What's happened
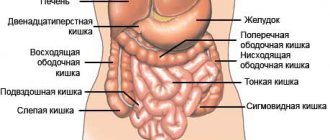
Cecal cancer is a low-quality tumor that begins its development from mucosal cells. Most often, the location of the tumor is observed at the junction of the small and large intestines.
Pathology is diagnosed in 10-20% of cases of all colon cancers. More often, the pathology occurs in people after 45-50 years of age, and is observed with equal frequency in men and women.
The first symptoms are quite difficult to independently determine, since they can differ depending on the location, size of the cancer node, and concomitant pathologies. Often the symptoms resemble those of hemorrhoids.
On this topic
- Oncogastroenterology
Feces for stomach cancer
- Natalya Gennadievna Butsyk
- December 6, 2020
The disease is characterized by moderate growth and slow spread of metastases, and the formation of secondary tumors is observed mainly in advanced stages of the pathology; distant organs and tissues are not affected.
Cecal cancer belongs to the moderately aggressive diseases; the prognosis directly depends on the timely diagnosis and implementation of therapeutic measures. With a very favorable prognosis, we can talk about complete elimination of the disease and restoration of all body functions.
Symptoms
Symptoms in the presence of a cystic growth depend on the location of its formation, type and size. Most often the disease occurs on:
- Sigmoid colon.
- Rectum.
The following organs are rarely susceptible to this pathology:
- Small intestine.
- Mesentery.
- Posterior wall of the abdominal cavity.
Local symptoms
If the node is small in size, it does not cause significant symptoms. Discomfort in the abdomen and other parts of the body appears as the tumor grows. As a rule, the following is observed:
- Colic (minor cramping pain).
- Flatulence, uncontrolled release of gases.
- Digestive disorders (constipation, diarrhea).
- Feeling of heaviness.
- Blood in the stool.
- Abdominal bloating.
- Frequent urge to defecate and urinate (to no avail).
- Pain in the perineal area.
- Modified stool (in most cases it is thin).
Any symptom listed is a good indication for visiting a doctor.
General symptoms
General signs of illness occur in the case of an inflammatory process or suppuration of an intestinal cyst or its membranes.

Cystic formation of the intestine
- Painful localized beating in the area of the node.
- Apathy.
- Nausea.
- Weakness.
- Drowsiness.
- Significant increase in body temperature.
- Aches.
- Headache.
- Dizziness.
In most cases, when the cyst shell spontaneously breaks through and its contents are released into the abdominal cavity, the general condition of the body returns to normal. When complications occur, fistulas or open cavities form.
Classification
ICD 10 code for cecal cancer C18.0.
Several classifications of cancer have been identified. According to histology, the following are distinguished:
- Adenocarcinoma - development begins from the cells of the colon mucosa.
- Signet ring cell carcinoma is detected in the form of vesicles.
- Squamous - the neoplasm consists of squamous epithelium.
- Glandular-squamous - the composition includes jelly-like, flat epithelium.
- Undifferentiated – characterized by increased aggressiveness, difficult to treat, and has a poor prognosis. The patient's condition is rapidly deteriorating.
- Unclassified - the composition includes cells that are not related to recognized histological forms.
Pathology has several stages of its development.
0 degree
In another way, this degree is called a precancerous condition. The upper layer of the intestinal epithelium is damaged, nearby lymph nodes are not affected, and there are no metastases. Characterized by small size.
Stage 1
The abnormal process extends to the next layers of the cecum, but does not affect the outer layer of the intestinal wall. No metastasis is observed.
Stage 2
The lesion affects all layers of the intestinal wall, metastases are not observed, and the lymphatic system is not affected. The prognosis for survival can be assumed based on the degree of spread of the pathology along the outer wall, but more often it is favorable.
Stage 3
The growth of the tumor to regional organs and tissues is observed, the lesion affects the lymph nodes - lymphoma. The prognosis for survival is about 5 years. Distant secondary tumors are not observed.
Stage 4
The terminal and last stage is characterized by serious damage to organs and tissues, lymph nodes. The prognosis at this stage is often unfavorable - the patient may live less than five years.
Causes
The true causes that can cause a low-quality tumor of the cecum are still not fully understood, and there are still disputes among scientists today. Some predisposing factors are reliably known.
Harmful production
With a long period of work in hazardous work, the risk of developing cancer increases significantly.
It is unfavorable conditions that cause the degeneration of cells in the cecum; for this reason, the mutated elements cannot perform the functions of healthy cells and gradually die.
Chronic diseases with non-malignant tumors
In the presence of chronic forms of diseases in the organs of the digestive system, cancer of the cecum is formed much more often.
Ignoring such diseases without treatment leads to the degeneration of cells into cancerous structures. In recent years, a similar cause has been increasingly identified in patients.
