Palpation using the Obraztsov-Strazhesko method allows you to determine:
- increase in liver size;
- sensitivity, soreness of the lower edge of the liver;
- surface of the liver (smooth, uneven, lumpy, with nodes);
— liver consistency (soft, dense, rocky);
- edge of the liver (smooth, uneven, pointed, rounded, soft, dense, painful)
EXHALATION
Normally, the liver is not palpable or the edge of the liver is palpable, painless, and has a soft consistency.
With hepatitis, the liver is enlarged, painful, and has a denser consistency.
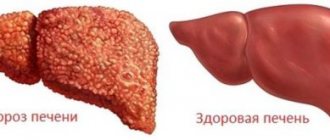
In cirrhosis , the liver is dense, usually painless, the edge is sharp, the surface is smooth or finely lumpy.
In case of congestive heart failure in the
INHALE
Method of jerk-like balloting palpation (used for large ascites): light jerk-like blows are applied to the abdominal wall from bottom to top; - the liver feels like a “floating piece of ice”
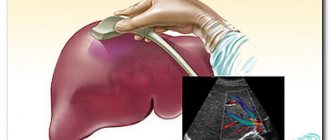
Palpation of the liver is performed as follows. The patient lies on his back with his legs extended and his arms placed along the body, his head lies low. The patient should breathe deeply with an open mouth (relaxation of the anterior abdominal wall is achieved). Palpation is carried out with the right hand. The doctor places the palm and four fingers of the left hand on the right lumbar region, trying to push the posterior abdominal wall forward. With the thumb of the left hand, the doctor presses the lower ribs in front, preventing the expansion of the chest during inhalation. This brings the liver closer to the fingers of the right hand. The palm of the right hand is placed flat with the last four fingers extended and the third slightly bent (the ends of the fingers form a straight line) in the patient’s right hypochondrium at the level of the previously found lower border of the liver along the midclavicular line. As you exhale, the hand sinks behind the costal edge. On a deep inhalation, the lower edge of the liver, pressed downwards by the diaphragm, enters the space between the costal arch and the doctor’s hand and then bends around the doctor’s fingers and slides down under them. At this point, the consistency, nature and tenderness of the lower edge of the liver should be determined.
In case of ascites, severe flatulence, when the liver is pushed upward in a supine position, it is advisable to palpate the lower edge of the liver with the patient in an upright position. The patient should stand slightly leaning forward and breathe deeply. The palpation technique does not change.
A low location of the edge of the liver occurs with:
— omission
liver (hepatoptosis) occurs with visceroptosis, pulmonary emphysema, effusion pleurisy, subdiaphragmatic abscess, while the edge of the liver does not change, but it is not always possible to palpate it, because the liver deviates downward and backward;
— increasing
its size, can affect both the entire liver (blood stagnation, acute hepatitis, obesity, infections, leukemia, amyloidosis) and individual parts (tumors, abscesses, echinococcus).
A decrease in liver size is usually observed with cirrhosis. In this case, palpation is not always possible.
Normally, the liver has a soft consistency. Moderate compaction is observed in acute hepatitis, significant compaction is observed in cirrhosis, neoplasms, and amyloidosis. Blood stagnation, obesity, infections, while causing liver enlargement, do not lead to its compaction.
Character of the edge of the liver:
— normally - sharp or slightly rounded;
- with cirrhosis - sharpens;
- with blood stagnation, non-alcoholic fatty liver disease, amyloidosis - blunt, rounded;
- for cancer - uneven
.
The surface of the liver can be assessed when the liver is compacted. Normally it is smooth. With cirrhosis, it becomes uneven, granular, with focal processes in the liver - lumpy.
Soreness of the edge of the liver appears with perihepatitis, acute cholangitis, blood stagnation against the background of decompensated heart failure, and to a lesser extent with acute hepatitis. With cirrhosis and amyloidosis, the liver is painless.
Liver pulsation occurs when the tricuspid heart valve is insufficient. In this case, the pulsation is felt over the entire surface, in contrast to the transmitting pulsation of the abdominal aorta, when the pulsation is felt along the midline.
