Comparison of MRI of the intestine and colonoscopy
The advent of magnetic resonance analysis in medical diagnostics has significantly improved the quality and level of diagnosis of many pathologies and increased the number of detected pathologies several times. With the help of an MRI machine, such complex conditions as tumors of the brain, spine, and bones of various locations began to be accurately diagnosed. The diagnostic method makes it possible to assess the size, location of the formation, its relationship and relative position in relation to neighboring organs and tissues.
To identify intestinal pathologies, the magnetic resonance analysis method is not used so often. Most appointments are for diagnosing neoplasms. This is explained by the peculiarity of the target organ. The intestinal loops are located tightly to each other and can be layered on top of one another, which reduces their visualization for magnetic waves. It is more suitable for examining pathologies of the small intestine, since it is not possible to reach it during a colonoscopic examination.
Colonoscopy involves an invasive examination. This means that the mucosal imaging device is inserted directly into the intestine through the anus. On the monitor screen, the doctor sees exactly what the surface of the intestinal mucosa looks like and can assess the presence or absence of pathological formations. Using video colonoscopy, you can not only examine the intestines from the inside, but also take material for biopsy examination.
Indications and contraindications
It’s unlikely that anyone would even think of going through a colonoscopy procedure just like that. It is prescribed only by a doctor if the patient has indications for it. When seeking advice, there is usually a standard set of complaints:
- pathological discharge from the anus;
- painful act of defecation;
- stool disorder;
- constipation;
- flatulence;
- weight loss;
- manifestations of anemia: pallor of the skin;
- diagnosing a history of intestinal neoplasms.
Such subjective complaints can be made by patients in whom the doctor suspects intestinal tumors of various locations, intussusception of an intestinal loop, Crohn's disease, colitis of various origins and clinical manifestations.
It is important to consider when choosing which is better: MRI or colonoscopy of the intestine, the subjective state of the patient, a list of concomitant diseases and an anamnesis of the previous medical history.
Contraindications to colonoscopy examination are as follows:
- diseases of the cardiovascular system;
- mental disorders;
- pregnancy with gestosis;
- intestinal damage;
- tendency to bleed;
- post-infarction state;
- pelvic joint injuries.
If possible, it is better to conduct a magnetic resonance examination in such cases. The diagnostic method is no less informative, but not always realistic for several reasons:
- lack of a tomograph;
- inability to ensure patient immobility during the procedure;
- pregnancy, especially the first three months;
- presence of a pacemaker;
- metal prostheses;
- claustrophobia - fear of closed spaces;
- deep drug or alcohol poisoning;
- general serious condition of the subject.
It is impossible to say unequivocally whether it is possible to do an MRI of the intestine instead of a colonoscopy. The indications for both procedures are similar, but the result cannot always be obtained from any one of them.
Indications and contraindications
In what cases is an MRI examination prescribed? Indications for magnetic resonance diagnostics are:
- health status indicating the development of an oncological process in the body;
- congenital abnormalities of internal organs;
- signs of bleeding in the gastrointestinal tract;
- symptoms indicating intestinal obstruction.
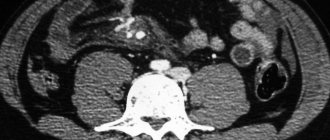
MRI is the main diagnostic method in oncology in cases of tumor location in various parts of the gastrointestinal tract, including those affecting the rectum and sigmoid colon. This method will also reveal the presence of metastases and their exact location. In cases where rectal cancer is diagnosed, the doctor may order an MRI to select the optimal tactics for surgical intervention.
MRI of the gastrointestinal tract will also be informative for other diseases of the small and large intestines; it will detect polyps, benign formations, and the presence of stones. A magnetic resonance imaging scanner also makes it possible, simultaneously with an examination of the intestines, to determine diseases of the kidneys, bladder and other pelvic organs.
This diagnostic technique has its contraindications. Thus, MRI cannot be performed in the following cases:
- the presence of implants containing metal parts in different parts of the patient’s body. This prohibition is due to the occurrence of resonance in response to the magnetic field of the equipment, which will lead to distortion of diagnostic results;
- hypersensitivity to contrast agents administered before the procedure; the patient has renal failure with a decrease in glomerular filtration rates to 30 ml/min/1.73 m2 or lower. For higher numbers, a preliminary consultation with a nephrologist is required;
- children under 7 years old, because Until this age, babies cannot lie in one position for a long time.
