The liver, due to its anatomical features, is often affected by bacterial or parasitic diseases of the abdominal cavity. This is the only formation in the body that has a double blood supply - vessels from the portal vein system (portal) and the hepatic artery approach it. This allows the infection to move to the liver from other organs: appendix, colon, stomach, pancreas, and so on. Also, structural disturbances can occur due to congenital defects, exposure to toxic substances (alcohol, heavy metals, metabolic disorders (Wilson-Konovalov disease) or specific viruses (hepatitis A, B, C, and so on).
In order to promptly detect signs of these diseases, a screening method is needed that will allow us to study the structure of the liver in sufficient detail. In accordance with MES (medical standards of care), ultrasound is the optimal method of primary diagnosis. It is accessible, safe and does not require much time to carry out.
Indications
An ultrasound of the liver is required during the examination of the abdominal organs. In addition, Professor Zubarev’s clinical recommendations highlight indications when it is necessary to study the structure of this organ using ultrasound:
- any suspicion of tumors (adenomas or cancer) of the liver;
- the presence of symptoms or laboratory data (increased ALT and AST) that indicate damage to this organ;
- determination of an increase in the size of the liver by palpation;
- control over minimally invasive interventions (liver puncture with biopsy, percutaneous drainage of an abscess, and so on);
- the need to monitor the dynamics of liver disease (for example, confirmation of the elimination of an abscess, disappearance of portal hypertension).
Currently, ultrasound in the adult working population is performed for the purpose of preventive examinations.
How is the procedure performed?
The child is located on the couch lying on his back. During the examination, the doctor may ask him to turn over on his side or hold his breath. A special gel is applied to the skin of the abdomen, which helps improve image quality.
Then, using an ultrasound probe, the doctor examines the liver from different angles. Rays passing through the body are reflected from the organ and structures. The signal is captured and processed by sensitive equipment. The graphic image is transmitted to the monitor.
The duration of the study is 10–25 minutes. After the procedure is completed, the doctor fills out an examination protocol, which is transcribed by the attending physician.
Preparation for liver ultrasound
For the best quality of research, it is necessary to eliminate all obstacles to the passage of the ultrasound wave through the body. The most common hindrance is intestinal gases, which are formed as a result of metabolic processes of normal microflora. Considering this fact, preparation for liver ultrasound is carried out as follows:
| Time interval | Recommendations for the patient |
| 2 days before the procedure | Following a diet low in fiber (excluding plant foods, rye bread, milk, juices) |
| 8 hours before the procedure | Avoid eating. For adults, smoking and drinking alcohol are also contraindicated. |
If the patient followed all the recommendations, the ultrasound results will be as reliable as possible. To correctly decipher the indicators, you should consult a qualified doctor, since a large number of nuances and normal variations in liver size can lead the patient to incorrect conclusions.
Technique for ultrasound examination of the liver
The liver
is the largest human organ, weighing about 1500 g and located in the right upper quadrant of the abdomen. The use of real-time ultrasound scanning has greatly facilitated abdominal ultrasonography in liver studies. This is facilitated by the high resolution and accessibility of the method, which increase diagnostic capabilities when assessing various liver lesions. The liver is considered the easiest organ for ultrasound examination, and the use of echography provides a lot for diagnosing its diseases.
Preparing the patient.
Ideally, the patient should fast for 6 hours before the procedure to reduce bloating and fill the gallbladder. Although scanning the liver is not difficult, we recommend, especially for beginners, to follow a fixed algorithm to ensure that all liver parenchyma is examined and all examination objectives are completed.
Research technique.
The patient's position can be either on the back or on the right side. The technical sequence of actions is as follows.
Subcostal section of the liver
We place the sensor under the right lower costal edge (Fig. 3) and, lightly pressing on the skin, make fan-shaped movements from top to bottom and from outside to inside (Fig. 4). When we point the sensor upward, we see the hepatic veins (Fig. 5) and study the segmental structure of the liver. Then, by pointing the probe slightly downward, you can see the veins of the portal system (Fig. 6).
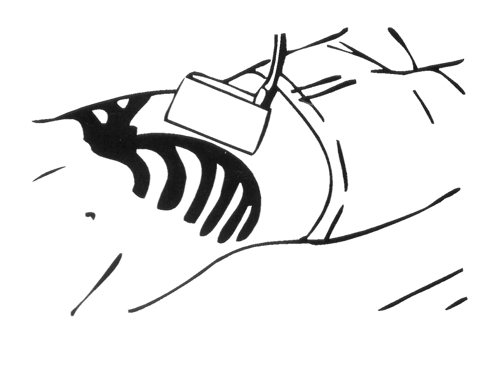
Rice. 3.
Scheme of applying a sensor to obtain a subcostal section of the liver.
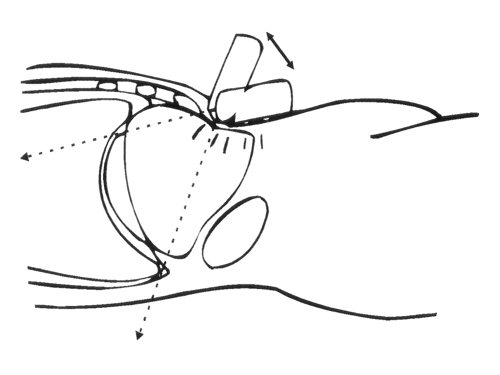
Rice. 4.
Scheme of the fan-shaped movement of the sensor during ultrasound of the liver.
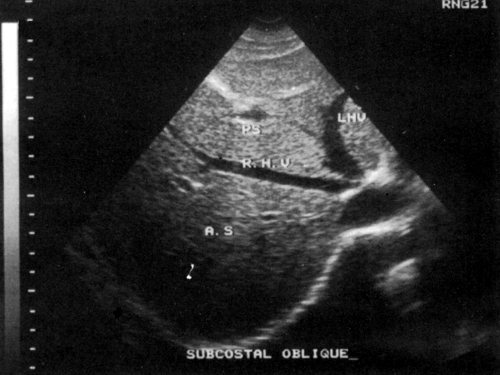
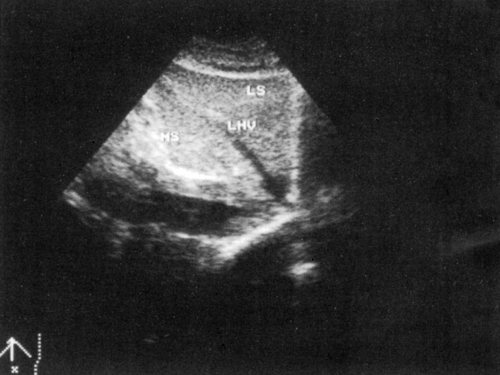
Rice. 5.
Ultrasound of the hepatic veins.
a)
Level of location of the hepatic veins (diagram).
b)
Normal image of the hepatic veins (echogram).