Didn't find what you were looking for? Use the search:
Best sayings:
If you get carried away with a girl, tails will grow; if you study, horns will grow
9696 – | 7622 – or read all.
91.146.8.87 © studopedia.ru Not the author of the materials posted. But it provides free use. Is there a copyright violation? Write to us | Feedback.
Disable adBlock! and refresh the page (F5)
very necessary
Just as with other diseases, the diagnosis of liver cirrhosis begins with an initial interview with the sick person, ascertaining his complaints and medical history.
How to determine liver cirrhosis based on medical history
People with this disease may present various complaints: it all depends on the degree of liver damage and the presence of complications.
With compensated cirrhosis, sometimes nothing bothers a person. However, the following symptoms may still occur:
- Episodic mild pain in the area of the right hypochondrium, dull in nature.
- Slight weight loss.
- Deterioration of general condition, weakness.
- There are symptoms of dyspepsia, but they are not very pronounced (mild nausea).
- Sometimes - a rise in body temperature to 37-37.5 ⁰C.
With cirrhosis at the subcompensation stage, complaints become more pronounced:
- Noticeable decrease in performance, fatigue.
- Poor appetite.
- Long periods of dull pain in the right side of the abdomen.
- Severe dyspeptic symptoms: nausea, increased gas formation, vomiting, bowel disorders in the form of constipation or diarrhea.
- Itchy skin for no other apparent reason.
- Sometimes a sick person may notice yellowness of the skin and sclera.
- Increase in body temperature to subfebrile values (37.5 ⁰C).
PALPATION OF THE LIVER
Palpation using the Obraztsov-Strazhesko method allows you to determine:
- increase in liver size;
- sensitivity, soreness of the lower edge of the liver;
- surface of the liver (smooth, uneven, lumpy, with nodes);
— liver consistency (soft, dense, rocky);
- edge of the liver (smooth, uneven, pointed, rounded, soft, dense, painful)
EXHALATION
Normally, the liver is not palpable or the edge of the liver is palpable, painless, and has a soft consistency.
With hepatitis, the liver is enlarged, painful, and has a denser consistency.
In cirrhosis , the liver is dense, usually painless, the edge is sharp, the surface is smooth or finely lumpy.
In case of congestive heart failure in the
INHALE
Method of jerk-like balloting palpation (used for large ascites): light jerk-like blows are applied to the abdominal wall from bottom to top; - the liver feels like a “floating piece of ice”
Palpation of the liver is performed as follows. The patient lies on his back with his legs extended and his arms placed along the body, his head lies low. The patient should breathe deeply with an open mouth (relaxation of the anterior abdominal wall is achieved). Palpation is carried out with the right hand. The doctor places the palm and four fingers of the left hand on the right lumbar region, trying to push the posterior abdominal wall forward. With the thumb of the left hand, the doctor presses the lower ribs in front, preventing the expansion of the chest during inhalation. This brings the liver closer to the fingers of the right hand. The palm of the right hand is placed flat with the last four fingers extended and the third slightly bent (the ends of the fingers form a straight line) in the patient’s right hypochondrium at the level of the previously found lower border of the liver along the midclavicular line. As you exhale, the hand sinks behind the costal edge. On a deep inhalation, the lower edge of the liver, pressed downwards by the diaphragm, enters the space between the costal arch and the doctor’s hand and then bends around the doctor’s fingers and slides down under them. At this point, the consistency, nature and tenderness of the lower edge of the liver should be determined.
In case of ascites, severe flatulence, when the liver is pushed upward in a supine position, it is advisable to palpate the lower edge of the liver with the patient in an upright position. The patient should stand slightly leaning forward and breathe deeply. The palpation technique does not change.
A low location of the edge of the liver occurs with:
— omission
liver (hepatoptosis) occurs with visceroptosis, pulmonary emphysema, effusion pleurisy, subdiaphragmatic abscess, while the edge of the liver does not change, but it is not always possible to palpate it, because the liver deviates downward and backward;
— increasing
its size, can affect both the entire liver (blood stagnation, acute hepatitis, obesity, infections, leukemia, amyloidosis) and individual parts (tumors, abscesses, echinococcus).