Is MRI done in different parts of the intestines and rectum during pregnancy? And when is it safe to carry out such diagnostics?
Here we must take into account that during the first trimester the formation of all internal organs and systems occurs in the fetus. Any external influence during these periods can lead to the appearance of pathology and developmental abnormalities. Therefore, if we consider the duration of pregnancy by week, MRI examination is completely excluded during the first 12 weeks. At later stages, this diagnostic method is not dangerous to the health of the woman herself and her baby.
Preparation and performance of MRI
In order to obtain the maximum diagnostic result and prescribe adequate treatment for the disease, it is necessary to properly prepare for the study. The intestines should be practically free of feces. To do this, a few days before the scheduled examination, you need to start following the following diet:
- pureed or slimy soups with water;
- homogeneous porridges from neutral cereals;
- Drinks allowed include water, herbal tea, and choleretic infusions;
- limit meat and eat only boiled;
- the last meal no more than 10-12 hours before the study.
Alcoholic drinks, smoking, so-called fast food products, pickled dishes, dairy products, confectionery, mushrooms, and nuts are strictly prohibited these days. All of the listed products cause increased gas formation and make it difficult to stool, which is unacceptable for obtaining a good result of magnetic resonance imaging. On the eve of the appointed time, do several cleansing enemas to completely cleanse the intestinal walls of feces.
An MRI takes from 40 minutes to one hour. At this time, the patient must remain motionless inside the chamber; to ensure this condition, he can be additionally fixed with special fasteners. The method is absolutely painless; its negative property for the patient’s subjective perception may be psychological discomfort. The doctor evaluates the data obtained from the images, which remain in digital form.
What are the distinctive features of the methods?
Both studies are prescribed for suspected intestinal tumors, for the diagnosis of polyposis, severe chronic colitis. Sometimes colonoscopy helps to exclude or confirm congenital pathology of the colon such as dolichosigma or dolichocolon (elongation of the intestine, the presence of additional loops of the organ).
The essence of the methods
Colonoscopy is an invasive study, that is, it is inserted into the human cavity - the intestinal tube. The procedure is performed using an endoscope equipped with a camera. The device is inserted through the rectum into the intestine, after which it is slowly advanced up to the cecum. Capsule colonoscopy is considered modern, in which the patient swallows a capsule with a camera and a memory medium. After its release, the flash memory is removed, and the doctor evaluates the images of the mucous membrane and lumen of the entire gastrointestinal tract.
MRI uses a magnetic field to produce layer-by-layer images of the area being examined. It is noteworthy that the technique is quite safe, especially compared to computed tomography, which is based on X-rays. A distinctive feature of MRI from colonoscopy is that to perform it there is no need to penetrate the human cavity and introduce foreign objects into it.

Difference in preparation
The general goal that is pursued in preparing for examinations is to cleanse the intestines for better visualization. For this, in both cases, a special diet is prescribed a few days before the procedure. It involves the exclusion of foods that can cause flatulence (brown bread, fruits, fresh vegetables, legumes, baked goods).
We recommend reading:
Fistulography of the fistula: preparation and examination
For both MRI and colonoscopy, it is necessary to clear the intestines of stool the day before the examination. Doctors prescribe cleansing enemas or medications.
When preparing for intestinal colonoscopy, preference is given to special cleansing preparations such as Fortrans. They are drunk strictly according to the scheme and are used only before endoscopic examinations. Contraindications must be taken into account.
In addition, fibrocolonoscopy is often performed under anesthesia, which requires prior consultation with an anesthesiologist. Before the procedure with anesthesia, you will also have to undergo an ECG and some laboratory tests.
Difference during the study
There are differences between the methods not only in preparation, but also in conducting the examination. If during an MRI the patient is in a separate room and placed in a large tomograph, then a colonoscopy is performed directly by a doctor and a nurse.
| Features of the event | MRI of the intestines | Fibercolonoscopy |
| Patient position | Lying flat on your back. | On the left side. |
| Time spending | 30-50 minutes. | From 30 minutes or more. |
| Need for anesthesia | No. | If indicated, if desired by the patient. |
| The need to administer a contrast agent | Sometimes (especially if a tumor is suspected) | No. |
| Possibility of surgical treatment and biopsy | No. | Yes (if necessary, under anesthesia, the doctor can remove polyps, stop bleeding, and perform a biopsy). |
MRI produces layer-by-layer images of a human organ, which are then carefully examined by a radiologist and makes a conclusion. During a colonoscopy, diagnosis is made “on the spot” - the doctor independently examines the intestines during the examination.