Age-related changes
In most cases, the disease is detected in people over 50 years of age; it is at this time that cell regeneration and some important processes in the body are inhibited. In addition, as people age, they tend to accumulate harmful compounds, which can also cause cancer.
Hereditary predisposition
If close relatives have had cancer of the gastrointestinal tract, the risk of developing pathology of the cecum increases. In such cases, it is necessary to carefully monitor your own health from the digestive system.
Diet
An incorrectly selected diet can cause cell mutation in the cecum. If you prefer animal products, especially fried ones, your chances of developing the disease increase.
This occurs against the background of the fact that the body regularly enters a large amount of fats, the breakdown of which will take time.
Colon cancer: stories from an oncoproctologist
“I also ask these questions myself,” the oncologist confesses. – You need to start with yourself, how ready you are to undergo a colonoscopy. not everyone can show the doctor the causative site (anus - author's note This is a definite problem for timely treatment. As a result, we are often faced with late presentation of patients and advanced forms of oncology. Indeed, with stage 1, recovery is possible in 90 percent of cases, and with stage 4, survival up to 5 years, according to our data, is achieved only in 20–25 percent of cases.
We need to somehow encourage people to undergo such examinations. Because both in developed countries and here in Kazakhstan, the incidence of colorectal cancer is increasing every year. Among the reasons are physical inactivity, poor environment, alcohol, smoking, unhealthy diet, a lot of refined fatty foods, fast food.
For example, when red meat is digested, unlike white meat, the intestines produce toxins and carcinogens that contribute to the formation of malignant tumors of the colon. Why examine the intestines?
And this is the kind of data that flows into KazNIIOiR from all over the republic: in 2006, 2,328 patients with colorectal cancer were identified in the country. In terms of ranking and incidence rate, it was in 5th place. And 11 years later, in 2020, 3,131 such patients were already identified. The incidence increased by 800 people, or 30 percent! And in terms of ranking, this type of oncology rose up after lung cancer, breast cancer in women and prostate cancer in men.
What are people afraid of?
- Of course, when the need arises, a person willy-nilly runs to us! If you already have abdominal pain, spotting, have lost weight, etc. But this, as a rule, is far from the initial stage, but the terminal stage, a borderline state between life and death,” continues Marat Kuzikeev. – Screening for colon cancer in our country has been carried out free of charge in clinics at the place of attachment since 2011. For 8 years.
It includes two points. The first is a non-invasive, painless FOB-N test, a fecal occult blood test . Moreover, everything is done very hygienically: the rod is removed from the plastic bottle. It is immersed in the subject's morning stool, then returned to the tester's cylinder with the solution. Then the tester bottle is opened from the back and the resulting solution is dripped onto the tablet. The procedure can be compared to a pregnancy test. After waiting 3-5 minutes, look at the tablet. If one stripe appears on it, everything is fine. If there are two, then you need to urgently run to the doctor and undergo a fibrocolonoscopy, since there is a possibility that the tumor is bleeding.
A colon tumor is a growth on the mucous membrane. When feces pass through the intestines, they begin to tear off part of the tumor purely mechanically, and blood is released. This is determined by the FOB-N test.
- What's so scary about that?
– There is such a device in the form of a probe or flexible tube, which is inserted through the anus into the lumen of the large intestine and penetrates to its end, to the cecum . This is the second stage of screening. The probe is hollow inside. And through its lumen, certain instruments can be introduced to verify the formations that are in the colon and remove them. At the end of the probe there is a camera and a lighting lamp. A visual inspection of the entire colon cavity is performed. If any changes are detected, they are recorded, and biopsy material is removed with forceps. If there are polyps, they are removed by cauterization with electric current . That is, thermocoagulation of polyps occurs, their cutting and bloodless removal.
– It turns out that both examination and partial treatment are carried out in one visit?
- Yes. In much the same way as examining the stomach or performing a coronary angiography. Only when treating heart vessels, a conductor, through which either a stent is inserted or other manipulations are performed, is inserted through the lumen of the artery. And here the probe is inserted through the lumen of the colon.
– So simple that you shouldn’t even be afraid?
- Absolutely not worth it. True, those who received such a procedure noted some pain. Unpleasant sensations occur when the peritoneum inflates with air. But all this is tolerable! I examined myself, and at the same time checked how my patients felt.
What is a polyp, where does it come from?
“A polyp is a benign tumor on the inner wall of the intestine,” explains Dr. Kuzikeev, “which can potentially degenerate and turn into cancer within 5 years. Therefore, if we remove this benign tumor at the very beginning, we will save the patient from the possibility of developing colon cancer in the near future. It is impossible to do such prevention against lung or pancreatic cancer, even if you follow a diet and don’t smoke.
There it is generally unknown what the tumor grows from, but here, by removing the polyp, we will protect a person from colon cancer! Such a direct dependence.
