluid. If the protein compounds in it significantly exceed the norm, and the sediment consists of a huge number of leukocytes and erythrocytes, the disease is confirmed.
The most characteristic symptom of ascites (we will discuss how the disease is treated further) is an enlarged abdomen. Unlike ordinary bloating due to flatulence in the intestines, the presence of cystic formations of the ovaries or uterus, in which the abdomen can also become larger, dropsy is characterized by dullness of percussion sound. If the patient takes a standing position, the fluid will concentrate in the lower peritoneum; if he lies horizontally, dull percussion will be heard on the sides.
Causes and risk groups
In 70% of cases of ascites, cirrhosis plays a major role. In severe cases of liver damage, accompanied by accumulation of fluid in the abdomen, the prognosis is unfavorable.
Often, abdominal ascites develops against the background of diseases accompanied by portal hypertension. Such pathological conditions include:
- sarcoidosis;
- hepatosis;
- hepatic vein thrombosis due to cancer;
- widespread thrombophlebitis;
- stenosis of the inferior genital or portal vein;
- venous stagnation;
- alcoholic hepatitis.
The accumulation of fluid in the abdomen can be a consequence of various diseases of the kidneys, gastrointestinal tract and heart. This complication often accompanies pathological conditions such as:
- myxedema;
- glomerulonephritis;
- nephrotic syndrome;
- heart failure;
- pancreatitis;
- diarrhea;
- Crohn's disease;
- lymphostasis.
Often, edematous-ascitic syndrome develops against the background of oncological processes occurring in the body. Often such a complication is observed when malignant tumors of the large intestine, stomach, ovaries, breast and endometrium are affected.
Sometimes pathological accumulation of fluid in the abdomen develops as a result of diffuse peritonitis, Crohn's disease, tuberculosis, fungal infection and parasitic infestation. Ascites can be observed against the background of polyserositis caused by systemic lupus erythematosus, rheumatoid arthritis, Meigs syndrome, uremia, etc.
There are a number of factors predisposing to the appearance of ascites. Significantly increase the risk of developing such a problem by chronic hepatitis, alcohol abuse, injection drug use, blood transfusions, living in areas with unfavorable environmental conditions, obesity, tattooing, high cholesterol and type 2 diabetes. This is not a complete list of factors contributing to the development of ascites.
In newborns, ascites often occurs with the development of hemolytic disease of the fetus, which occurs during pregnancy. In young children, fluid in the abdominal cavity may begin to accumulate due to hemolytic disease, exudative enteropathy, malnutrition, and congenital nephrotic syndrome.
To effectively treat ascites, identifying the root cause of the problem is extremely important.
To prevent the re-accumulation of fluid in the abdomen, it is necessary to direct efforts to eliminate the underlying disease.
What is dropsy of the abdomen?
Let's figure out what is ascites or abdominal hydrops (another name for the disease)? This is a pathology in which there is an accumulation of ascitic fluid in the peritoneum, leading to the development of edema and ascites. Normally, ascitic fluid is formed in the peritoneum and is gradually absorbed by the vessels. But due to the development of other diseases, a malfunction occurs and the body produces too much of it or it simply stops being absorbed. Ultimately, the liquid can reach about 25 liters and this can lead to increased blood pressure and poor circulation.
Normally, ascitic fluid is formed in the peritoneum and is gradually absorbed by the vessels, but if it is abnormal, it begins to accumulate, forming a ball.
Very often you can hear about diseases such as hydrocele of the liver and hydrocele of the kidney. But, if the first is the main factor in the formation of ascites of the abdominal cavity, which appears as a result of the development of cirrhosis of the liver, then hydrocele of the kidney is an independent disease, accompanied by a violation of the outflow of urine from the renal pelvis. The second more popular name for the disease is hydronephrosis.
There are several main types of dropsy:
- cerebral or otherwise hydrocephalus in adults and newborns;
- chest;
- peritoneal;
- inguinal
Symptoms and treatment are different for each type.
Pathogenesis of ascites development
The peritoneum performs several important functions at once, including fixing the organs located in this area in their anatomical places, and also protects them from injury. Any healthy person has some fluid between the layers of the peritoneum, the volume of which is maintained at normal levels by an extensive network of lymphatic vessels. There is constant circulation of transudate here, that is, the old one is absorbed, and a new one comes in its place. However, certain serious diseases and pathologies can disrupt this delicate natural mechanism.
