Pancreatitis is a pathological process that develops in the tissues of the pancreas against the background of enzyme activation. Exacerbation of the disease is accompanied by pain localized in the right hypochondrium and the epigastric region (near the stomach). Additionally, heaviness that occurs after eating is noted. The chronic form can occur without symptoms, as a stage of remission or rest. How long an exacerbation of chronic pancreatitis lasts depends on the individual characteristics of the patient.
Forms of the disease
Gastroenterologists distinguish several forms of pancreatitis. The classification is based on the clinical picture. The form of the pathological process and the presence of concomitant diseases determine how long pancreatitis is treated.
The acute phase is divided into several subtypes:
When an inflammatory process begins in the body during an exacerbation, the chemical breakdown of enzymes responsible for the breakdown of proteins and peptides is activated. Provided that the nerve endings are not damaged, the pain syndrome is severe. Dangerous cases requiring immediate medical intervention are accompanied by intoxication and severe dehydration.
The period during which exacerbation of pancreatitis continues can range from 2-3 hours to one week. Most often, the acute form of the disease lasts 3-4 days. Medical practice and statistics say that it is at this stage that the most deaths occur - from 7 to 15% of all cases of inflammatory process in the pancreas.
The main signs of acute pancreatitis are:
- attacks of nausea, often accompanied by vomiting;
- increased gas formation;
- change in skin tone (it becomes white, gray);
- increased body temperature without other signs of colds;
- Halstead, Coolden and Gray-Turner symptoms.
The chronic form manifests itself differently. With the onset of this stage, an inflammatory-degenerative process begins to develop in the body of a sick person. Chronic pancreatitis can be divided into the following subtypes:
Unpleasant sensations are most often observed with the onset of the second type of disease. Most often, the pancreas hurts with chronic pancreatitis for seven days. But if the disease reaches a recurrent stage, pain will be observed constantly.