A decrease in liver size is usually observed with cirrhosis. In this case, palpation is not always possible.
Normally, the liver has a soft consistency. Moderate compaction is observed in acute hepatitis, significant compaction is observed in cirrhosis, neoplasms, and amyloidosis. Blood stagnation, obesity, infections, while causing liver enlargement, do not lead to its compaction.
Character of the edge of the liver:
— normally - sharp or slightly rounded;
- with cirrhosis - sharpens;
- with blood stagnation, non-alcoholic fatty liver disease, amyloidosis - blunt, rounded;
- for cancer - uneven
.
The surface of the liver can be assessed when the liver is compacted. Normally it is smooth. With cirrhosis, it becomes uneven, granular, with focal processes in the liver - lumpy.
Soreness of the edge of the liver appears with perihepatitis, acute cholangitis, blood stagnation against the background of decompensated heart failure, and to a lesser extent with acute hepatitis. With cirrhosis and amyloidosis, the liver is painless.
Liver pulsation occurs when the tricuspid heart valve is insufficient. In this case, the pulsation is felt over the entire surface, in contrast to the transmitting pulsation of the abdominal aorta, when the pulsation is felt along the midline.
How to diagnose liver cirrhosis during a general examination
The second stage of diagnosis is examination of the sick person. The data obtained will also differ depending on the extent of the process and the presence of complications. At the initial stages, all these signs are weakly expressed or absent, at later stages they appear in full. So , how to determine liver cirrhosis by appearance? You need to pay attention to the following symptoms:
- Jaundice: the skin, mucous membranes, and sclera become yellow.
- Weight loss, little fat tissue, muscles atrophy.
- Spider veins.
- Pronounced capillaries on the face.
- In men - enlargement of the mammary glands.
- Dilated veins on the skin of the abdomen.
- Increase in abdominal volume.
- Edema of the lower extremities.
- Hernias are umbilical, inguinal, femoral.
- Red skin on the palms, less often the soles.
- “Lacquered tongue” - the tongue is bright red and shiny.
- Fingers in the form of “drum sticks” - with widening of the terminal phalanges.
- Hemorrhagic (spotty, red) rash.
In this case, during an extended study, the doctor may reveal:
- Enlarged liver, spleen.
- Decreased muscle volume and tone.
- Changes in the boundaries of the liver and spleen during percussion.
- Dull sound when percussing (tapping) the abdomen.
- Increased body temperature.
- Increased blood pressure and heart rate.
Palpation of the liver during cirrhosis reveals a lot of important information and allows one to suspect the disease. In the initial stages, the liver may be only slightly enlarged, but its consistency remains unchanged. During the stage of decompensation, the enlargement of the liver is significant; it is localized behind the edge of the costal arch, protruding more than 2 cm. During palpation of the liver in cirrhosis, pain is determined, the liver is compacted, its surface is lumpy and uneven.
Laboratory tests in the diagnosis of liver cirrhosis
Let's consider the main laboratory changes that characterize cirrhosis. Sometimes they are not present in full, their severity depends on the degree of activity of the pathology and the functional capacity of the liver.
A general blood test determines anemia, accelerated ESR, and increased white blood cell counts.
A general urine test sometimes reveals protein and red blood cells.
The most revealing is a biochemical blood test. With its help, you can find confirmation of the diagnosis and establish the degree of compensation. The content of all fractions of bilirubin, enzymes increases: AlT (alanine aminotransferase), AST (aspartate aminotransferase), GGT (gamma-glutamyl transpeptidase), a decrease in albumin, an increase in fibrin and changes in other indicators.
Detection of serological signs of viral hepatitis (blood serum examination).
General blood analysis
In a general blood test, the number of platelets decreases. The reason for this will be a decrease in protein synthesis, hypersplenism, or an increase in the size of the spleen due to portal hypertension and increased platelet breakdown. They will also be consumed in excess due to disseminated intravascular coagulation and hemorrhagic syndrome.