Ascites develops when the release of fluid into the abdominal cavity, the process of its reabsorption is impaired, or there is a decrease in the barrier to toxins.
Gradually, the volume of fluid increases, which leads to a number of complications. First, compensatory mechanisms are launched, so the lymphatic system begins to work at the limit of its capabilities, pumping more than 15 liters of fluid per day, removing it from the liver. Normally, the volume of pumped lymph when it is removed from this organ is about 7-8 liters. The venous network is unloaded, which contributes to a temporary improvement in the general condition. Subsequently, the overloaded lymphatic system can no longer cope with this task. Oncotic pressure decreases significantly and interstitial fluid volume increases. Due to these pathological processes, transudate sweats, where it accumulates.
Patient rehabilitation
Laparocentesis is not associated with global tissue trauma, and rehabilitation after it is short. 7-10 days after the operation, the patient's sutures are removed. To eliminate the symptoms of the main diagnosis, he needs to remain in bed for a few more days. During the postoperative period, physical activity is contraindicated for the patient.
To prevent relapse, the patient must stop eating salt and try to drink less fluid. You are allowed to drink no more than 1 liter of water per day. The daily diet should include a lot of protein, chicken, eggs, and dairy products. It is necessary to avoid eating spicy, pickled foods and sweets.
As practice shows, laparocentesis for most patients is an effective way to alleviate ascites, prevent the development of associated abnormalities, and prolong a person’s life. Refusal of the procedure is reasonable only if the patient has contraindications.
Symptoms of fluid accumulation in the abdomen
Despite the gradual development of edematous-ascitic syndrome, a rapid variant is also possible. There are 3 main stages of pathology: transient, moderate and intense. The nature of symptomatic manifestations depends entirely on the amount of accumulated fluid.
- With transient ascites, the volume of transudate does not exceed 400 ml. In this case, only swelling is observed.
- With moderate ascites, about 5 liters of fluid can accumulate in the abdomen. In this case, the manifestations become pronounced. The patient begins to notice problems with the functioning of the digestive organs and increasing signs of cardiac and respiratory failure.
- Tension ascites is diagnosed when the volume of fluid accumulating in the abdomen varies from 5 to 20 liters. At this stage of development of the pathology, the patient’s condition becomes extremely serious, as disruptions in the functioning of a number of vital organs increase.
Typically, edematous-ascitic syndrome develops gradually. With this classic version, the patient notices that his stomach is slowly increasing in size. As a rule, no obvious signs of a problem are observed at first, but the clothing size gradually increases. In some cases, the patient may be bothered by causeless weight gain. A noticeable increase in size is observed exclusively in the abdominal area. When more than 3-5 liters of fluid accumulates in the abdominal cavity, pronounced signs of ascites appear. These include:
- feeling of fullness;
- nausea;
- belching,
- abdominal pain;
- heartburn;
- protrusion of the navel;
- heartache;
- swelling of the abdomen in the sides;
- swelling of the legs;
- dyspnea;
- difficulty turning;
- gurgling noise during sudden movements.
The accumulation of a significant volume of transudate in the abdominal cavity is accompanied by a number of complications.
Often, due to increasing pressure, umbilical and femoral hernias develop. In addition, severe ascites can lead to rectal prolapse. In some cases, edematous-ascitic syndrome leads to the appearance of hemorrhoids and varicocele in men. Compression of organs located in the abdominal cavity often causes the development of obstruction and accumulation of feces. Accumulating fluid creates the preconditions for the development of peritonitis.
Transudate contains a large amount of protein, therefore it is an excellent breeding ground for pathogenic microflora. The development of peritonitis against the background of ascites usually leads to death. A significant increase in the volume of transudate causes disruption of the functioning of all vital organs.
Preparation
For the paracentesis procedure to be successful, it is necessary to properly prepare for it.
First of all, the patient must undergo a series of diagnostic examinations, which includes a urine and blood test, a coagulogram, an ultrasound examination of the pelvic organs, and radiography. Consultation with a therapist and other specialists is required.
Since the procedure may require laparoscopy or laparotomy, all preparatory measures must be carried out as for a classic operation.
On this topic
- Oncogastroenterology
What kind of pain occurs with rectal cancer?