Preparing and performing a colonoscopy
In order for a colonoscopy to give the most informative results, you need to prepare for it in much the same way as for an MRI. The intestines must be completely freed from feces, follow a diet, take laxatives the day before and do several high cleansing enemas.
During the examination, the patient experiences discomfort because the colonoscope tube is inserted directly into the intestine through the anus. During the examination, the patient is on his side, his legs are bent and brought to his stomach. A complete examination lasts approximately 20–30 minutes. The doctor visually assesses the condition of the intestinal mucosa, the presence of tumors, their shape, appearance, location directly during a colonoscopy, since he sees the picture transmitted by the camera on the monitor screen.
Preparatory activities
Any diagnostic method requires complete readiness from the patient.
If you follow all the recommendations, you will not have to go through the procedure again and will be able to make an accurate diagnosis.
If an MRI of the intestine is prescribed, preparation for the study consists of following certain rules:
- 2-3 days before the appointed date, a person should follow a cleansing diet. She completely excludes from the diet those foods that lead to the formation of gases and the development of constipation. This includes sweet and flour products, dairy products, some fruits and vegetables, legumes, and alcoholic beverages.
- If it is not possible to cope with the problem of increased gas formation, the doctor prescribes carminative drugs in the form of Espumisan.
- For chronic constipation, you should do an enema or take a laxative the night before.
- It is forbidden to eat 6 hours before the procedure.
- In some cases, a contrast agent may be required.
Such activities will provide significant assistance in preparing for MRI.
Comparative advantages and disadvantages of methods
How to make a choice: MRI of the intestines or colonoscopy, which is better to do, what are the reviews, all this worries those who are faced with the issue of examining the intestines for the first time.
The indisputable advantages of magnetic resonance diagnostics include:
- digital accuracy of the obtained data;
- the ability to assess the spatial location of detected tumors;
- safety of data in the form of images and computer material;
- non-invasive, painless for the patient.
The method has the following disadvantages: the ability to detect inflammatory changes in the mucosa is very limited, when intestinal loops are superimposed on each other, pathology may not be detected, the price of the procedure is quite high.
The advantages of colonoscopy are the following:
- obtaining visualization of the pathological formation;
- During the procedure, it is possible to take material for histological examination;
- colonoscopy makes it possible to immediately cauterize the ulcer and cut off the polyp;
- objective assessment of the condition of the mucous membrane.
The disadvantages of a visual examination of the large intestine are quite significant: pain, psychological discomfort, the likelihood of injury to the intestinal mucosa, and the potential danger of bleeding.
MRI (magnetic resonance imaging)
The essence of the MRI method: the use of nuclear magnetic resonance properties. Organs are affected by electromagnetic waves. As a result, hydrogen atoms are excited in the cell nuclei. This electromagnetic response is recorded by a special tomograph.
Safety: during this study there is absolutely no radiation exposure to the body. Therefore, MRI can be used as often as the situation requires and even in those patients for whom X-ray irradiation is contraindicated (pregnant women, infants, patients with bone marrow diseases, etc.).
Information content: the doctor can obtain a three-dimensional image of the area being examined. In addition, the slice thickness is 1-5 mm (the ability to detect the smallest pathological foci). Currently, this is the most accurate method for studying the human body. However, due to the structure of the intestine, there are limitations in studying the digestive system. The stomach and esophagus are clearly visualized during MRI, but the numerous loops of intestine that overlap each other are not always visible.
What can be examined: features of the blood supply to the stomach and intestines, lymph nodes, abdominal organs - stomach, loops of the large and small intestines, liver, spleen, retroperitoneal space - kidneys, adrenal glands.
Indications for MRI (if gastrointestinal disease is suspected):
- Constant abdominal pain.
- Suspicion of a tumor process.
- Detection of stomach or intestinal ulcers.
- Suspicion of congenital anomalies.
- Intestinal obstruction (volvulus, stones and other causes).
MRI of the intestine using an open type device

Methodology of the procedure: the study is carried out without any anesthesia, always on an empty intestine. Therefore, before the procedure, the patient requires a cleansing enema. The whole process takes a few minutes and is absolutely painless for humans.
Contraindications:
- The presence of various metal implants;
- Pacemakers;
- Ferromagnetic and electronic devices;
- Any metal parts and fragments.