An ambulance should be called even when the patient does not know that he has an exacerbation of pancreatitis. After all, such pathological processes are dangerous because they can subside for a certain period of time, and then suddenly relapse.
The chronic form of pancreatitis may be accompanied by other pathologies of the gastrointestinal tract:
Signs of exacerbation of pancreatitis include the following symptoms:
- Pronounced dull, sharp pain of a girdling nature. It covers the epigastric region, left or right hypochondrium.
- The patient has diarrhea, while the stool has an unpleasant odor, is gray in color and contains pieces of food. The coprogram shows a high content of fiber, muscle fibers, and fat.
- Bitterness in the mouth, white coating on the tongue.
- Nausea, often accompanied by vomiting of bile.
- Increase in general body temperature.
- Violation or even complete lack of appetite, which is why the patient begins to rapidly lose weight.
- General weakness, decreased blood pressure.
The symptoms of pancreatitis are complicated by the fact that they are difficult to eliminate with medications. At the same time, the risk of another type of manifestation of pathology, reactive, remains.
The main sign of the reactive form is the immediate appearance of the clinical picture. It occurs due to food that has an irritating effect on the mucous membrane of the pancreas. When it is consumed, the ducts of the organ are clogged, all the produced enzymes remain inside. This damages the walls, causing an aggravation. The acute nature of the pain requires prompt medical attention. The attack is short-lived. Provided that the treatment is correctly prescribed, it stops after 4 days.
Symptoms
When an exacerbation occurs in the pancreas, it brings a lot of discomfort and pain to the patient. But, in some cases, signs of exacerbation may not appear. Common clinical manifestations:
- During the period when the pancreas is exacerbated, the patient experiences a dull or sharp pain in the hypochondrium. Often the pain radiates to the back.
- Problems with stool appear. During an exacerbation, feces become greasy, and remnants of undigested food are found in the feces.
- Symptoms of exacerbation of pancreatitis are always accompanied by bitterness in the mouth, a rumbling stomach, severe nausea and vomiting. In addition, a white coating is observed on the tongue during this course of the disease.
- Body weight decreases because the patient has no appetite.
Additional symptoms during exacerbation of the disease include:
- Pain in the peritoneal area can radiate to the back or lumbar region. It is quite rare for a patient to experience pain under the shoulder blades. In this case, the nature of the pain syndrome is dull. Signs of pain occur against the background of a large number of nerve endings, which are also involved in the pathological inflammatory process.
- In severe cases of the disease, pain shock occurs.
- The gag reflex also causes pain. The vomit contains the initial food, followed by vomiting bile.
- During the period when pancreatitis is exacerbated, symptoms such as belching, dry mouth.
- Shortness of breath or chills.
- In rare cases, the temperature rises.
In severe cases, signs of vitamin deficiency are observed on the skin, and blood pressure decreases.
How long to treat pancreatitis
How long an attack of pancreatitis lasts depends on the stage the disease has reached. If we talk about the acute phase, the clinical picture is observed over several hours. Then relief comes. Most often, such conditions are observed after eating fatty or fried foods in large quantities.
Chronic pancreatitis is dangerous because it can last for a long time without any symptoms. A relapse can occur against the background of a gross violation of the diet. Provoking factors include passion for alcoholic drinks, fried, spicy and fatty foods. You can eliminate an attack by simply removing foods that are dangerous to the pancreas from your diet.
The longer the chronic form remains without medical attention, the more dangerous the patient’s further condition. The aggressive form of the disease and exacerbations can be treated in a hospital setting.
Duration of treatment
Substitution treatment continues throughout the patient's life. When the tail of the pancreas is affected with destruction of the bulk of the islets of Langerhans, daily administration of insulin is required in a volume corresponding to the level of glycemia and bread units of food consumed. If exocrine insufficiency prevails, pancreatic enzymes after meals (Pancreatin, Creon) are indicated.
Patients who have developed an exacerbation of the disease are admitted to the hospital. As a rule, this occurs when the recommended diet is violated by consuming:
- acute;
- salty;
- overly sour;
- pickled products;
- fried.
Most often, remission is interrupted after taking even small doses of alcohol or non-alcoholic energy drinks (Red Bull, Adrenaline Rush).
Information! It takes from one week to a month or more to restore the condition of the pancreas. The duration depends on the severity of the lesion and the patient’s response to the drugs used.
Correction of the condition is carried out using a large number of saline and colloidal solutions (Trisol, Reopoliglucin), agents that inactivate the patient’s own enzymes (Gordox), histamine H2 receptor blockers (Famotidine), antispasmodics (Drotaverine). With the development of hemorrhagic syndrome, transfusion of coagulation factors and fresh frozen plasma is performed.
Pain syndrome requires the administration of analgesics. For moderate pain, NSAIDs (paracetamol, analgin) can be prescribed. In some cases, there is a need to use drugs.
In the first 2-3 days from the onset of an exacerbation, the patient needs to be hungry. Then they begin to feed him liquid food, gradually expanding the diet.
The list of permitted products includes:
- cottage cheese;
- steam omelette;
- lean fish;
- boiled vegetables;
- steam puddings;
- enveloping mucous porridges;
- baked apples.
You should avoid canned food, whole milk, fatty or smoked fish, difficult-to-digest meat, meat and mushroom broths, and fresh rye bread. In addition, you should avoid other foods that are irritating to the stomach and intestines.
What will happen if left untreated?
Chronic pancreatitis develops into an acute form if left untreated. This leads to dysfunction of the gastrointestinal tract. The produced pancreatic enzymes due to blockage of the ducts begin to have a negative effect on the organ. This is how ulcerative formations arise and processes that are irreversible in most cases begin.
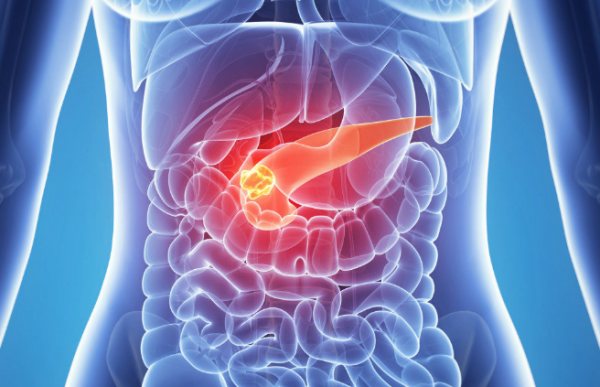
If pancreatic function is not restored, complications may occur:
- development of diabetes mellitus;
- formation of cysts, abscess;
- pleurisy, pneumonia;
- formation of stones in the pancreas.
Frequent bowel movements that accompany the reactive stage of pancreatitis deplete the body. In the absence of adequate therapy, this leads to general exhaustion and critical loss of body weight.
Lack of treatment in patients who have a genetic predisposition to cancer leads 4-5 years later to the development of pancreatic cancer. Therefore, even if during an exacerbation the stomach does not hurt much, you need to consult a doctor.
Forecast
Prognosis for exacerbation of the inflammatory process depends on the timeliness of therapy and compliance with the doctor’s recommendations. If the patient ignores the symptoms of an attack, the consequences can lead to death (peritonitis, sepsis) or a significant decrease in quality of life. In chronic pancreatitis, remission can reach several years, but only with adequate therapy and compliance with preventive measures.
Complications of the inflammatory process:
- renal failure;
- pancreas cancer;
- encephalopathy;
- internal bleeding;
- abscesses;
- death.
How to speed up treatment and restore the gland
If an adult is diagnosed with chronic pancreatitis, complex treatment is required.
Only in this case will it be possible to restore pancreatic function. Be sure to follow these recommendations in the event of the onset of the acute phase of the disease:
- If acute pain occurs, it is recommended to refrain from eating any food for three days. To maintain the salt and mineral composition, use mineral water (still), rosehip decoction without sweeteners.
- By the third day, slimy porridges, soups, and jelly are introduced into the diet.
- You should not eat solid food for two weeks.
- In case of severe manifestations of pain, it is recommended to remain in bed and apply cold to the epigastric area (ice bag, no more than 15 minutes at a time).
You should definitely call an ambulance. Before the doctors arrive, you can take an anesthetic antispasmodic drug (only No-shpa or Drotaverine will do).
During exacerbation of chronic pancreatitis, the diet expands gradually as the pain subsides. Protein-rich foods are introduced first:
- low-fat meat, steamed in the form of soufflés, meatballs;
- boiled lean fish;
- cottage cheese;
- protein omelettes.
Along with the diet, drug treatment is carried out. Inhibitors are used to reduce the production of enzymes and secretions. Anti-inflammatory drugs are required. They accelerate the healing of damaged gland walls. Drugs that prevent the formation of blood clots help restore microcirculation in the vessels of the organ. In the acute period, as well as during pain, taking enzymes is contraindicated, since increased secretion will aggravate the condition.
Symptoms of an attack of chronic pancreatitis
- pain that is localized in the left side of the ribs or in the upper abdomen. Often, they appear immediately after eating;
- flatulence;
- a sharp decrease in body weight;
- the appearance of a whitish coating on the mucous membrane of the tongue;
- nausea and vomiting.
The described symptoms can appear either one at a time or in combination, depending on the characteristics of the body, as well as the course of the disease.
However, it is impossible to diagnose an exacerbation of the disease solely by these signs. Similar symptoms of an attack of chronic pancreatitis are characteristic of many other diseases. Therefore, it is necessary to do a number of instrumental medical studies, including: blood and stool tests, ultrasound, computed tomography.
What to do in case of exacerbation of chronic pancreatitis?

As experts note, such a condition can occur at any time. It does not require a long period of time for its onset. As a result of an exacerbation, various vital organs, such as the kidneys or heart, may be damaged, because toxins and enzymes secreted by the pancreas can enter the bloodstream. And in case of hemorrhage, death may even occur. Therefore, an attack of chronic pancreatitis should be stopped immediately.
To do this, first of all, you need to refuse to eat any food. This recommendation must be followed for three days. Drinking is allowed in minimal quantities in the form of still water.
It is also necessary to ensure the patient's rest. Ideally, bed rest should be observed. To minimize pain, it is recommended to apply a cold heating pad to the pancreas area.
As for drug treatment, it must be prescribed by a competent doctor. There is no point in postponing a visit to a specialist. After all, chronic pancreatitis is an insidious disease. Relief is usually temporary. The attack itself will never go away. And without proper medical care, the disease will soon make itself felt again. Moreover, with new, even greater strength.
How long does an attack of chronic pancreatitis last?
In each individual case, the exacerbation of the disease can last for a different period of time. On average, the time interval is from one to three days.
Pancreatitis is common in medical practice. People may have different forms and course of pathology, but despite this, the quality of life deteriorates.
Patients are interested in how long they live with pancreatitis, what the prognosis is and whether death from the disease can occur.
Prevention of exacerbations
In chronic pancreatitis, eliminating exacerbations helps to avoid exacerbations. It is recommended to give up smoking, drinking alcohol, and carbonated drinks. Knowing the rules of proper nutrition helps avoid relapses.
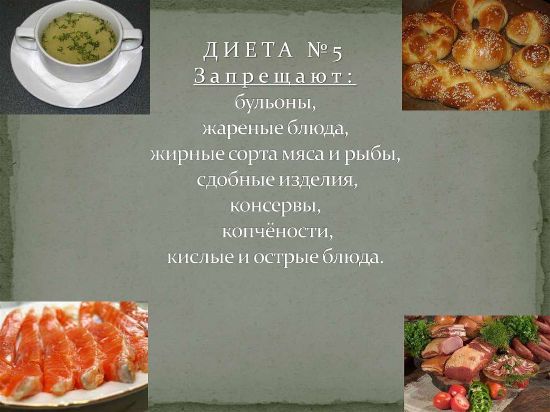
Patients with diagnosed pancreatitis are prescribed diet No. 5. Despite some restrictions for the prevention of exacerbations, it allows you to saturate the body with necessary substances. Food should be prepared by stewing and baking. The steam method will also work. You should eat at least 5-6 times a day, in small portions.
Stress is another provoking factor for exacerbation of pancreatitis. Eliminating it helps avoid relapse. Proper rest is also very important. You should undergo preventive examinations every four months.
Problems with the digestive system, although they do not rank first among the most dangerous diseases, are still one of the leading ailments affecting modern society. One of these diseases is chronic pancreatitis.
Chronic pancreatitis is a dysfunction of the pancreas, causing shrinkage of its parenchyma. This pathology is considered irreversible in medicine. Often the disease occurs as a result of ineffective treatment of acute pancreatitis. It is much more common in smokers and older people. Failure to comply with doctor's recommendations can lead to exacerbation of chronic pancreatitis.