- Olga Vladimirovna Khazova
- December 3, 2020
Before performing a abdominal puncture, you must empty your bladder. This can be done independently by the patient himself or with the help of a catheter when the person is unconscious. A tube is used to remove the contents of the stomach.
If the patient is in a state of shock, anti-shock therapy is first administered. This is necessary in order to maintain hemodynamics. Also, if there are significant indications, the patient is connected to a ventilator.
Methods for diagnosing abdominal ascites
The process of identifying fluid accumulation in the abdomen is currently not difficult. First of all, the doctor gets acquainted with the medical history to identify diseases that can provoke the development of such a pathology, and also performs percussion, that is, tapping.
Even light clicks on the stomach cause oscillatory movements of the fluid located inside. When a large amount of transudate accumulates, if you place your palm on one side of the abdomen and clap on the other, a pronounced fluctuation is observed.
Computed tomography and ultrasound are performed to confirm the presence of fluid in the abdominal cavity. In addition, general and biochemical blood and urine tests are done to make a diagnosis. Depending on the patient's medical history, chest X-ray, examination of abdominal fluid, Doppler sonography, selective angiography, and hepatoscintigraphy may be necessary. If the root cause of the complication cannot be identified, a diagnostic laparoscopy is performed, which allows all the fluid to be removed and a biopsy of the peritoneum to be performed.
Technique
Before puncturing the peritoneal wall, the patient is given a local anesthetic. To perform the technique, instruments such as a trocar, a tube for removing fluid, clamps and syringes are used.
The contents that are removed from the abdominal cavity are collected in a special container. Before sending it to the laboratory for bacteriological examination, it is placed in sterile tubes.
The doctor who performs the operation must wear gloves. If paracentesis is performed for ascites, the patient is covered from above with a film or an oilcloth apron.
On this topic
- Oncogastroenterology
How does colon cancer hurt?
- Olga Vladimirovna Khazova
- December 3, 2020
The tactics of performing the procedure do not cause any difficulties for the surgeon. Novocaine or lidocaine is used as an anesthetic. It is injected into the soft tissues in the abdominal area. The place where the puncture will be made is treated with an antiseptic solution.
The patient is in a sitting position when the puncture is performed to remove fluid that has accumulated due to ascites. In other situations, the patient should lie on his back.
The puncture is made along the midline, with a distance of two centimeters down from the navel. Before the trocar is inserted, a small incision is made with a scalpel. In this case, the skin, fiber and muscle tissue are dissected. All actions must be performed with extreme caution, as there is a high risk of damage to internal anatomical structures.
Most surgeons prefer to push the soft tissue apart using a blunt method, which is safer for the patient. As the surgical instrument moves in, it is important to continually control bleeding. This will allow you to avoid obtaining false research results in the future.
A trocar is inserted into the hole in the peritoneal wall, which is then inserted with rotational movements into the abdominal cavity. Its inclination relative to the xiphoid process should be 45 degrees.
To create a space through which the special trocar will move, the specialist grabs the umbilical ring. As a result, a slight elevation of the peritoneal wall occurs. To ensure safety and facilitate puncture, surgical thread is also used. It is inserted into the puncture area through the aponeurosis.
With ascites
In this case, laparocentesis can be performed on an outpatient basis. The trocar is inserted according to the same principle as described above. After liquid appears in its cavity, in order to remove it, the device is tilted towards a previously prepared container. The distal end is held with fingers.
If the ascitic contents are excreted quickly, this process may be accompanied by fluctuations in blood pressure, which can provoke collapse, since in this condition the blood rapidly penetrates into the vessels of the peritoneum, which were previously compressed by the accumulated fluid.
To prevent the sudden onset of hypotension, it is necessary to remove excess contents at a slow pace. Typically about one liter over five minutes. It is important to constantly monitor the patient’s condition.
On this topic
- Oncogastroenterology
Does ultrasound show colon cancer?
- Olga Vladimirovna Khazova
- December 3, 2020
During the manipulation, the assistant gradually tightens the patient's abdomen to prevent hemodynamic disorder.
After complete removal of the ascitic contents, the trocar is removed. The incision is sutured and covered with a sterile bandage.
It is not recommended to remove the compression towel. This will ensure normal pressure inside the abdominal cavity and gradual adaptation of the patient to the new created conditions for the blood supply to the organs.