These are absolute contraindications. In such cases, it is impossible to replace colonoscopy with MTP. Relative contraindications are the presence in the body of implants not made of metal, but of plastic (wires, hemostatic clips, insulin pumps, etc.). In addition, difficulties arise with patients suffering from claustrophobia and mental illness.
Which method is more informative?
It is not possible to give an unambiguous answer to this question. Medicine is not an exact science, so diagnostics must complement each other.
The data obtained from MRI or colonoscopy are equally valuable, it all depends on how much they helped to make the correct diagnosis. The doctor has education, experience, clinical thinking, so the assessment of how much more he needs this or that method is only up to him.
Reviews from doctors and patients
The doctor has a specific task: to make a diagnosis and carry out competent, adequate treatment. In order to achieve this goal, a specialist must understand the details of instrumental diagnostics and prescribe exactly the type of study that will facilitate the path to diagnosis.
Reviews from doctors about the advantages or disadvantages of intestinal MRI and colonoscopy are different in each individual case, it all depends on whether the planned information was received or not enough.
Patients are afraid of the discomfort that a colonoscopy can bring. This is understandable and justified, but you should not categorically refuse it if the doctor insists on conducting a colonoscopy examination.
Who chooses
The choice in this case should be a priority for the attending physician. The patient has the right to control his own health; he may be subject to subjectively unpleasant, invasive diagnostics, but this is not always justified. MRI, despite being painless, is a fairly serious test for the nervous system.
The doctor must choose because he is the one to diagnose and treat the patient. Without complete confidence in the clinical picture and pathogenesis of the disease, it is impossible to prescribe treatment and choose the right tactics. It is necessary to take into account the patient’s subjective attitude, his somatic diseases, and the state of the nervous system, but one should only be guided by the achievement of the result.
MRI of the intestine or colonoscopy?
MRI (magnetic resonance imaging) is one of the most informative and popular diagnostic techniques. MRI is used to study almost all body systems, including the intestinal tract. The impact of an MRI scanner is absolutely harmless and safe for human health, since the equipment technology is based on a strong magnetic field, and X-rays are not used during the procedure. MRI has many advantages over other diagnostic technologies, but as an independent method it does not always provide detailed visualization of the full clinical picture. Often, MR imaging is performed in combination with other techniques, which together complement each other. You need to figure out what is better: MRI of the intestine or colonoscopy?!
Colonoscopy is an endoscopic invasive technique for examining the intestines, which with high accuracy detects inflammation of the mucous membrane, the development of the pathological process and neoplasms of any etiology, even at the stage of initial formation. Endoscopy is prescribed as a standard diagnosis of the intestine, after which, if necessary to confirm the diagnosis, the patient is sent for additional examination (CT or MRI).
If we compare between MRI of the intestine and colonoscopy, in terms of the comfort of the procedures, magnetic resonance imaging takes the lead, since its implementation does not cause pain or discomfort for the patient. However, an MRI scanner does not always obtain a holistic and detailed picture of an organ, which is due to the specific structure of the gastrointestinal tract. For example, the stomach and esophagus are clearly visualized on the MRI screen, but intestinal loops layered on top of each other hide some areas from the scanner. In this case, a more effective method is colonoscopy, since the introduction of an endoscope into the rectal cavity makes it possible to view every centimeter of the large intestine, and during diagnosis, carry out therapeutic procedures. At the same time, the small intestine and terminal parts of the large intestine are clearly visualized on contrast-enhanced MRI. Medical practice shows that both methods have both disadvantages and advantages, therefore they are often carried out in combination. Before prescribing a diagnosis, the specialist studies data on the patient’s preliminary diagnosis and his individual characteristics, after which he decides that a colonoscopy or MRI of the intestinal tract will be more effective.
Research methods - colonoscopy and MRI
Which is better when diagnosing gastrointestinal diseases - MRI of the intestines or colonoscopy - depends entirely on the symptoms, the development of which will lead to a preliminary diagnosis. Each method has its own advantages and disadvantages, which should be taken into account when prescribing such a research method. It is up to the doctor to finally decide which method will be most effective in diagnosing a particular disease. In addition, doctors’ arsenal includes other, no less effective methods for examining patients with gastrointestinal diseases. Among them:
- X-ray examination - irriography is usually prescribed, where X-rays can determine intestinal pathology. The group of X-ray examinations also includes MRI, despite the fact that X-rays are not involved in this examination.