This is what the pancreas looks like on an ultrasound
Diet
A therapeutic diet is the most important component of treatment for exacerbation of pancreatitis. A properly composed menu and compliance with medical recommendations allows you to relieve the digestive organs and provide them with peace.
The ban on eating any food can last up to three days. You are only allowed to drink alkaline mineral water up to 1.5 liters per day. Then liquid and semi-liquid dishes are introduced - puree soups, jelly. You should eat in small portions, but often. Alcoholic drinks of any strength, fatty, spicy and fried foods are prohibited.
As a basis, you can take diet No. 5, developed specifically to normalize the functioning of the gastrointestinal tract. It contains all the substances necessary for the body and excludes harmful products.
If you stick to a gentle diet for at least several months, you can achieve stable remission and significantly reduce the amount of medications you take. It is very important to satisfy the need for protein, so it is recommended to introduce meat products into the diet almost immediately after fasting.
The lean varieties that are best digested are rabbit, chicken, turkey and veal. Before cooking, the meat must be de-veined and minced in a meat grinder. As it recovers, it can be baked or boiled as a whole piece.
Since insulin is produced in the pancreas, you should not eat sugar for a month after an exacerbation. After the condition has stabilized, it is allowed to make jelly and compotes with fructose.
By the end of the first week of illness, the menu can include low-fat fish and steamed cutlets from it. Dietary varieties include cod, pollock, perch and navaga. Pike, pike perch, flounder and crucian carp contain 2% fat content. Canned fish and meat, salted, dried and dried fish, herring are prohibited foods for the entire period of treatment.
After fasting, it is recommended to eat rice and oatmeal porridge in water, well boiled. Sugar, butter and salt cannot be added to them. It is not advisable to include corn, millet and barley porridge in the menu, as they are very difficult to digest.
Diet during remission
When the attack is over and there are no acute symptoms, a significant part of the dietary restrictions is lifted and the range of permitted foods is expanded. However, you should not overload the pancreas, so it is still necessary to follow certain rules:
- fractional meals. Eating food in small portions up to 6 times a day promotes better absorption, and it is easier for a person to give up unhealthy foods;
- all dishes should be slightly warmed, neither hot nor cold;
- the amount of fats, proteins and carbohydrates in the diet is limited to 60, 120 and 400 g, respectively. It is not recommended to exceed these standards;
- Rough food is prohibited: foods should be boiled or steamed.

A light dessert made from available sugar-free products will diversify the patient’s diet and enrich the weakened body with vitamins
The diet is gradually introduced into pureed vegetable soups, yesterday's or pre-dried white bread made from 1st-2nd grade flour, pasta and cereals - rice, oats, buckwheat. When choosing pasta, it is better to give preference to small products (stars, rings, ears).
Dietary dishes that are recommended for chronic pancreatitis include a protein omelet, boiled or baked vegetables - potatoes, pumpkin, zucchini, carrots and beets. You can eat low-fat fermented milk products, such as cottage cheese, fermented baked milk, kefir and cheese. Fresh milk is permissible only in small quantities and diluted; it is better to add it to ready-made dishes or tea.
Butter and vegetable oil are used as fats within acceptable limits. The most useful fruits will be apples with a medium level of acidity and sweetness, as well as jam, jellies, mousses and compotes made from them.
To facilitate the functioning of the damaged organ and speed up the digestive process, proper drinking regimen is necessary. The amount of liquid consumed is about two liters. You can drink vegetable and fruit juices, rosehip decoction, alkaline mineral water, herbal teas, jelly and compotes.

You should only prepare peach juice during the season, since store-bought juices contain preservatives and a lot of sugar.
The most useful juices will be from peach, apples, pears, apricots, potatoes, pumpkins, tomatoes and cucumbers. It is better to prepare these drinks yourself, since dyes and preservatives are added to store-bought products. In addition, freshly squeezed juices should be consumed immediately; they cannot be stored in the refrigerator.
Green and red hibiscus tea has the mildest effect; drinking a drink made from kombucha is allowed. Kissels can be cooked from oatmeal, dried fruits, flaxseed, milk, as well as based on berries and fruits.
What is the pancreas responsible for?
This organ performs the functions of producing enzymes directly involved in digestion. This means that any disruption of the gland leads to malfunctions of the entire digestive system. Exacerbation of chronic pancreatitis, treatment of which is not started in a timely manner, can cause the development of gastritis and ulcers. A perforated ulcer is mortally dangerous, in which surgical intervention is inevitable. Enzymes secreted by iron:
Amylase is responsible for breaking down large protein chains into simpler elements. If this enzyme is deficient, the intestines will be unable to absorb many nutrients.
Lipase breaks down fats into glycerol and fatty acids, thereby helping the intestines absorb them. A lack of substance in the human body reduces the ability of the digestive system to absorb vitamins A, D, E, which can lead to many problems.
Note. Without vitamin D, the absorption of calcium in the body is impossible. Lack of calcium makes bones brittle.
Nuclease takes part in the body's absorption of nuclear (nucleic) acids.
Trypsinogen is an auxiliary enzyme, without which amylase does not break down carbon compounds.
Prophospholipase breaks down phospholipids into simpler elements.

