Reactive pancreatitis in children occurs most often between the ages of 10-14 years, but the disease can appear earlier. The disease is characterized by a strong infectious process, so the child experiences complications from the gastrointestinal tract.
It should be noted that if reactive pancreatitis occurs in a child at an early age, the symptoms are less pronounced.
Recommendations from Elena Malysheva in the special issue “Live Healthy!” on how to overcome pacreatitis using the healing effects of natural remedies.
Symptoms
With this type of pancreatitis, acute swelling of the gland tissue occurs.
This in turn leads to compression of the excretory ducts directly to the pancreas. After this, the child’s outflow of enzymes and pancreatic juice into the gastrointestinal tract becomes difficult. In addition to swelling of the gland tissue, the child also experiences pain. As a rule, the pain with such pancreatitis is girdling in nature, and is localized in the area above the navel. This disease in children is accompanied by general symptoms.
For example:
- The child experiences severe nausea;
- In severe cases of the disease, vomiting occurs. Note that vomit in the reactive form of the disease will contain gastric contents;
- Diarrhea;
- Moodiness and irritability;
- Often the child’s temperature rises to 37-38 C.
A clear sign may include dryness in the mouth, as well as the appearance of a white coating on the tongue.
Note to parents! As soon as your child loses interest in games and all of the above symptoms occur, you should immediately consult a doctor.
In older children, the disease begins with pain. The child may complain of severe pain in the back and abdomen.
Also read: Which doctor treats the pancreas?
The nature of the pain is varied:
- Spicy;
- Aching;
- Wavy.
While a tall child can tell what is bothering him, a baby cannot. Therefore, parental care is needed during this period. As soon as the baby cries for several days in a row, the temperature rises and motor restlessness arises - a reason to visit the doctor.
Diagnostic measures
Impaired functioning of the pancreas is manifested by all the typical symptoms: pain, nausea, vomiting, decreased appetite, diarrhea. In some cases, clinical manifestations may be absent for a long time. But in the future this leads to pronounced changes in the digestive process.
Diagnosis of such conditions presents certain difficulties due to the vagueness of manifestations and minor changes in functional examination methods.
Biochemical blood parameters - enzyme activity (most often amylase). With exacerbation of chronic pancreatitis, the numbers exceed the norm by 3 times. In other cases, this process is so short-lived that it is not possible to determine its increase in the blood.
Coprogram - stool is shiny, greasy, viscous and sticky, “sticks to the pot”, when analyzed it reveals:
- a large amount of fat - steatorrhea;
- undigested muscle fibers - creatorrhea;
- starch grains as a result of incomplete breakdown of carbohydrates - amilorrhea.
The fecal elastase test is the gold standard for diagnosis. Elastase-1 is determined: it does not change when passing through the entire intestine:
- elastase level is not lower than 200 mcg/g;
- moderate deficiency - 200–100 mcg/g;
- severe deficiency - less than 100 mcg/g.
Instrumental research methods.
Ultrasound determines:
- echogenicity of the pancreas;
- resizing;
- clarity of contours;
- the presence of cysts or calcifications.
Tomography (computer, magnetic resonance) gives a clear picture of the structure of the gland tissue, even minor structural changes are accurately determined.
There are a sufficient number of other functional and laboratory studies, but in this case they will be uninformative.
What are the first actions of parents and doctors?
If your child has one of the above signs, you need to call a doctor as soon as possible. Parents should not just wait for the doctor; before his arrival, it is necessary to ensure the child’s peace.
The second stage is for parents to tell all their complaints and notify the doctor about the child’s complete condition.
What should the doctor do?
Of course, first, listen to the parents and conduct a full examination of the child. After this, a referral is issued for laboratory tests, most often a blood test. After all, a blood test can quickly detect whether a child has an inflammatory process or not.
If pancreatitis is suspected based on the first test result, a biochemical blood test is prescribed, which will help determine the level of pancreatic enzymes.
After a laboratory examination, doctors send the child for ultrasound or computer diagnostics. In order to make an accurate diagnosis, laparoscopy is mandatory.
In case of severe illness, the child is hospitalized together with the parent. Treatment of the disease in children is carried out conservatively and under strict supervision.