- Laboratory diagnostics - in which blood is donated from a vein for the presence of tumor markers in it when diagnosing intestinal cancer, refers to non-instrumental diagnostic methods.
- Endoscopic examinations - a group of which includes colonoscopy - a special device equipped with optics is inserted by a doctor into the intestines to examine and study the structure of the organ or the presence of pathologies in it.
MRI of the intestine and colonoscopy are fundamentally different research methods in purpose and essence. But for many patients who are prescribed this or that examination, the main question remains of choice.
MRI of the intestine or irrigoscopy method?
Irrigoscopy is an X-ray method for examining the intestinal tract, in which a barium suspension is injected into the patient’s rectal cavity. The method is atraumatic and painless, but not absolutely safe, since the procedure technology involves a small dose of radiation. In this regard, the number of irrigoscopy examinations for a patient is limited.
According to the general opinion of experts, irrigoscopy is not the most informative diagnostic method. An X-ray examination is carried out to confirm the results of a standard colonoscopy and visualize areas invisible to the invasive method. However, magnetic resonance imaging is a more effective and, moreover, absolutely safe method. Therefore, if the question arises, which is better, intestinal MRI or irrigoscopy, the answer is obvious.
What does irrigoscopy reveal:
- level of functioning of the intestinal sections;
- the condition of the mucous membrane and its structure;
- structure of the intestinal tract
MRI or CT scan of the intestine?
CT is a modern research technique, the principle of which is based on the influence of x-rays. The method has an alternative name – virtual colonoscopy. But unlike traditional invasive diagnostics, the CT procedure does not involve invasive endoscopy, so the scan is painless.
If we compare whether it is better to examine the intestines with CT or MRI, we can note that both methods give similar results. Computed tomography, like MRI, may not be sufficiently informative in identifying formations smaller than 0.1 cm. Thanks to MRI, it is possible to study in detail the condition and structure of soft tissues, as well as the nature of the pathology in them, the degree of damage, and the prevalence of the abnormal process. Like MRI with contrast, CT visualizes hemorrhages, hematomas and neoplasms with high accuracy. In terms of safety, MRI is an impeccable leader, since the MRI scanner creates a magnetic field that is not harmful to health and is allowed to be used even during pregnancy. However, there are contraindications to MRI (metal objects in the patient’s body, prosthetics, fragments, fear of confined spaces, etc.) In such cases, computed tomography is prescribed.
What does a CT scan reveal:
- intestinal anatomy;
- structural relief of the mucous membrane;
- inflammatory processes;
- tumors of any nature;
- localization of metastasis
Advantages and disadvantages
This method is used using a contrast agent, which is absolutely safe for patients and is easily and quickly eliminated by the body. If a contrast agent was not used, intestinal MRI would have low informativeness and diagnostic efficiency. The examination itself lasts about an hour. During this time, patients are advised to remain in a relaxed state, but not to sleep, since in their sleep they may move, which will disrupt the entire study as a whole. To securely fix it, special belts are used to fasten it to the table surface. Despite the high percentage of positive qualities, intestinal MRI is not a leader in the diagnosis of diseases of the large and small intestine. Flaws in pathology visualization, the high cost of the study, the length of stay in the camera of the device, and, compared with colonoscopy, the inability to carry out local intestinal therapy or take pathological material (biopsy) for further research.
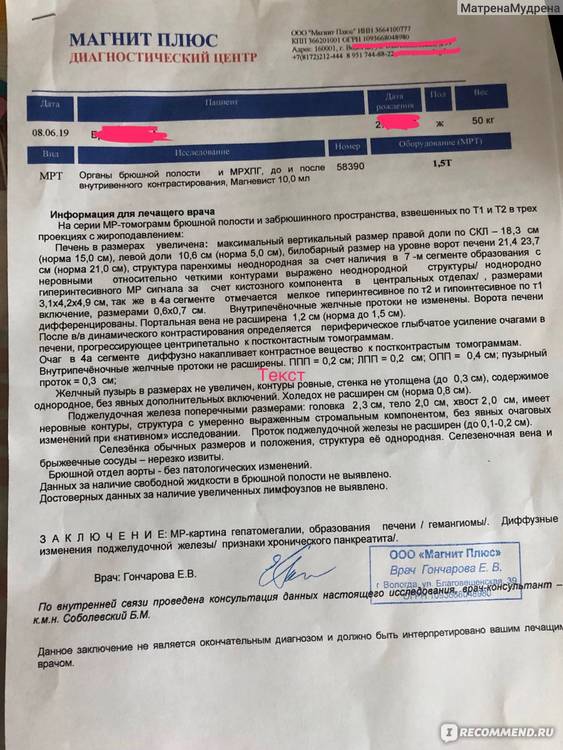
MRI of the abdominal cavity, retroperitoneum and cholangiography - review
Hi all! Today I will talk about magnetic resonance imaging of the abdominal cavity.