The pancreas plays a major role in digestion
What's important to remember?
Inflammation of the pancreas, whether it is an exacerbation of its chronic form or an acute course of pancreatitis, is a serious disease.
In the absence of timely medical attention, it can lead to death.
A person suffering from pancreatic dysfunction should ensure that exacerbations occur as rarely as possible.
The main preventive measure is proper nutrition: without following a diet, any other methods of therapy are ineffective. By following all the specialist’s instructions, you can live with chronic pancreatitis for many decades without ever encountering an exacerbation of it.
Signs of illness
It is important to understand that treating the symptoms of exacerbation of chronic pancreatitis does not lead to a cure for the disease itself. And the treatment of the disease itself must begin with finding out the causes.
Exacerbation of chronic pancreatic inflammation is usually accompanied by the following clinical symptoms:
- Characteristic pain in the abdomen or in the left hypochondrium, radiating to the back in the area of the shoulder blades.
- Nausea.
- Vomit.
- Bitterness and dryness in the mouth.
- Frequent and copious bowel movements.
- Strong pungent odor of feces that is difficult to wash off.
- Weight loss.
- Decreased appetite.
- Irritability.
The period of exacerbation of chronic pancreatitis can last from 2 days to several months. If the pain is acute, then the exacerbation stage is usually short-term. With mild pain, the period can last up to several months.

Symptoms of exacerbation of chronic pancreatitis often appear in the autumn-spring seasons, when the body suffers from a lack of vitamins
Important! Typically, patients exhibit general symptoms of chronic pancreatitis, but treatment, on the contrary, is individual. It depends on the causes of the disease and the patient’s response to elements of medications.
Typical symptoms of pancreatic exacerbation
Pancreatitis in acute form cannot be ignored. A person experiences girdling pain, the center of which is in the epigastrium (between the ribs and the navel). At the beginning of inflammation, repeated vomiting may occur, after which no relief is felt and a rapid heartbeat occurs. If a person is able to ignore these signs, he will develop a fever within two to three days.
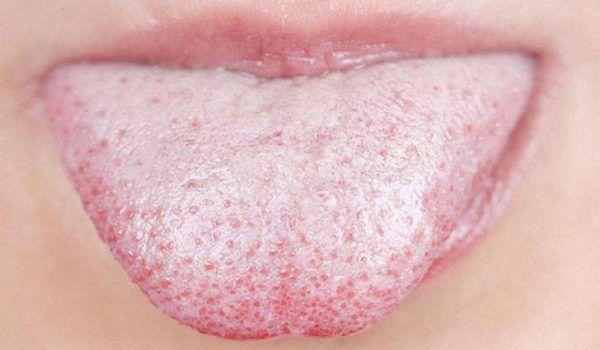
Patients with pancreatitis are characterized by a whitish coating on the tongue, a bitter taste in the mouth, and bad breath.
In acute pancreatitis, pain is constantly present and does not correlate with food or liquid intake. However, a reaction to a meal still occurs - after eating a person feels nausea or experiences a single vomiting, often with elements of undigested food. When taking painkillers, the pain subsides, and after the effect of the painkiller ends, it increases gradually.
Diagnostics
After determining the symptoms and etiology of the disease, the specialist doctor prescribes tests. Usually this:
- general and biochemical blood tests;
- Analysis of urine;
- fecal biochemistry;
- saliva tests to determine amylase levels.
An accurate diagnosis may require additional abdominal tests, such as a CT scan, MRI, x-ray, ultrasound, or endoscopy.
Fact. Did you know that the symptoms of exacerbation of chronic pancreatitis in adults and children are the same?

Additional studies give specialists an idea of the extent of organ damage and the stage of development of the pathology, which is important for timely and effective treatment
Summarizing
Pancreatitis, like any disease of the pancreas, is a dangerous illness that can deprive a person of the joy of a full life. We mentioned that the pancreas is a unique and irreplaceable organ, therefore it needs to be especially protected.
Exacerbation of pancreatitis occurs against the background of an acute illness. Every patient with pancreatitis should understand that the disease can manifest itself only six months later, immediately after its onset.
During this period of time, doctors diagnose a relapse of the acute form. If treatment is not started in time, the patient’s condition worsens, causing an exacerbation of chronic pancreatitis. Let's look at the main signs and find out what to do in case of exacerbation of pancreatitis.
At-risk groups
The disease affects all age groups and people of both sexes. However, chronic pancreatitis occurs more often in older people.
Conventionally, 9 risk groups can be distinguished, these are people:
- those suffering from alcohol addiction;
- those who eat haphazardly and often resort to fast food;
- taking a large number of medications;
- those suffering from nicotine addiction;
- having a history of gallstone disease;
- obese patients;
- patients with cardiovascular diseases;
- experiencing frequent stressful situations;
- those who have suffered a pancreatic injury or have recently suffered severe poisoning.

The disease causes anxiety, and constant pain in the left hypochondrium, lumbar and epigastric regions, as well as in the back between the shoulder blades keeps a person in constant irritation
Signs of exacerbation of pancreatitis
An attack of pancreatitis always begins with the onset of acute pain localized in the left hypochondrium. The pain syndrome intensifies in the absence of drug therapy. The pain may become wandering in nature and spread to the back, lower back, and shoulder blades. Painful symptoms are gradually joined by other signs of exacerbation of the inflammatory process.
Signs of development of exacerbation of pathology:
- characteristic pain after eating prohibited foods (fatty, fried, salty foods, alcohol, etc.);
- pain decreases if the patient assumes the fetal position or tilts the torso forward;
- pain occurs after taking enzyme medications (such medications increase the inflammatory process and enzyme activity of the pancreas).
First aid
Symptoms of exacerbation of chronic pancreatitis may be atypical. The patient may experience rapid heartbeat, pain between the shoulder blades, and increased temperature. It is easy for an unskilled person to confuse these symptoms with an attack of angina.
The main indicator of exacerbation of pancreatitis in this case will be acute pain in the left hypochondrium, radiating to the lumbar region or pain in the epigastric region. Acute pain is usually preceded by a gnawing pain that a person experiences even before the exacerbation.
Important! First of all, you need to call an ambulance.