Diagnosis of pathology
If symptoms characteristic of pancreatitis appear, consultation with a pediatrician and gastroenterologist is necessary.
If the development of the disease is suspected, a number of diagnostic measures are carried out aimed at identifying the severity and form of the disease, as well as to differentiate it from other pathologies with similar symptoms (appendicitis, gastric ulcer, renal colic, cholecystitis).
Diagnostics involves the following procedures:
- examination of the peritoneum by palpation, which allows you to determine the source of pain and draw preliminary conclusions about which organs are affected;
- taking blood samples for a general analysis - this allows us to establish the fact of the development of inflammatory processes, in which the level of leukocytes in the blood increases and the ESR increases;
- sonography (ultrasound examination) of the abdominal cavity (the procedure is used to determine the degree of enlargement of the pancreas and determine the presence of necrotic areas);
- performing CT and MRI.
An additional method for identifying pancreatic dysfunction can be a coprogram. With pancreatitis, accumulations of starch, undigested retina and neutral fats are found in the stool.
Treatment
The therapeutic course includes taking medications. Together with drug therapy, doctors prescribe a diet for the child. If the disease occurs in a breastfed child, then the diet is prescribed to the mother.
Important! The drug is prescribed not only based on the patient’s age, but also on the severity of the disease. Therefore, you should not self-medicate.
The first stage of treatment is taking medications that will help reduce the volume of gastric juice produced; Pirenzepine is most often prescribed in childhood.
Also read: Types and classification of pancreatitis of the pancreas
Festal or Panretin may be prescribed as a pain reliever, as well as to improve digestion. If a child has an allergic reaction, then No-shpa is prescribed. To improve the outflow of pancreatic juice, it is necessary to take antispasmodic drugs, for example Platiphylline. Note that this drug also helps eliminate pain symptoms.
As you understand, with this disease the digestive tract is disrupted, so it is necessary to replenish the body with easily digestible nutritional material. Therefore, doctors at older ages prescribe Glucose drips to the child.
Important! Reactive pancreatitis can also be treated with other drugs prescribed by the treating doctor.
Many people ask, is it possible to cure pancreatitis with traditional medicine ? No, herbal recipes alone will not bring a positive result for such a disease, because it is imperative to take medications and adhere to a diet. If necessary, traditional methods can be prescribed, but only in combination with the main therapy.
Pancreatitis in children: causes
Pancreatitis is a serious disease. In adults, the main causes of this disease are alcohol abuse and gallstone disease. In children, pancreatitis is less common, and the causes are broader and more diverse.
Pancreatitis develops when the bile ducts become inflamed
Pancreatitis occurs when the bile ducts become inflamed and the enzymes produced by the pancreas remain trapped in the pancreas. Bile begins to affect the gland itself, destroying the tissue. Bile is released into the blood, which can cause obstructive jaundice and lead to poisoning of the body.
There are acute and chronic forms. Acute pancreatitis is much less common. The chronic form is more common - it is diagnosed in children aged 7 years and older. In preschool age, cases of pancreatitis are much less common.
In approximately one case out of four, it is impossible to determine the exact cause of the disease.
Possible reasons:
- heredity, genetic predisposition
- blunt trauma to the pancreas (due to a strong blow)
- diseases of the biliary system
- food allergy
- infections (hepatitis, chickenpox, influenza, herpes, etc.)
- medications (metronidazole, furosemide, sulfonamides, tetracyclines, etc.)
- poisoning with toxic substances (lead, mercury, arsenic)
- increased pressure in the bile ducts
- chronic cholecystitis
- parasitic diseases (opisthorchiasis)
Most often, the disease develops against the background of an unbalanced diet of the child (eating fatty, fried, spicy foods) and a violation of the diet.
The correct identification of the causes of the disease will determine how successful the treatment of pancreatitis in children will be.
Proper diet for reactive pancreatitis in childhood
The main goal of dietary nutrition is to eliminate inflammatory changes, as well as quickly restore pancreatic function.
Stages of diets
For the first 3 days, fasting is prescribed. Why? Due to fasting, the child stops secretory activity, thereby ensuring peace of the inflamed organ.