Conservative treatment of ascites
To prevent the accumulation of transudate in the abdomen, the primary disease must be treated first.
Complex therapy is especially important for heart failure, tumors and liver damage.
If there is transient ascites, clear improvement can be achieved with conservative measures. The patient is prescribed a strict salt-free diet for abdominal ascites. It is imperative to include foods high in potassium in your diet. These include:
- baked potato;
- dried apricots;
- spinach;
- raisin;
- grapefruit;
- asparagus;
- green pea;
- carrot;
- oat groats.
Despite the fact that the diet has a lot of restrictions, it must be designed so that the patient’s body receives all the necessary proteins, fats, vitamins and minerals. Depending on the characteristics of the primary disease, the list of foods that are recommended to be excluded from the diet may vary significantly.
The amount of liquid consumed per day should be limited to 1 liter.
In addition, medications are prescribed to help restore water and electrolyte balance.
Diuretics can have a significant positive effect, but they should be used with extreme caution. At a moderate stage of ascites, in addition to medications and diet, puncture removal of fluid from the abdomen is used to a limited extent.
Abdominal laparocentesis for ascites can very quickly improve the patient's condition. Up to 5 liters of transudate can be eliminated in one puncture. It is not recommended to immediately remove large amounts of fluid, since collapse may develop due to a rapid decrease in intra-abdominal pressure. In addition, this treatment method creates optimal conditions for inflammatory processes, infection, the formation of adhesions and the occurrence of other complications. This method of treatment is effective when there is non-strain ascites. In severe cases, when frequent evacuation of fluid from the abdomen is required, a permanent peritoneal catheter is installed. When ascites progresses, treatment can only slow down the process.
General signs and symptoms
The accumulation of abdominal fluid leads to an increase in intra-abdominal pressure, as a result of which the dome of the diaphragm is pushed into the chest cavity. First of all, this negatively affects the functioning of the pulmonary and cardiovascular systems: patients experience heart rhythm disturbances, and severe shortness of breath develops even at rest. In addition, ascites is accompanied by protein loss and water and electrolyte imbalance.
An increase in intra-abdominal pressure threatens the development of an umbilical hernia, dilation of the veins of the spermatic cord, the formation of hemorrhoids, prolapse of a segment of the colon, the development of severe lumbar pain and pinching in the spine (it is difficult for the patient to roll over on his side and rise from a lying position).
Initially, the patient observes a sharp and inexplicable weight gain. Along with this, there is an increase in waist volume, this becomes especially noticeable when it is necessary to fasten the belt on trousers. The patient also complains of frequent heartburn, belching, increased acidity in the mouth, heaviness in the stomach, nausea, and sometimes vomiting. Due to compression of the intestines, problems with stool in the form of prolonged constipation are possible.
As dropsy progresses, an increase in the area of the peritoneum is observed: in the “standing” position, the stomach protrudes, but in the lying position, free fluid begins to distribute and protrude in the lateral sections.
Surgical treatment of ascites
Surgical interventions to eliminate fluid from the abdominal cavity are used only in severe cases, when other methods are not effective or there are complications of the pathology. For example, if the transudate becomes infected with microflora and peritonitis develops, all accumulated fluid is removed and the intestines and abdominal organs are treated with special solutions. Such a radical method of treatment does not always save the patient’s life, but there is no other method of eliminating infected exudate.
Among other things, if a patient is diagnosed with severe ascites, a peritoneovenous shunt is installed or deperitonization of the abdominal walls is performed. This allows liquid to be removed directly. In addition, surgical interventions can be performed that indirectly help eliminate ascites. In some cases, measures are necessary to reduce pressure in the portal system. For this purpose, lymphovenous anastomosis or reduction of splenic blood flow is often performed. In addition, intrahepatic bypass can be performed. In rare cases, splenectomy is performed. When ascites develops against the background of cirrhosis, only liver transplantation can improve the patient's condition and prevent the accumulation of transudate.
Medical history – cirrhosis of the liver ascites
In liver cirrhosis (LC), fatigue and loss of energy are common early symptoms associated with decreased appetite and nausea.
“Spider nevus” (dotted red patches of blood vessels that create a spider-like appearance) appear on the skin. Patients in the advanced stage develop jaundice (yellow color of the skin and whites of the eyes), caused by the inability of the liver to remove bilirubin from the body.