In a critical situation, the main thing is to be collected and not panic, then you can provide the patient with the pre-medical care he so needs
To relieve severe pain during exacerbation of chronic pancreatitis, you must:
- remove the patient’s clothing that may impede breathing (tight tops, turtlenecks, sweatshirts, etc.);
- try to sit him down by tilting his body forward, this will help ease the pain;
- the patient should breathe shallowly without inhaling deeply;
- To reduce pain, it is recommended to periodically hold your breath;
- it is strictly forbidden to eat;
- every half hour you need to give the patient boiled still water, no more than 50 ml at a time;
- give the patient an antispasmodic drug (drotaverine or no-spa 0.8 g, papaverine 0.8 g); it is advisable to administer intramuscularly if you have the appropriate skills, according to the dosage;
- Do not give painkillers or enzyme preparations under any circumstances, this will make it difficult for the doctor to diagnose;
- Do not apply a heating pad or a cold compress to the sore spot.

In case of acute pain, hospitalization of a patient with chronic pancreatitis, the symptoms of which were determined by the doctor on duty, is a common procedure
First aid measures
Exacerbation of the pancreas can be caused not only by systematic overeating and alcohol, but also by hormonal imbalances in the body, diseases of the gallbladder and duodenum, as well as incorrect use of certain medications.

Fasting during exacerbation of the pancreas is a prerequisite for relieving inflammation
When an attack occurs, you must first refuse any food and drinks except plain water. Such restrictions are explained by the fact that the entry of foods into the digestive system causes the production of enzymes and even greater irritation of the pancreas.
Therapeutic fasting should continue for at least 24 hours. You need to get out of it gradually, and first eat unsweetened crackers, and then introduce dietary dishes into your diet. It is recommended to drink still mineral water; Narzan and Borjomi are especially useful for pancreatitis.
To relieve pain, you need to sit and lean forward. You should not lie down, especially in the first hours after the onset of an attack, as this will cause an increase in symptoms. A cold compress - a heating pad with ice or a bag of frozen food from the refrigerator - will help reduce inflammation. It is better to apply them to the back, just above the lower back, and first wrap them in a towel.
Attacks are often accompanied by severe nausea and vomiting, which brings some relief, albeit temporary. Emptying the stomach from its contents helps relieve the pancreas. Therefore, when gagging, you can speed up the process by pressing two fingers on the root of the tongue.
During an exacerbation of the pancreas, a person needs complete rest, physical activity and sudden movements are excluded in order to reduce the intensity of blood flow in the gastrointestinal tract.
It should be remembered that treatment for exacerbation of pancreatitis should be carried out in a hospital setting, since there is a threat not only to the health, but also to the life of the patient. In some cases, the exocrine function of the pancreas increases significantly, which causes increased production of enzymes.
An excess of enzymes is dangerous because they begin to corrode the gland and can enter the systemic bloodstream. As a result, the functioning of all organs and systems, including the respiratory and cardiovascular systems, is disrupted.

In the hospital, the patient is examined using modern diagnostic equipment, and based on the conclusion, therapeutic measures are carried out
In this case, independent and alternative treatment will not only be useless, but can harm the body and aggravate the condition. Therefore, you should call an ambulance when the first signs of inflammation of the pancreas appear.
Before the arrival of doctors, it is prohibited to take any medications except antispasmodics. Enzyme preparations, analgesics and non-steroidal anti-inflammatory tablets are strictly prohibited. Restrictions even apply to the amount of liquid consumed - you can drink water every half hour, but no more than 50-70 ml at a time.
Drug therapy
Treatment in a hospital is aimed primarily at relieving spasm and pain. For this purpose, antispasmodics and analgesics are used:
Enzyme-containing drugs, such as pancreatin, compensate for the deficiency of substances produced by the gland.
If there is an excess of enzymes, inhibitor drugs are prescribed that inhibit the action of the pancreas, such as Famotidine, Gordox, Contrikal, etc. Inhibitors are used to prevent the destruction of gland tissue by its own enzymes.
Effective treatment of chronic pancreatitis with drugs that will fight the disease and will not cause hormonal imbalances and dysfunction of other organs can only be prescribed by a qualified therapist or gastroenterologist.
Attention! Self-medication with such drugs can lead to serious problems.

Medicines should be taken only as prescribed by a doctor
How does the treatment work?
An emergency doctor installs a drip with saline solution. He administers an antiemetic - Metoclopramide, an anesthetic - Ketorolac, an antisecretory - Kvamatel.

The patient is immediately taken to a medical facility, since exacerbation of the pancreas can only be treated in an inpatient setting.
First of all, to make an accurate diagnosis, indicator and pathogenetic biochemical tests and ultrasound are required.
When the pancreas is inflamed, amylase activity increases in the blood and urine, and on the echogram there is a noticeable decrease in the echogenicity of its tissues and the accumulation of effusion inside the omental bursa, due to which a lumen is formed that is unusual for a healthy gland.
In some cases, to establish the form of the disease, laparoscopy is required - a diagnostic operation in which internal organs are examined through small incisions in the abdominal cavity using a special device: a laparoscope.
In a hospital, the attending physician prescribes complex therapy taking into account individual characteristics and the course of the disease. The following medications are common to all types of inflammation:

- Saline solution in combination with Contrikal and Reopoliglucin.
- Diuretic. The attending physician prescribes the drug that is most suitable for the patient in his condition.
- Antisecretory. Kvamatel or its analogues.
- Antispasmodics. Most often, No-Shpu is used intramuscularly.
- Antiemetic. Metoclopramide is taken until vomiting stops completely.
- Painkiller. Ketorol, Ketonov.
- Antibiotics. In each specific case, the specialist selects them individually.
- To restore the functioning of the digestive system, Festal or its analogues are prescribed.
- Vitamins of group B and C.
- In the event that the body is weakened and eating food is not yet possible, parenteral nutrition is used. Alvezin and Aminosol protein mixtures are often indicated.
Since the number of forms of pancreatitis is quite large, the treatment strategy will be individual in different cases. Sometimes conservative measures are not enough and surgery is required.
Folk remedies for exacerbation of chronic pancreatitis
Attention! You should not use the method described below if the exact diagnosis is unknown!
Suddenly worsened chronic pancreatitis can be calmed with medical cups that were used to treat colds. The jar is lubricated with alcohol from the inside and set on fire, immediately placed in the pancreas area from the lumbar region, but so as not to get on the kidneys, or from the abdominal region. The jar should fit tightly.
After a minute, the jar is removed, and the place where it was installed is smeared with alcohol and covered with a thick towel or woolen scarf. After this procedure, you cannot go outside for the next 2 days.