And the more often we perform colonoscopies, the fewer people we will have with colon cancer. Since it is polyps that 98 percent lead to colorectal oncology . And anal fissures and hemorrhoids account for only two percent of the likelihood of this type of malignant tumor.
– Can there be many cancerous foci?
– In my practice, I saw 4 types of cancer simultaneously in one of the patients. Vulvar cancer, cervical cancer, sigmoid and transverse colon cancer. This happens when the immune system is deeply damaged. We operated and cured this woman. Now she is being observed. Age somewhere between 50–60 years. Among the reasons, as far as I remember, was the factor of psychogenic trauma.
In the presence of some kind of shock, stressful situations, such as the death of a relative or the loss of a favorite job, under difficult circumstances, it happens that after 3-6 months a malignant tumor is discovered in patients.
It's very scary when children get sick. We had one girl. When I operated on her, she was 17 years old. Very pale, anemic. She had advanced colon cancer that had already spread to nearby organs. The operation was a large combined one. Where did it start? There was no pain, since there are almost no nerve receptors inside the large intestine . But she was losing weight and turning pale. The adults thought maybe she had overextended herself in her studies and didn’t pay attention. But the main thing is that her mother died at the age of 40 from cancer, also of the colon. This is how heredity manifested itself in a child!..
“We operated on the girl,” the doctor continues. “We had to remove not only the tumor itself, but also the ways it spread throughout the body. In her case, it was necessary to perform another resection of part of the bladder.
Cancer is more insidious - it, like rust, eats through everything. And organs, and blood vessels, and bone tissue.
But she was lucky that there were no distant metastases and lesions of the lungs and liver. If this happened, the prognosis for life would be completely negative.
– Could she have died within two or three months?
- Yes. But we helped this girl. Therefore, we feel great satisfaction from our work. After all, when you operate on a child, everything is much more emotional than with adults. Soul and body against cancer
And we had a grandmother, 91 years old. Elderly people have other problems. They have damage not only from the organ itself - the colon, but also from the heart, lungs and much more. By this age, the entire body wears out. And operating is a big risk. But we took a chance, cut out the tumor, sewed up parts of the colon, and she now goes to the toilet safely naturally . It is very dangerous to perform such reconstructive operations on older patients. But everything went well for us, we are happy. Although even in the last century there was talk about the feasibility of such operations. And such cases were most often left to chance.
What am I talking about? Moreover, it is now possible and necessary to undergo surgery and treatment for colon cancer at any age. And be sure to undergo screenings, especially after 50 years.
-Did you pass?
– Yes, although I am only 47. The age for screening is 50–70 years old, when this disease is at its peak. But since I demand and convince people to get a colonoscopy, I should experience it myself. And it passed without pain relief. Handled it well. Now for 3-5 years I will have peace of mind that I don’t have colon cancer. And then, perhaps, I’ll go through some more. In medicine there are certain rules that must be followed, then you will live happily ever after!
– In Europe and America, are patients more disciplined than ours?
– There are also many neglected cases there. That is, it’s not just us who are afraid of colonoscopy. But in Japan the situation is different. There, this procedure, like the examination of the esophagus, stomach and duodenum, is mandatory even when applying for a job. This is their state program for the early detection of oncology and the improvement of the nation. Therefore, colorectal cancer is detected mainly in the early stages.
In our country, so far, even less than a hundred people came to KazNIIOiR in Almaty for a free examination on an open day both last year and this year! And this is for the entire city of two million!
ALMATY
Symptoms
Cancerous tumors that form in the cecum are characterized by a long asymptomatic course. Characteristic symptoms can only be identified in the final stages, when the disease is already in an advanced form and is very difficult to treat. However, even when a clinical picture appears, without diagnostic methods it is impossible to determine the location of the tumor.
First symptoms
Symptoms intensify as the tumor grows. First, the patient complains of nausea, vomiting, and frequent belching.
In addition, appetite worsens, regular bloating is observed, constipation appears for no reason, which is replaced by diarrhea. Abdominal pain on the right side also appears.
Further symptoms
As the cancerous node grows, traumatization by feces increases, which becomes the cause of bleeding. At first they are hidden and may not be noticed, then anemia develops.
Signs of asthenia appear:
- General weakness, increased fatigue.
- instability : apathy, irritability, poor sleep.
- Earthy color .
- loss .
During defecation, the discharge of bright red blood is observed, but this symptom is typical for neoplasms of any part of the intestine.
Symptoms of the thermal stage
At the last stage, the following signs appear:
- Severe pain - appears due to pressure of the tumor on regional organs and tissues.
- Intestinal obstruction - can be partial or complete.
- Yellowness of the skin.
- Liver failure - metastases enter the liver by lymphogenous and hematogenous routes, affecting it.