The hemoglobin level decreases significantly and the color index drops. After all, hemoglobin is a protein, and there is nowhere to take it from; the protein synthetic function of the liver gradually decreases. For the same reason, the number of red blood cells decreases, and anemia syndrome occurs. In the terminal stages, a patient with cirrhosis experiences bleeding, and if there is hypersplenism, or an enlarged spleen, then red blood cells are further destroyed when passing through it.
Since immune inflammation occurs in cirrhosis, relative leukocytosis is observed for quite a long time, but in the terminal stages there is nothing to build from either, the red bone marrow has a persistent “supply deficiency” and leukopenia occurs in the blood. These echoes of immune inflammation and the release of a variety of substances into the blood from destroyed liver cells cause a long-term and significant increase in ESR, which can last for years.
Thus, liver cirrhosis is one of the most difficult and complex diseases in terms of laboratory diagnostics. The picture is divided into several laboratory syndromes, which can, however, themselves occur in other liver diseases. But the final diagnosis of cirrhosis is currently impossible without instrumental diagnostic methods and liver biopsy.
How to diagnose liver cirrhosis using additional tests?
- Ultrasound for liver cirrhosis often makes it possible to make a final diagnosis, especially during the period of decompensation. With a mild degree of cirrhosis, an ultrasound will show an enlarged liver, but its structure will still be homogeneous. With subcompensation and decompensation, the picture is more typical. If cirrhosis is small-nodular, then an increase in the echogenicity of the liver of a uniform nature is recorded. In case of large-nodular cirrhosis of the liver, ultrasound will reveal individual nodes, a heterogeneous structure of the organ, and often a tuberous surface. In advanced cases, unevenness of the liver lobes is determined: the right one decreases. In the last stages, the liver is even smaller than normal. In addition, ultrasound for cirrhosis of the liver indicates an enlarged spleen.
- Laparoscopic diagnosis is a minimally invasive surgical intervention to confirm the diagnosis. The doctor sees the surface of the liver and can evaluate the picture visually, which helps in the differential diagnosis of liver cirrhosis. If cirrhosis is large-nodular, individual red to brown nodes are visible (usually more than 3 mm), these nodes are irregular in shape or round, with pale connective tissue strands between them. In micronodular cirrhosis, the liver is of a normal shape, with many small nodules on the surface. Connective tissue grows between the nodules. The liver capsule is thickened, the veins are dilated (this applies to all types of cirrhosis).
- Liver biopsy and histological examination of the material allows a final diagnosis to be made. Signs indicating cirrhosis:
- Nodes surrounded by connective tissue
- Hepatocytes of different sizes, unevenly changed vascular lumens
- With active cirrhosis: necrosis of the liver tissue, swelling of liver cells, the border between fibrosis and normal tissue is not pronounced
- With inactive cirrhosis: no necrosis, the above-described border is clear
- Fibrogastroduodenoscopy allows you to determine the presence of dilated veins of the esophagus and diagnose esophageal and gastric bleeding.
How to check your liver for cirrhosis yourself?
Of course, you cannot completely exclude cirrhosis yourself; only a doctor can do this. But there are some signs that a person can notice himself, and then contact a specialist for a full diagnosis.
- Prolonged increase in body temperature for no reason.
- Weight loss, loss of appetite, performance.
- Pain in the right hypochondrium and the right side of the abdomen in general, the pain is long-lasting and dull in nature.
- The appearance of a yellow color of the skin and eyes.
- Nausea, changes in stool, vomiting for which there is no other reason.
- Increased bleeding.
It is especially necessary to monitor your condition for those who have diseases leading to cirrhosis of the liver: hepatitis B, C, non-viral hepatitis, chronic diseases of the liver and gallbladder, alcohol abuse. If you feel worse, you should contact your doctor, who will know how to check your liver for cirrhosis and will prescribe additional tests.