Banks came to our medicine from China. They have been used for a long time to treat bronchitis and pneumonia.
Diet for exacerbation of chronic pancreatitis and acute pancreatitis
A person living with this diagnosis must realize that the cure for the disease will depend, first of all, on diet and diet. Therefore, in addition to taking medications, in case of exacerbation of chronic pancreatitis, fasting is prescribed for 2-3 days, depending on the severity of symptoms, and then dietary nutrition.
It is necessary to exclude fatty foods and everything fried. You should limit your salt intake to 3 g per day, or it is better to eat without salt at all, replacing it with soy sauce. Cold and hot, spicy and sour are also not allowed. In case of illness, the first table is indicated. All food is steamed: porridge (preferably buckwheat), cutlets, potatoes. It is better to eat little by little, but often: about 5 times a day, provided that you eat at the same time every day.
Important! Unsystematic nutrition often causes gastroenterological diseases and catastrophic weight changes.

Healthy food is the key to a speedy recovery of the digestive system
If symptoms of exacerbation of chronic pancreatitis occur, treatment should begin immediately. The symptoms of the disease are similar for most people, but there are atypical symptoms that can be confused with angina. The causes of the disease can only be determined by undergoing a full laboratory examination, so trying to independently establish a diagnosis is a high risk of error and, as a result, ineffective treatment. Exacerbation of pancreatitis is treated with both medications and folk remedies.
People who do not have bad habits and regularly eat healthy foods are much less likely to develop pancreatitis.
Pancreatitis brings quite a lot of trouble to a person who has this diagnosis. In chronic cases, it is necessary to constantly follow a diet and take medications. An exacerbation of the disease requires immediate medical intervention. What is celiac disease read on this page

Exacerbation of pancreatitis can be caused by stress
Causes of exacerbation
Exacerbations of pancreatitis may occur for the following reasons:
- Poor nutrition:
- Binge eating
- Non-compliance with diet
- Uneven nutrition, fasting
- Nervous feelings, stress.
How long does the exacerbation last?
An exacerbation of chronic pancreatitis, on average, lasts about a week. In some cases, this disease develops into recurrent pancreatitis and can last for years. The pancreas recovers very slowly, so you must strictly follow the diet and take enzymes, and follow all the doctor’s recommendations. Read about the reasons for the development of pancreatitis here: https://jeludokzone.ru/podzheludochnaya-zheleza/bolezni-pz/pankreatit/obzor-prichin-razvitiya-pankreatita.html
The first signs of exacerbation of pancreatitis:
- abdominal pain radiating to the back
- bitterness in the mouth
- vomiting bile
- frequent stools, loose and fatty
In such a situation, you should not self-medicate; urgent hospitalization will help cope with the exacerbation.
Neglect of hospital treatment or taking prescribed medications leads to greater damage to the gland tissue, complicating the further course of the disease and its treatment.
Exacerbation during pregnancy
Chronic pancreatitis, in itself, with the exception of the acute form of the course, is not a contraindication to conception and gestation. With a disease such as pancreatitis, you should plan your pregnancy for a period of stable remission and do not forget about following a diet. However, even with strict adherence to the diet and doctor’s recommendations, an exacerbation of the disease may occur. Read how long an attack of pancreatitis lasts and how to relieve pain.
During pregnancy, self-medication is unacceptable. If you experience any symptoms that cause discomfort, you should immediately seek medical help. The symptoms of exacerbation of pancreatitis in a pregnant woman are similar to the standard symptoms in adults.
What to do in case of exacerbation?
During exacerbation of pancreatitis, it is important to relieve pain. And implement several changes in your lifestyle to prevent an increase in relapses:
- You need to change your diet to the most gentle one possible, eat cereals, low-fat soups, baked fruits, and dietary beef.
- Break your meals into smaller portions and eat a little more often.
- Apply cold to the left hypochondrium
Antispasmodics and enzyme preparations must be on hand.
If they have not been prescribed to you yet, be sure to contact a gastroenterologist.
If an exacerbation of chronic pancreatitis occurs, you should immediately stop irritating the gastrointestinal tract and exclude food for the first two days.
- Drink still mineral water or unsweetened rose hip decoction.
- On the third day, you can introduce jelly and slimy soups and porridges into your diet.
- Eliminate solid foods for a week or even two.
In case of exacerbation of chronic pancreatitis, inpatient treatment is recommended to relieve pain. Antispasmodics and drugs that reduce gastric secretion are prescribed.
Treatment in the acute phase
With this course of pancreatitis, hospital treatment and bed rest for at least two days should be prescribed. You can get by with diet No. 5p, or prescribe fasting with plenty of fluids. Subsequently, fractional meals are prescribed up to 6 times a day in small quantities. Read what reactive pancreatitis is here: https://jeludokzone.ru/podzheludochnaya-zheleza/bolezni-pz/pankreatit/reaktivnyj-pankreatit-simptomy-lechenie-i-dieta.html
Slimy soups and porridges, vegetarian soups and water porridges are acceptable from the menu.
First of all, it is necessary to relieve pain (antispasmodics and analgesics are prescribed) and create functional rest for the stomach (provide abundant alkaline drinks).
Medicines for exacerbation of pancreatitis:
- The course of treatment also includes inhibition of proteases and kinins; the drugs are administered intravenously.
- In the future, it is necessary to eliminate the swelling of the pancreas; diuretics are prescribed.
- Then you should start restoring vascular microcirculation with the help of heparin and antiplatelet agents. Correction of exocrine insufficiency is carried out using multienzyme drugs.
- If a concomitant inflammatory process is detected, anti-inflammatory drugs and antibiotics are prescribed.