Palmar erythema, or hepatic palm (redness), is common. In men, skin hairiness decreases, testicular atrophy may develop, and sometimes painful breast enlargement (gynecomastia) occurs.
Ascites is a common sign of the onset of cirrhosis. Fever, abdominal pain and pressure in the gastrointestinal tract are usually signs that an infection is present.
If a person has cancer, the probability of developing ascites reaches 10%. Fluid accumulation does not occur in all malignant lesions.
Prognosis for abdominal ascites
The accumulation of fluid in the abdomen is a serious complication of any disease. The survival prognosis depends on the general condition and the primary pathology that provoked the development of the problem. In addition, peritonitis, hepatorenal syndrome, hepatic encephalopathy and bleeding can significantly aggravate the situation. Unfavorable factors that worsen the prognosis include:
- elderly age;
- liver cancer;
- increased albumin levels;
- decreased glomerular filtration of the kidneys;
- diabetes;
- hypotension.
In older people with the pathologies presented above, the prognosis for the development of ascites is unfavorable. In this case, even with targeted therapy, the life expectancy of patients rarely exceeds 6 months, and in the most favorable case - no more than 2 years.
Ascites is a serious complication, indicating that the primary disease is severe.
Currently, new techniques are being actively developed to improve the condition of patients with this complication, but, as a rule, a good survival prognosis is observed only in cases where the pathology was identified at an early stage of development.
Complications
According to statistics, consequences after laparocentesis are observed only in 8-10 percent of patients. In most cases, the reason for their appearance is non-compliance with the rules of antiseptic treatment, the penetration of infection into the place where the puncture was made.
On this topic
- Oncogastroenterology
Stool color for bowel cancer
- Natalya Gennadievna Butsyk
- December 3, 2020
After the trocar is removed from the cavity, bleeding may occur. During surgery, the patient may faint. This often happens when the blood begins to rapidly distribute through the vessels.
Other complications include:
- injury to the intestinal loops, against which peritonitis may develop;
- vascular damage which leads to the formation of hematomas or extensive bleeding into the retroperitoneal cavity;
- entry of air, which entails the development of subcutaneous emphysema;
- the appearance of phlegmon in the area of the anterior wall;
- puncture of a malignant tumor - as a result, the oncological process can be activated, and the rapid spread of metastases to nearby anatomical structures and systems will begin;
- prolonged release of contents in the puncture area.
Currently, cases of complications are recorded extremely rarely. As a result, laparocentesis began to be considered not only effective, but also the safest method for pumping out fluid accumulated in the peritoneum.
It is important not to forget that during the procedure a lot of albumin is lost with the liquid. This condition often causes a lack of proteins. That is why it is important to ensure that the volume of the extracted effusion corresponds to its nature of origin, as well as the condition of the patient himself.
The likelihood of complications increases significantly if proper nutrition is not followed, if the requirements for emptying the bladder are not met, and also if the manipulations were carried out while the child was pregnant.
Where is ascites treated in our country?

Considering that ascites, as a rule, develops in patients with liver cirrhosis and cancerous tumors, you need to look for an institution of the appropriate profile. Today, several research institutes in Moscow and other Russian cities are engaged in the diagnosis and treatment of liver diseases. The most famous medical centers:
- "Research Institute of Epidemiology and Microbiology named after. G. N. Gabrichevsky Ministry of Health and Social Protection of the Russian Federation.”
- "Central Research Institute of Gastroenterology of the Moscow Healthcare Department."
- "Clinical City Hospital No. 20" on the street. Lenskaya.
- "Clinic of Oncoimmunology and Cytokine Therapy."
Ascites and cancer
Treating ascites in oncology, no matter how strange it may sound, is completely useless. When the peritoneum is damaged by cancer cells, it is important to remove the malignant neoplasms. If you manage to overcome oncology, the dropsy will go away on its own. An indispensable method of treating malignant diseases of the liver and peritoneum is chemotherapy (the drugs Cisplatin, Azathioprine, Methotrexate are used).
In combination with chemotherapy, the patient may be prescribed a course of radiation, which can kill cancer cells and reduce tumor size. The prognosis and quality of life can be improved after successful surgical removal of a malignant tumor.