On an ultrasound of the abdominal cavity, the doctor discovered some strange formation in the liver of quite large size and recommended an MRI with contrast to determine what it was. I admit, I was scared. Some diagnoses began to flash through my brain, one more terrible than the other. A tumor always sounds scary, even if it is benign. Abdominal MRI with contrast plus cholangiography are quite expensive. The insurance company (VHI) did not want to approve it for me. After 10 days they gave up and I signed up for the procedure.
Cost: from 6500 plus contrast from 1500 rubles plus each photo 300 rubles. No budget.
Preparation. The clinic administrator sent me a detailed SMS describing the preparation for the examination.
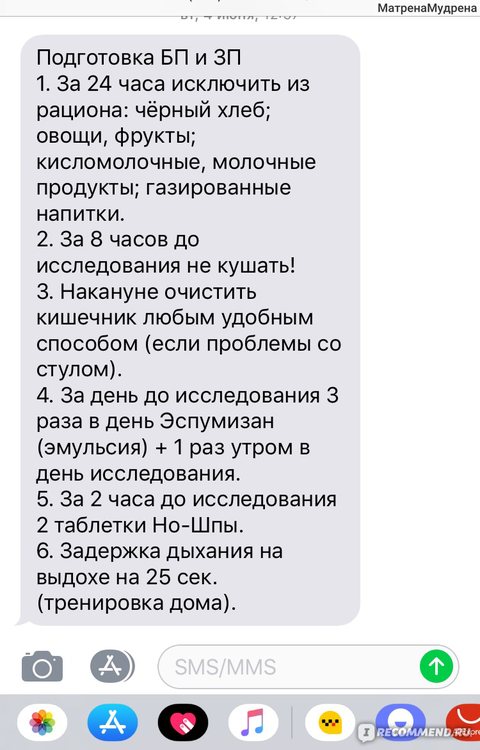
The preparation is simple, but all instructions must be strictly followed! If you do not follow a diet, the image will be uninformative.
The administrator also asked if I was allergic to medications, if I had any metal implants in my body, and also if I suffered from claustrophobia.
Before this, I had an MRI of the brain twice. The sensation is not pleasant, but it is a quick procedure that does not require any preparation. But with MRI of the abdominal cavity the situation is the opposite. First, preparation. Secondly, it's long: 40 minutes
I was scheduled for an examination on Saturday at 7 am. This is convenient because you can’t drink or eat in the morning. You need to take with you a cotton shirt or T-shirt, all documents and a referral for examination.
Before the procedure, the doctor asks again about allergies, etc.
I changed into a T-shirt and shorts (it is important that you are not wearing any metal objects). The doctor laid me on the tomograph bed, inserted a catheter into a vein, put headphones on me and gave me instructions. According to his command, for about 20 minutes you need to hold your breath as you exhale for 25-30 seconds and not move. This is not as simple as it might seem at first glance, because holding your breath while exhaling is more difficult than holding your breath while inhaling.
At the same time, the tomograph makes a very loud noise and knocks; it is practically closed. After 10 minutes, I began to feel dizzy, but the doctor in headphones constantly reassures me, and I also have an emergency stop button for the tomograph in my hand)))).
After 20 minutes you need to start breathing, adjusting your breathing to the tomograph. The better you do this, the faster the procedure will end.
After the end of the study, the conclusion is issued approximately 2 hours later. It includes a recording disc and a paper report.
I did it...)) Preparation and procedure for fluoroscopy, irrigoscopy!
I need this before gynecological surgery...
Before X-ray examination (X-ray of the stomach and 12 intestines) - this is easy and no special preparation is needed:
in the evening, do not have dinner after 18-00, so that your stomach is empty in the morning.
But for irrigoscopy (x-ray of the intestine), you need to carefully prepare yourself.....
But when you drink more...after an hour your stomach starts to swell, you don’t even want to eat anymore and you think when will it all end.....