Dietary nutrition for pancreatitis is the basis on the path to remission
In case of exacerbation of pancreatitis, treatment at home is unacceptable, since in 10% of cases this disease is treated through surgery when organic changes in the stomach are diagnosed.
Anti-inflammatory drugs that can be taken during an exacerbation:
Pictured are Pancreatin tablets
Diet during exacerbation
Since this disease is subject to hospital treatment, a diet for exacerbation of chronic pancreatitis is prescribed by a doctor. The menu for this diet is called table No. 5p. For the first two days, food is excluded, plenty of fluids are recommended - mineral waters such as "Borjomi". In the future, gradually expand the table with gentle dishes.
Everything that can be eaten during exacerbation of pancreatitis is recommended for daily use by patients. These dishes will only be useful for normalizing digestion. During exacerbation of pancreatitis, you should drink alkaline mineral waters, jelly and rosehip decoction.
Watch a video about how to treat an attack of pancreatitis:
Exacerbation of pancreatitis can be triggered by both poor nutrition and psychological stress. Read about the causes of pancreatitis in children on this page
Pancreatitis is caused by self-destruction of pancreatic tissue by activated enzymes. Activation of enzymes that break down proteins and fats occurs in response to inflammatory changes in tissues.
Pancreatic changes in the activity of the pancreas occur as a response to the vigorous activity of enzymes. Excessive enzyme activity develops due to a number of factors:
- Mechanical destruction. It consists of blocking the duct and blocking the outflow of gland juice. Develops due to adjacent diseases of the bile ducts and edema. Injuries are distinguished separately.
- Neuroendocrine disorder. General disorders of the body's hormonal function - fat metabolism, carbohydrate metabolism. Reasons: abuse of fatty foods, alcohol.
- Toxic and allergic disorders. Allergic reactions to systemic drugs, droppers.
Regardless of the factor in the development of pain, a pancreatic attack is often caused by a combination of factors and a negligent attitude towards health.
Traditional methods
Rose hips
When exacerbating chronic pancreatitis, you can use a variety of folk recipes. Tea based on rose hips has proven itself well
To prepare the recipe at home, you will need 3 tablespoons of berries and about 1/2 part water. Mix everything and boil over low heat for 15-20 minutes. Once the healing tea is ready, you can strain it.
Take 100 ml before meals.
Using rosehip tea, you can quickly remove bile, so the recipe is also actively used for cholecystitis.
Buckwheat
The second well-known recipe for exacerbation of pancreatitis is buckwheat.
Preparation: prepare buckwheat in 1/2 liters of kefir. Application: first eat 1/2 of the prepared porridge for breakfast, and the rest in the evening.
Golden mustache
A golden mustache will also help get rid of aggravation .
To prepare, you will need to chop about 3-4 leaves of golden mustache. Then pour 500-600 ml of water into the container. Mix everything well and simmer over low heat for about 10 minutes. As soon as the finished broth has cooled, you can strain it.
Take 2 times a day. Dosage regimen: first drink 1 tablespoon, then increase the dosage to 1/2 cup every day.
Potato
Many patients with pancreatitis noted that the disease can be treated with simple potatoes. Doctors also claim that potatoes have a positive effect on the pancreas. The recipe will help relieve the patient from spasms, and also if there is damage to the mucous membrane, then potato juice has a healing spectrum of action and will quickly eliminate the problem.
To make juice, you will need to grind raw potatoes and squeeze out the juice. You should have about 70 ml of fresh juice. Take 2 hours before meals.
Important! You should not prepare a lot of juice at once, as it loses its positive properties. Therefore, prepare the recipe daily.
Herbal treatment
At home, you can treat an exacerbation with the help of tinctures and decoctions of medicinal herbs.
Let's look at a few recipes that really help eliminate all the symptoms of the disease. Also read: Acute pancreatitis in adults: treatment drugs
First recipe
To prepare the decoction you will need:
- Dill seeds, hawthorn berries: 2 tablespoons each.
- Immortelle flowers, chamomile: 1.5 tablespoons each.
Preparation: all these herbs must be mixed in one container, then pour in a liter of water. Put the broth on the fire, as soon as it boils, remove it and let it brew. Before use, filter through a clean cloth or gauze.
Application: consume the recipe 1 glass three times a day.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
Second recipe
The second folk recipe is complex, since it will require a large number of different medicinal plants.
Ingredients:
- Dandelion root and celandine.
- Violet, but only tricolor flowers.
- Anise seeds and knotweed.
- Corn silks.
Preparation : the indicated herbs must be taken in equal proportions, approximately 2 tablespoons each. Pour into a container and fill with water (liter). Cook on fire for 10-15 minutes. Like all other recipes, this healing collection is also strained.
Application: drink 1/3 glass three times a day before the main meal. Treatment with this prescription lasts 14 days; if necessary, doctors extend the course.
Third recipe
use a decoction of oat grains for treatment at home .
Preparing the decoction is quite simple. First, grind the oat grains and pour boiling water over them. As soon as it cools down a little, you can drink it. Take the prescription for 30 days, strictly on an empty stomach. This recipe helps reduce signs of inflammation and relieve the patient from general symptoms (nausea, vomiting and diarrhea).
Fourth recipe
Tincture from Glebov, which effectively and, most importantly, quickly eliminates all symptoms of pancreatitis.
Prepare a recipe from the roots of burdock, sage, agrimony, dandelion and calendula.
Preparation: take 3 parts each of burdock, sage and calendula herbs, 2 parts each of the remaining ingredients. For better effect, you can also add 2 parts of meadow clover. Mix everything and pour 0.5 liters of boiling water, let it brew. You can infuse the recipe in a closed jar or thermos overnight.
Also read: Blood test for pancreatitis, indicators, types
Application: consume in small portions before meals. Many people now have a question: how much to drink? We will not be able to answer your question, since the dosage of this particular prescription is calculated individually. If you take the decoction incorrectly, serious health complications may occur.
Propolis is another remedy that helps relieve pain attacks and normalize digestion. There is no need to prepare propolis; just chew small pieces. This treatment method is a clear example of homeopathy and is worth trying at home.
Local changes leading to pain
The ducts of the gland close, but the release of enzymes into the food taken does not stop. The active substances are released into the tissue of the gland itself. Enzymes are highly active proteins. The fat-digesting enzyme molecule is capable of breaking down 154 fat molecules. If a small part of the enzymes gets on the gland tissue, it leads to the death of cells and tissues.
Necrosis occurs - acute pancreatitis. During necrosis, enzymes of the tissue itself are released, enhancing the effect of active substances, worsening the outflow from the affected area, increasing the vulnerability of blood vessels. The cycle of chronic pancreatitis closes.
Pain syndrome in chronic pancreatitis
The key process of chronic pancreatitis is the replacement of gland tissue with connective tissue. Sometimes salt compounds, often calcium, settle in the connective tissue, clogging the ducts of the gland (calculous pancreatitis). The closed ducts continue to function, accumulating fluid, forming cysts. When an exacerbation of pancreatitis occurs, dull pain appears in the area under the stomach, increasing after a diet violation. More often, the sensations occur after heavy feasts or an excessive amount of food eaten. This happens due to the expansion of the stomach, pressing on the head of the pancreas, causing spasm, leading to pain. It occurs under the stomach, it feels deep in the abdomen. Depending on the eating disorders, the pain is short-term or becomes permanent.