Rice. 6.
Bifurcation level.
a)
The bifurcation level is achieved when the sensor is directed slightly caudally (diagram).
b)
Normal image of the portal veins at the level of the bifurcation (echogram).
Longitudinal section of the liver
We firmly install the sensor on the skin under the xiphoid process and direct it upward (Fig. 7), then move it in the lateral direction (parallel to the original position) so as to examine the entire liver (Fig. 8). This section is ideal for examining the left lobe of the liver.

Rice. 7.
Longitudinal liver scan - sensor application diagram. The sensor should be in close contact with the skin.

Rice. 8.
Echograms of a longitudinal section of the liver.
a)
Longitudinal section of the liver through the right lobe.
b)
Longitudinal section of the liver through the left lobe.
Cross section of the liver
A transverse section of the liver can be obtained by rotating the probe 90° from the longitudinal position and passing it through the liver (Fig. 9). These sections are of great help in assessing the dilatation of the intrahepatic bile ducts, which is clearly visible on transverse sections of the right lobe.
Rice. 9.
Obtaining a cross section of the liver.
a)
Scheme of applying the sensor to obtain a cross section of the liver.
b)
Cross section of a healthy liver (echogram).
We complete the abdominal ultrasonography of the liver by installing the sensor in the 7-10 intercostal space to examine the vault of the right lobe of the liver, which sometimes cannot be clearly visualized, especially in obese patients. In addition, the intercostal approach can help in examining the vessels and gallbladder.
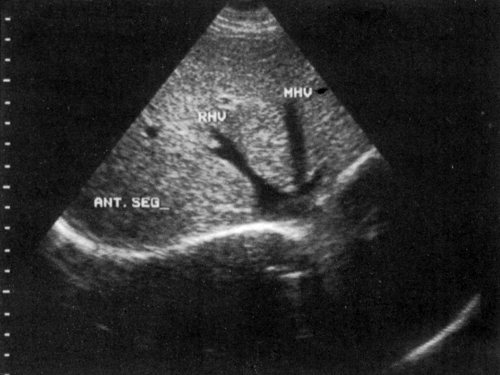
Segmental structure of the liver
The segmental structure of the liver is an important part of ultrasound examination, since information about which segment of the organ the lesion is located in is of great importance. The liver can be divided by the hepatic veins as follows: the right vein divides the right lobe into two segments - posterior and anterior (Fig. 10) and the left vein divides the left lobe into lateral and medial segments (Fig. 11). Now, if we draw longitudinal planes through the left, middle and right main portal veins (Fig. 12), the liver will be divided into eight segments (Fig. 13).
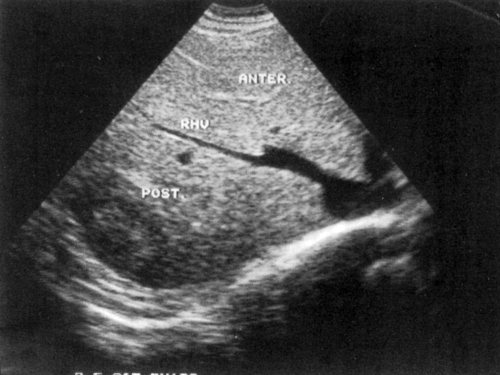
Rice. 10.
A subcostal oblique section through the right lobe of the liver allows you to see the anterior and posterior segments (echogram).
Rice. eleven.
Medial and lateral segments of the left lobe of the liver (echogram).
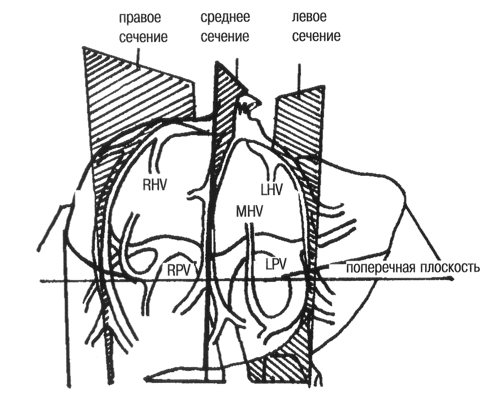
Rice. 12.
Longitudinal planes drawn through the left, middle and right branches of the portal vein. RHV - right hepatic vein, MHV - middle hepatic vein, LHV - left hepatic vein, RPV - right main portal vein, LPV - left main portal vein.
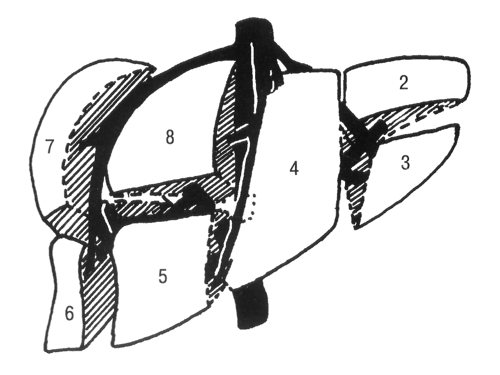
Rice. 13.
The liver is divided into eight segments as follows: 1 - caudate lobe, which is bounded posteriorly by the inferior vena cava and anteriorly by the main hepatic groove; 2 and 3 — left lateral segment; 4 - left medial segment; 5 and 8 — right anterior segment; 6 and 7 - right posterior segment.