We have put a lot of effort into making sure you can read this article and would welcome your feedback in the form of a rating. The author will be pleased to see that you were interested in this material. Thank you!
Often people who feel pain in the right hypochondrium ask how to identify cirrhosis of the liver at the initial stage. But unfortunately, the disease initially occurs with almost no symptoms, and signs appear when the gland has already increased in size.
To protect the liver from chronic disease, you need to eat right, lead an active lifestyle and undergo preventive medical examinations that will help to detect liver dysfunction.
Liver cirrhosis (transformation of parenchymal tissue into pathological connective tissue) is a common disease that is the final stage of a number of chronic liver diseases. A diagnosis of liver cirrhosis is made, taking into account data from the medical history, physical examination, functional tests, laboratory and instrumental studies.
What indicates liver cirrhosis
Liver cirrhosis is often preceded by viral hepatitis B and C, and the disease also develops against the background of alcohol abuse. The pathology can also develop against the background of chronic autoimmune hepatitis, sclerosing cholangitis, bile stasis, narrowing of the ducts, cystic fibrosis, glycogenosis, galactosemia, Wilson's disease, chronic heart failure, taking hepatotoxic medications, intestinal surgery, parasitic infestation of the intestines and liver.
Therefore, when diagnosing liver cirrhosis, studying the patient’s medical history is of great importance. Symptoms of cirrhosis depend on the etiology of the disease, the rate of progression and the degree of organ damage. About 20% of patients at the early stage of the process do not notice any signs of the disease, while others only mention increased gas formation and decreased performance.
As the tissue degenerates, a temporary dull pain occurs in the right side, which occurs after drinking alcohol or heavy food, and does not go away after taking antispasmodics. Signs of bile stagnation are rapid saturation and itching of the skin.
In some cases, nosebleeds occur and fever begins. As the disease progresses, jaundice and signs of portal hypertension, varicose bleeding from hemorrhoidal and esophageal veins are detected, and the amount of fluid in the abdominal cavity increases (ascites).
The following symptoms are typical for patients with cirrhosis:
- “drumsticks” (the phalanges of the fingers are thickened);
- “watch glasses” (changes in the nail plate);
- palmar erythema (red palms);
- “Spider veins” (thin vessels are visible through the skin of the face and body).
Thus, the doctor can assume cirrhosis of the liver during the first examination of the patient, after studying his medical history. In the later stages of cirrhosis, even the appearance of the patient changes, which can serve as an indirect sign of the development of pathology.
After interviewing the patient about his medical history, complaints and lifestyle, the doctor conducts a physical examination, which includes palpation and percussion of the abdominal cavity, and examination of the skin. Upon examination, the doctor notes yellowing of the skin and sclera, weight loss, capillaries on the body and face, dilated veins in the abdomen, enlarged abdomen, swelling of the legs, redness of the palms, and a red rash.
The severity of these signs depends on the degree of the disease and at an early stage they may be completely absent. When palpating and listening to the abdominal cavity, the doctor may notice:
- hepatosplenomegaly;
- decreased tone of the abdominal wall muscles;
- changes in the contour of the liver and spleen during percussion;
- dull sound when tapped.
When palpating the liver, the doctor receives a lot of information, since enlargement of the gland is typical even for the initial stages of the pathology. In the stage of decompensation, the organ is already significantly enlarged and protrudes beyond the edge of the costal arch by two centimeters. The doctor determines by touch that the gland is too dense and uneven due to the formation of nodules.
What do tests show?
Blood tests for liver cirrhosis show a lack of hemoglobin, leukocytopenia and thrombocytopenia, which indicates a pathological enlargement of the gland. The coagulogram notes a decrease in the prothrombin index, that is, the blood clots more slowly than normal.
Blood biochemistry reveals increased activity of liver enzymes (alkaline phosphatase, Alt, AST), increased total and direct bilirubin, potassium, sodium, as well as urea and creatinine, and decreased albumin. Additionally, in case of liver cirrhosis, tests are carried out for antibodies to viral hepatitis, and the content of alpha-fetoprotein is determined.