The pain spreads to the area of the left sternum, affecting the shoulder, spreading to the back. If the disease progresses in the head of the gland, it spreads to the liver area. If the pathology affects the entire organ, the pain encircles.
There is an increase in pain in certain positions of the patient - lying on his back. Becomes weaker when sitting. Instinctively, the patient presses his legs to his chest in a sitting position - with this position the pain weakens.
According to statistics, with chronic pancreatitis, pain is observed in 9 out of 10 patients, and only 1 in 10 pancreatitis is not accompanied by painful sensations.
The attacks may recur. Doctors have created a scale of attacks:
- Type A. Pain lasts up to 10 days, interspersed with long periods without it.
- Type B. Long periods of pain up to 30-60 days. This type is more common in alcoholic pancreatitis.
- Persistent, ongoing pain. It is an indication for surgical intervention and the use of narcotic painkillers.
Folk remedies
The following drugs are prescribed:
- Enzyme agents. Taking medications is aimed at reducing the load on the organ and accelerating tissue repair processes. Enzymes entering the body from the outside stimulate the process of digestion and absorption of food and reduce the load on the digestive organs (Pancreatin, Creon).
- Antacids. These are drugs that reduce acidity. The principle of their operation differs. Some (Rennie) are quickly absorbed and provide instant relief, others are non-absorbable, acting after a certain period of time, but their effect is longer lasting (Maalox).
- Analgesics. Taken to relieve pain. These are antispasmodics Papaverine, No-shpa and others.
- Antisecretory. Necessary for neutralizing acid (Omeprazole, Famotidine).
- Anti-inflammatory drugs help reduce pain symptoms (Diclofenac).
- Agents to reduce secretion (Sandostatin, Octreotide).
- Prokinetics. They are prescribed for painful nausea and vomiting, which often appears during periods of exacerbation. (Cerucal, Motilium).
When an exacerbation occurs, treatment at home cannot be carried out. In case of very severe attacks, it is recommended to call for emergency help. Strong medications for exacerbation of pancreatitis of the pancreas can only be taken in a hospital setting.
To alleviate the patient's condition, it is recommended to stop eating, provide the patient with rest and apply an ice pack to the pancreatic area.
It is not recommended to take any medications before the doctors arrive, but if medical help remains unavailable in the near future, the following remedies are allowed:
- Creon or Pangrol;
- Drovertin, Papaverine;
- Rabeprazole, Lansoprazole.
Alternative medicine is ineffective during an exacerbation of the disease, however, during remission it will be very useful.
Patients who decide to treat the disease with herbs and other non-traditional methods must be prepared for long-term and systematic treatment.
The following herbs are most often used to prepare medicinal infusions and decoctions:
- chamomile;
- dill;
- hawthorn;
- immortelle;
- mint;
- dandelion;
- calamus;
- thyme;
- hop cones;
- corn silk;
- plantain;
- linen;
- kryphea;
- celandine and many others.
It is very important to consult with your doctor before taking any folk remedy, since even plants that are completely harmless at first glance can cause allergic reactions and other side effects.
How long does an attack of pancreatitis last?
The answer to the question of how long an attack of pancreatitis lasts lies in the stage of pancreatitis and aspects of development. Violation of the outflow of pancreatic juice and an increase in pressure in the lumen of the duodenum lead to the reflux of contents into the gland duct. The duct is not designed for this; small breaks occur, into which active bile enzymes from the intestines enter. They activate their own pancreatic enzymes. The process of inflammation and destruction of pancreatic tissue begins.
Pain in chronic pancreatitis varies. Dull infrequent accompanies patients who violate their diet due to illness.
A different type of pain is acute, with intensification, without spasm. Women are more often haunted by pressing pain after eating. According to statistics, in women, pancreatitis is often combined with biliary tract disease. Pain after eating the wrong food goes away after 2-3 hours and occurs in periods with a chronic course.
Treatment of pain due to pancreatitis
The issue of treating pain syndrome in chronic inflammation of the gland is complex; pain and gland disorder have to be treated simultaneously.
The golden mean is observed when the functions of the gland are restored. Favorable conditions are created for the organ through a strict diet and pain relief. After the pain disappears, the inflammatory process in the gland is relieved and treatment is carried out to restore function.
It is necessary to occupy the gland by restoring the outflow of pancreatic juice, then the pain will subside. For these purposes, non-narcotic analgesics and antispasmodics are used in a hospital setting. Good results are observed when using drugs that block choline receptors, using ganglion blockers.
For persistent pain of an increasing nature, analgesics are administered intravenously - novocaine, diphenhydramine, papaverine, combined with saline, magnesium sulfate and ascorbic acid.
In some cases, doctors resort to the use of serious analgesics - tramadol and others. Sometimes the described therapy is replaced by paracetamol with non-steroidal anti-inflammatory drugs. In extreme cases, narcotic analgesics allow the patient to survive until surgery.
Depending on the stage, the pain can last a long time without subsiding. For such pancreatitis, surgical treatment is recommended. An operation is performed to remove part of the gland or duct.
Home remedies to relieve pain
Selected measures can temporarily lull the pain and relieve the symptoms of acute pancreatitis. Conventionally, the measures are called “Cold, hunger and peace”:
- Refusal of food. The minimum time is one day. The measure is due to the need for enzymatic unloading of the gland.
- Apply a cold compress or a bottle of cold water to the navel area to eliminate swelling.
- Water mode. Increasing the liquid to 2 or more liters of warm water.
- Elimination of spasm. Taking antispasmodics.
- Peace from stress. Avoid physical and psychological stress.
The following simple actions ease and relieve pain. It is important to remember that moderation in consuming foods not recommended for pancreatitis will only provoke pain. You should take medications to relieve pain after a specific doctor’s prescription.
Treatment
Exacerbation of pancreatitis requires complex treatment. The main method is a combination of drug therapy and diet. The patient will have to take certain medications and adjust the diet for a long time. Violation of the recommendations will shorten the period of remission and increase the severity of the next attack.
It is permissible to supplement therapy with some folk remedies, but only after agreeing with the attending physician.
Medicines
If pancreatitis is detected, the patient is prescribed certain drug therapy. Additionally, the doctor gives recommendations on the choice of drugs that will help stop the exacerbation of the pathology. Incorrectly selected medications will not only not eliminate the symptoms of the inflammatory process, but can also provoke serious complications.
Examples of medications:
- non-narcotic analgesics (Paracetamol, Analgin);
- agents to suppress secretion (Octreotide, Somatostatin);
- proton pump inhibitors (Omeprazole);
- prokinetics (Motilium);
- antispasmodics (No-Shpa, Drotaverine);
- preparations with enzymes (Creon);
- antienzyme agents (Gordox);
- anticholinergics (Methacin, Atropine).