If primary symptoms occur, you should immediately consult a doctor; such a measure will make it possible to quickly diagnose the disease and begin its treatment, without starting it to the thermal stage.
The liver is a vulnerable organ
Most often, the tumor affects the liver, since this organ is directly involved in hematopoietic processes, passing through itself up to 2 liters per minute. Through the venous artery, blood enters it from the following organs:
- intestines;
- pancreas;
- spleen;
- gallbladder.
Cancer of the cecum and sigmoid colon is almost always accompanied by lesions in the hepatic zone, which are characterized by severe pain in the abdominal area.
The gallbladder is adjacent to the liver and collects bile leaving the hepatic ducts. Gallbladder cancer leads to blockage of the ducts and damage to the main organ by cancer cells. Diagnosing a malignant bladder tumor is quite difficult. It is asymptomatic in the first two stages. The first signs of the disease, as well as obstructive jaundice with a number of distinctive properties, develop when gall bladder cancer has taken root in the liver.
The pancreas is located next to the liver area. These organs produce the necessary amount of enzymes for digestion. The diagnosis of pancreatic cancer with liver metastases is often detected at an advanced stage of the disease, which complicates the patient’s recovery.
Less commonly, stomach or lung cancer causes further liver damage, although it is much easier to recognize the disease in the early stages with these pathologies. Lung cancer with liver metastases occurs when the main organ is almost affected.
Diagnostics
To make an accurate diagnosis, it is necessary to carry out a set of measures. To begin with, the doctor collects a complete medical history of the patient, examines the patient and palpates the rectum.
The abdominal cavity is tapped and the resulting sound phenomena are analyzed, which makes it possible to determine the presence of free fluid. Palpation of the abdomen sometimes makes it possible to determine the location and condition of the node, and sometimes it is possible to detect the presence of metastases.
If a splash of liquid is detected during listening, this directly indicates the formation of intestinal obstruction.
Endoscopic examination
The doctor prescribes a series of tests.
Colonoscopy
The manipulation is painful, so it is necessary to perform anesthesia before performing it. It is carried out using a colonoscope - an optical device.
The method makes it possible to determine the size of the pathological node, its location, and assess the condition of the mucous membrane of all parts of the intestine. The manipulation is characterized by taking a biopsy for histological analysis. Prescribed in cases where other diagnostic measures have not given accurate results.
Sigmoidoscopy
The condition of the rectum is assessed using a sigmoidoscope. The technique reveals the location of the tumor and the extent of damage.
Irrigoscopy
X-ray analysis of the loops of the ileum and colon. The patient is first given an enema, which is designed to fill the entire intestine with a contrast agent. Irrigoscopy makes it possible to determine the diameter of the lumen, the size of the tumor and its growth beyond the cecum.
Additional diagnostic measures include magnetic resonance imaging, computed tomography, and ultrasound analysis of the abdominal cavity; they can be used to determine the presence of a tumor and the presence of regional and distant metastases.
Treatment
Therapy for a malignant cecal node involves a combination of therapeutic methods such as surgery, radiotherapy, and chemotherapy.
Surgical intervention
Surgery is the main method of treatment for any type of cancer; its scale depends on the stage of development of the disease and the location of the cancer node. Based on the results of the examination, resection, application of anastomosis by connecting different parts of the large intestine, and excision of the tumor can be performed.
Lymph nodes that are affected by the tumor are removed. If for certain reasons surgery is not possible, then an artificial anastomosis is performed, bypassing the affected area.
Radiotherapy
The therapy method can be prescribed before and after surgery. This measure makes it possible to reduce the size of the formation, destroy abnormal cells, and reduce the risk of relapse.
Chemotherapy
The use of drugs is aimed at reducing the tumor, also blocking the uncontrolled division of mutated cells as much as possible, and inhibiting metastasis. The method is often combined with radiotherapy.
Therapy
Treatment methods for this pathology depend on the symptoms and type of disease. But it is worth considering that complete removal of the cyst is only possible with surgical intervention. This method is especially effective for acute complications and malignant tumors.
For cancer, in addition to surgical removal of the tumor, chemotherapy is used. This procedure is carried out by intravenous administration of a certain drug using a dropper.
All operations to remove a tumor are performed by cutting into the abdominal cavity, but there are cases when such operations are performed through the anus.
Forecast
In order to talk about the prognosis, it is necessary to take into account the results of diagnostic studies: size, growth rate, presence of metastasis, depth of damage to the intestinal wall. An important aspect is the age of the patient and the success of the surgery.
If the disease is detected at stage 0, the prognosis for recovery is more than 95%, with the first stage – just over 90%.
When stage 2 is diagnosed, survival rate over 5 years is 72%; at stage 3, the figure drops to 44%. If we consider the thermal stage, then no more than 8% of patients manage to survive 5 years.