But this does not mean that the child should completely refuse to eat, because otherwise dehydration will occur. Therefore, for the first time, you are allowed to drink water without gas, for example, Borjomi, for 3 days.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
The second stage is a gentle diet, which lasts for 14 days. At this point, adhere to diet No. 5.
The third stage is beyond the exacerbation stage. The duration of the third stage is from 2-3 months, it all depends on the general condition of the child.
Also read: Pancreatitis during pregnancy: what to do
What kind of dishes can you eat?
- Puree soups;
- Rusks;
- Porridge;
- Mashed potatoes.
You can prepare a dish from carrots, beets, cauliflower or pumpkin.
The dangers of poor nutrition
Dr. Komarovsky talks about many diseases in his programs, including pancreatitis. He says : “If we feed a child crap in a beautiful cover, then he wonders where we got diseases from!” .
Therefore, it is important to always adhere to proper nutrition, and not just during illness. According to Dr. Komarovsky, if parents stop adhering to the diet for any type of pancreatitis, then all the symptoms of the disease will worsen. After all, drug therapy must be comprehensive; this is the only way to get rid of the disease.
Now you understand what symptoms children have and what treatment should be given. Remember that treatment is strictly under the supervision of a doctor.
Video on the topic
About children and the pancreas

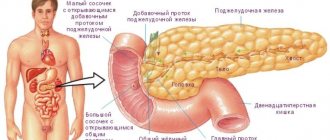
The pancreas is an important digestive organ that lies below the stomach at the level of the final thoracic and initial lumbar vertebrae. It consists of three parts: head, body and tail. In newborns, the organ weighs about 3 g, the length varies from 3 to 6 cm. Until the child is 5 years old, the process of increase occurs intensively, reaching a mass of 20 g. Further development slows down and by the age of 12, a gradual increase brings the weight of the organ to 30 g.
Why does the pancreas enlarge?
In a child, changes in the size of the head of the pancreas have the following reasons:
- abscess;
- cystic adenoma;
- pseudocyst;
- malignant tumor;
- scar of the small intestinal papilla;
- blocking of the excretory glandular duct with a stone;
- a tumor on the duodenal papilla that does not allow the release of pancreatic secretions;
- an additional excretory duct in the head, formed due to duodenitis and inflammation of the minor papilla of the duodenum.
The tail of the pancreas also changes its size due to the influence of various factors. Doctors find the cause of the anomaly in a pseudocyst that affects the gland during acute pancreatitis. A pseudocyst is a modified area with sterile contents and walls formed from glandular tissue.
The pancreas becomes enlarged in a child due to intestinal tumors and scars, cystic adenoma, and purulent accumulations. The baby is plagued by colic, vomiting, and diarrhea.
Serious reasons for the fact that the tail has become enlarged in a small child may lie in malignant neoplasms. Reaching large sizes, disintegrating or causing hemorrhages, tumors cause local swelling of the digestive organ.
The glandular tail may have the following causes of growth and inflammation:
- stone in the Wirsung duct;
- pancreatic abscess, or purulent tissue in the capsule;
- cystic adenoma is a benign tumor developed from glandular structures.
The reasons for abnormal enlargement of the pancreas when the body is relatively healthy are also parental omissions. For example, a mother strives to feed her child, but the diet is incorrectly formulated or the baby eats food with additives and artificial substances. Distortion of the composition of enzymes and the size of the organ occurs against the background of gastrointestinal motility disorders, gastritis, abdominal injuries and current viral-bacterial diseases.
How to understand that the pancreas is enlarged?
The main symptoms of an enlarged digestive organ in a child are:
- increased body temperature;
- refusal to eat due to nausea, bitterness in the mouth, vomiting;
- aching or burning pain, radiating to the lower back, right arm;
- localization of discomfort in the upper abdomen;
- weakness, pallor, weight loss;
- stool disorder (diarrhea without mucous and bloody inclusions).
In the diagnosis of glandular pathology, such a sign as the “pancreatic triad” is important. This means that proteins, fats and carbohydrates not processed by iron change the consistency of stool. The products of defecation become liquid and greasy, and a film is visible on their surface. The feces are poorly washed off and give off a foul odor.