Biochemical blood test
When conducting a biochemical study, you should know that a biochemical blood test for liver cirrhosis indicates different laboratory syndromes:
- Cytolysis syndrome. The integrity of liver cells is disrupted, their contents are released into the blood.
This syndrome can be diagnosed in the initial and middle stages of cirrhosis, when there are still many liver cells. In this case, transaminases ALT and AST, isoenzymes of lactate dehydrogenase increase, and hyperbilirubinemia occurs (the direct fraction increases). You can also find increased levels of vitamin B12 and iron in the blood.
The enzymes ALT and AST, which are markers of cytolysis and greatly increase in acute viral hepatitis, in cirrhosis reflect the gradual disintegration and disappearance of the liver tissue. Therefore, usually in patients with cirrhosis, transaminase levels are, of course, significantly higher than normal, but usually do not reach 200 units. And only in the terminal stage, when there is nothing left of the liver cells, these biochemical indicators drop sharply;
- Laboratory syndrome of cholestasis, when the bile ducts are affected and destroyed.
An excess of alkaline phosphatase, gamma-glutamyl transpeptidase, leucine aminopeptidase, high levels of cholesterol and phospholipids appear in the blood, along with high bilirubin there is an increase in the concentration of bile acids and beta-lipoproteins. Cholestasis is characterized by an increase in direct bilirubin and an increase in the concentration of bile acids;
- Hepatocellular failure.
The liver begins to slow down the synthesis of various substances. In the blood serum, the concentration of total protein decreases due to the albumin fraction, low levels of prothrombin and cholesterol are found (as you remember, in the case of isolated cholestasis it increases - there it simply enters the blood, and this result indicates a decrease in its synthesis). The activity of the cholinesterase enzyme decreases, the concentration of ammonia, aromatic compounds - phenols and free amino acids, which the liver is no longer able to convert into proteins, gradually increases.
In the case of a stable course of liver cirrhosis without the addition of symptoms of hepatic encephalopathy, the level of ammonia in the blood serum increases slightly, no more than 50% of the upper limit of normal. If ammonia increases by one and a half to two times, then this will be characteristic of encephalopathy, which indicates the approach of hepatic coma;
- Blood clotting disorder syndrome - laboratory hemorrhagic syndrome.
With cirrhosis of the liver, the ability to synthesize protein is sharply reduced, so there is nothing to produce blood clotting factors from. When performing a hemostasiogram, the number of factors 7, 2,9 will decrease. Deeply advanced cirrhosis and hepatic cell failure leads to a decrease in the synthesis of factors 1, 5 and 13. In addition, massive and steady destruction of liver cells releases many thromboplastic substances into the blood.
Intravascular coagulation occurs in the blood, followed by fibrinolysis. As a result, all these coagulation factors are consumed, and according to the coagulogram, this condition in cirrhosis is called consumption coagulopathy;
- Finally, we can also distinguish the so-called laboratory syndrome of immune inflammation.
In the initial stages of cirrhosis, an immune reaction occurs, during which the concentration of gamma globulins in the serum increases, and this is especially characteristic against the background of a decrease in albumin levels. The indicators of thymol and sublimate tests change significantly, and in immunoassays the ratio of lymphocyte subpopulations changes.
The biochemistry of blood in cirrhosis is far from exhausted by these numerous data. If we remember that hormone metabolism is disrupted, we can give an example of such participation of aldosterone. The patient develops a state of increased potassium and hydrogen consumption due to hyperaldosteronism. Where does it come from?
In a normal patient, aldosterone, which has served its term, is destroyed in hepatocytes. With cirrhosis, hepatocytes become fewer and fewer and aldosterone accumulates. As a result, the water-salt balance is disrupted, since aldosterone continues to work “over the top”, and the content of potassium and magnesium in the blood decreases. In patients with advanced cirrhosis, the amount of sodium is further reduced and, although it is retained in the body, it can pass into the intercellular and ascitic fluid with the formation of congestive edema, despite the general exhaustion and weight loss of the patient.