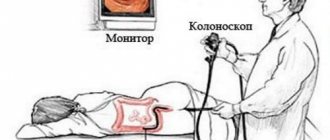
Causes of flatulence
There are many factors that can cause such an unpleasant condition:

eating foods that cause increased fermentation or gas formation;- consumption of a certain type of food with chronic intolerance;
- lack of colon enzymes (which is common in newborns);
- disturbance of intestinal microflora;
- slowing of intestinal motility (during intoxication and infections);
- mechanical obstacles in the intestine that interfere with the movement of food mass (tumors or adhesions);
- excess progesterone in the blood, which relaxes muscles (during pregnancy);
- disruption of adequate blood flow in the vessels of the pelvis and lower extremities;
- stress that causes involuntary intestinal spasms.
Drug treatment
The basic principles of prescribed therapy primarily depend on the cause that caused the excessive discharge of intestinal gases. In addition, medications are prescribed to normalize the composition of the intestinal microflora and prevent increased gas formation:

prebiotics that stimulate the growth of beneficial bacteria;- probiotics, which populate the intestines with essential bacteria;
- drugs to destroy gas bubbles in the colon;
- enterosorbents that remove microbes and gases;
- agents that enhance intestinal motility;
- enzymes;
- antispasmodics;
- antiparasitic agents.
It should be noted that it is quite difficult to independently determine the cause of flatulence, so it is highly undesirable to take any medications without a doctor’s recommendation.
Traditional methods
Traditional medicine offers many recipes to reduce gas formation:
- Carrot seeds are taken one dessert spoon three times a day.
- One spoon of dill seeds is poured into a liter of water and infused in a water bath for twenty minutes. Then the broth needs to stand for at least three more hours. The tincture is taken one third of a glass three times a day.
- A dessert spoon of bitter wormwood is poured with a glass of boiling water and left for 12 hours. Take one spoonful of tincture at least three times a day.
Diet

It is recommended to limit sweets and baked goods as much as possible. Eating legumes also causes problems with digestion. Each piece should be chewed thoroughly, without being distracted by conversations.
You should drink at least two liters of clean water per day (coffee and tea will only increase gas formation). It is advisable to completely eliminate alcohol and carbonated drinks from the daily diet.
What diseases can flatulence indicate?

Flatulence is usually called the excessive release of gases formed in the intestines as a result of the vital activity of microorganisms inhabiting it. The condition may also be accompanied by painful bloating, belching, and bad breath.
Flatulence can be either one of the signs of diseases of the digestive tract, or a consequence of unbalanced or excess nutrition.