When the gland is inflamed, all symptoms increase gradually. In the case of the development of a tumor or cystic element, signs of pathology appear much later, after a long period of time from the initial changes. Therefore, at the slightest suspicion of problems with the baby’s gland, you should show it to a specialist and undergo an ultrasound.
An overgrown tail and head of the pancreatic structure are dangerous changes. They exert compression on nearby organs. The abnormally enlarged head puts pressure on the child's duodenum. The consequence of this exposure is intestinal obstruction.
How to return the gland to normal size?
What to do, how to help your baby when pathological signs appear? First, you need to show him to a gastroenterologist, and before going to the clinic, transfer the baby to a hydro-diet with drinking mineral alkaline water. To relieve pain to the left of the navel, you can apply cold. If a child complains of acute unbearable pain, you must call an ambulance.
Doctors suggest a conservative or surgical treatment regimen for the altered gland. The general principles of therapy to restore the size of the organ come down to the following measures:
- inhibition of secretory activity by proton pump inhibitors, histamine receptor blockers and hormonal substances;
- reducing swelling by applying cold heating pads;
- correction of organ function with artificial digestive enzymes;
- transferring the baby to parenteral nutrition, when the body receives nutrients through injections;
- surgical intervention if it is necessary to eliminate the inflamed focus or dead tissue.
Restoring gland size with diet
The Pevzner diet No. 5 helps children achieve recovery. Its main principles require maximum limitation of fatty foods and any fatty ingredients in dishes. It is recommended to replace them with protein components - they improve the condition of the diseased organ.
In order for the tail and head to normalize their parameters, the following products are removed from the children's diet:
- juices;
- jam, chocolate, ice cream;
- raw vegetables, herbs, fruits;
- fatty dairy foods (whole milk, cream, sour cream);
- rich meat broths and dishes prepared from them.
During the period of treatment of the digestive structure, Komarovsky reminds of the importance of steaming and boiling foods. The doctor advises boiling porridge in water, steaming vegetable stews, and baking fruits. A child can drink black tea, but with a minimum of sugar. For baked goods, you are allowed to eat biscuits, crackers, and dried bread.
If neoplastic processes occur in the baby’s body, it is not advisable to use diet alone as treatment. A tumor in the gland can only be removed surgically. During the rehabilitation period, the importance of a properly formulated diet comes to 1st place, since the affected organ needs to reduce the load.
How to treat the gland with folk remedies
The simplest folk treatment for pancreas is to drink potato juice. A couple of tubers of the pink variety are thoroughly washed and ground together with the skin. Squeeze the juice out of the pulp and give the child 2 rubles. a quarter of a glass per day. After another 5 minutes. They suggest drinking a little kefir. The general course of juice therapy is 2 weeks. Then they take a 7-day break and continue to feed the baby potato juice.
Children love sweets. For the pancreas, this addiction is used by teaching the baby to eat 1 tsp in the morning. honey It is useful to drink the beekeeping product with warm milk (half a glass). If a child suffers from allergies or diabetes, feeding him honey for medicinal purposes is prohibited.
Licorice preparations are often used in the treatment of children 2–3 years old. When the baby's gland is enlarged, 1 tsp. Healers advise combining dry roots of the plant with the roots of burdock and dandelion (5 g each). The collection should be infused in half a liter of boiling water for about 3 hours. The herbal medicine is given to the child in a moderately hot form 4 times a day. half a glass a day. The product normalizes the production of pancreatic substances.
Our specialist comments
- If the enlargement process has affected the pancreas due to acute pancreatitis or abscess, do not refuse to place the baby in the surgical department. There he will be successfully treated with both conservative and surgical therapy.
- The urgency of excision of a pseudocyst identified on the gland should be agreed upon with the surgeon. In some cases, the pathological area is left and forced to resolve with the help of medications.
Diseases and pathologies of the pancreas
The complexity of all problems with the pancreas is partly related to its special location. It is located in the center of the abdomen, and, unlike other organs of the digestive system, is located retroperitoneally. Therefore, it is not accessible to palpation, which makes it difficult to diagnose the pathology associated with it. Large gland sizes are detected using functional methods. But it is impossible to make a diagnosis based on the fact of its increase alone: it can be a manifestation of a developmental abnormality or arise under external influence, without being pathological. Such pancreatomegaly does not pose a threat to the health and life of the child.