Hardware research for diagnostics
It is impossible to diagnose cirrhosis only on the basis of the patient’s complaints, his medical history and laboratory blood tests, since the same data can be obtained for completely different pathologies of the biliary system, and the characteristic signs of cirrhosis develop with significant liver damage.
Differential diagnosis is carried out between liver cirrhosis and cancer. Verification and confirmation of diagnoses is carried out using ultrasound, laparoscopy and biopsy. If cirrhosis led to liver cancer, then pathologies can only be distinguished by laparoscopy.
Also, the symptoms of cirrhosis are similar to the parasitic disease echinococcosis, in which the gland enlarges and becomes denser. In this case, ultrasound is informative, and the diagnosis is confirmed by laboratory testing that detects antibodies to esinococcus.
During differential diagnosis, it is possible not only to make the only correct diagnosis, but also to determine the type of cirrhosis. During the research, the biliary system is thoroughly studied, which makes it possible to determine the cause of the development of the pathology and take measures to eliminate it.
Diagnosis of liver cirrhosis includes an ultrasound examination of the gland. An ultrasound accurately determines the size of the organ and its shape, notes sound permeability, and looks for signs of portal hypertension and changes in the spleen. This study provides a low-resolution image, but it still allows one to recognize inflammatory processes and neoplasms in the gland.
At the initial stage of cirrhosis, the structure of the liver is still homogeneous, and at the stage of subcompensation and decompensation, fibrous tissue is already noticeable, replacing parenchymal tissue. With small-nodular cirrhosis, the echogenicity of the gland is increased evenly, and with large-nodular cirrhosis, individual nodes and a heterogeneous tissue structure are distinguished.
In the later stages of the disease, the right lobe of the liver is reduced, and in the latter the gland becomes smaller than normal. Thus, an ultrasound examination of the liver allows not only to make a diagnosis, but also to determine the stage of development of cirrhosis.
Tomography
Computed tomography of the abdominal cavity makes it possible to see the gland, its vessels and bile ducts in more detail. If necessary, an MRI of the liver is performed. Based on the study, a conclusion is made about the homogeneity and density of the gland tissue.
Using this method, you can examine the vessels and bile ducts and draw conclusions about their patency. Due to its high cost, the examination is carried out to clarify the results of other diagnostic studies.
The images show congenital anomalies of the hepatobiliary system, metastases of extrahepatic tumors, accumulation of iron in hepatocytes, and obstruction of the bile ducts. This information is useful in making a diagnosis and determining further treatment tactics, and can also shed light on the etiology of the disease.
Doppler
Doppler analysis of the vessels of the gland determines the course of the vessels, whether there are obstacles to blood flow, and also measures the diameter of the vessels and the speed of blood flow. It is determined whether there is a change in blood flow speed when holding your breath or straining.
Laparoscopy
Laparoscopic examination is an operation that is performed to confirm the diagnosis. The doctor visually evaluates the surface of the gland. In large-nodular cirrhosis, individual nodes larger than 3 mm are distinguishable, between which there are strands of fibrous tissue. With small nodules, there are small nodules on the liver, the space between which is filled with connective tissue.
Other methods for diagnosing cirrhosis
Although laboratory methods occupy an important place in making the diagnosis of liver cirrhosis, in addition to them there are other equally informative studies.
- Collection of complaints, medical history and physical data are routine methods necessary to suggest liver pathology.
- Testing for the presence of antimitochondrial antibodies, a serological diagnostic method, is necessary to determine the cause of primary biliary cirrhosis.
- Ultrasound examination of the liver, gallbladder and biliary tract is the most easily accessible and frequently used method. With its help, you can evaluate the size, structure, blood supply of the organ, as well as the patency of the bile ducts and the condition of the bladder.
- Cholecystography is an auxiliary x-ray method for examining the gallbladder and bile ducts.
- CT scan.
- Magnetic resonance imaging.
- Puncture biopsy is the main histological method, with the help of which, more recently, it has been possible to differentiate cirrhosis from chronic hepatitis. A piece of organ parenchyma is taken and examined under a microscope.