Honestly, drinking 3 liters is very difficult, it was mentally difficult for me and in general...
Saw 1 pack. for 1 glass, I drank about 3 liters, even a little less and only 12 sachets for MY 62 kg. (whoever has more, then 15 or more needs to be diluted and drink 4 - 4.5 liters)
After 2 hours it started……the first stool…..then liquid….
If you have a choice between colonoscopy and irrigoscopy, do the latter, do not torture yourself and your psyche; if the former, they recommend anesthesia.
I did it for a fee, because... they didn’t want to send insurance…….
For those who need to do such procedures, don’t worry and tune in for good results, I wish you to be healthy!
Colonoscopy or tomography, which to choose?
Colonoscopy and intestinal tomography occupy an important place in the modern arsenal of diagnostic procedures. Both types of examination are highly informative, but for each of them there are certain indications. How do these methods differ, and what is better in each specific case: CT scan or intestinal colonoscopy?

Computed tomography (CT) is based on the use of X-rays. As a result of an examination using this technique, the doctor receives documented layer-by-layer images of certain areas of the body. In the case of intestinal tomography, the abdominal cavity is specifically examined. The prepared patient is placed on a special surface, which then passes through a kind of mini-tunnel. This device is referred to as a computed tomograph. Inside the capsule through which the subject is advanced, an X-ray tube moves in a circle. The rays are absorbed by a receiver mounted opposite the radiation source. All collected information is transferred to a computer and digitized into a series of images. Thus, in a fairly short period of time, the diagnostician receives many high-quality images with a slice difference of about 1 mm.
All located structures and formations of the abdominal cavity are clearly visible on tomograms. In this case, it is impossible to assess the nature of the internal lining of the intestine.
During a colonoscopy, the doctor examines the mucous membrane of the distal gastrointestinal tract using a special optical system inserted through the rectum. New generation endoscopes display images on a monitor, which simplifies the specialist’s work, allows a more accurate assessment of the condition of the intestinal mucosa and reduces the risk of diagnostic errors.

To obtain high-quality results both in the case of colonoscopy and intestinal tomography, it is necessary to carry out proper preparation. In both cases, the patient is prescribed a slag-free diet and laxatives according to a specific regimen for several days before the examination. Combined salt preparations or drugs based on macrogol are used. The night before and immediately before the examination, stop all food intake, including minor snacks. In addition, the patient comes to the diagnostic procedure strictly on an empty stomach (you shouldn’t even drink in the morning).
Computed tomography method
CT scan of the intestines is performed in the following situations:
- Suspicion of tumors, as well as metastases in the abdominal cavity and intestines. It is possible to determine the location and nature of a formation larger than 1 mm, but it will not be possible to take material for a biopsy or destroy polypous growths.
- Study of the intestine in the presence of adhesions, large tumors, pronounced narrowing of the lumen of the intestinal tube, preventing the insertion of a colonoscope.
- The need to examine the colon in case of general exhaustion of the patient, including in the elderly.
There is a method with contrast, when the intestine is more clearly visualized using a special substance. In this case, the subject is recommended to drink a barium preparation a couple of days before the procedure, or immediately before the tomography, an iodine-containing agent is injected into a vein.
Bowel examination methods

All pathological processes are concentrated in the large intestine: fecal masses accumulate here, provoking inflammatory processes. In modern medicine, there are many ways to assess the condition of the digestive tract. The most reliable are colonoscopy and MRI. Other diagnostic methods also help the doctor make the correct diagnosis, such as:
- Ultrasound of the intestines;
- irrigoscopy, during which X-rays can be taken;
- virtual research using a computer program, when a special capsule is taken - a sensor.
Colonoscopy of the intestine

- Duphalac - instructions for use for adults and children
- Shellac lamps - which one is better to choose. How much does a shellac lamp cost, price
- Megafon - subscriber tracking, connection. How to disable the Radar service on Megafon
This method appeared in the last century along with video endoscopic technology. Doctors admit that colonoscopy is the most reliable way to examine the intestines. The procedure is also called video colonoscopy, because is carried out using a thin, flexible fiber colonoscope, which is equipped with a micro-camera. If a specialist notices pathological changes during the examination, then during the procedure he can pinch off a piece of tissue for a biopsy. Indications for fibrocolonoscopy:
- detection of colitis;
- detection of mucosal polyps;
- confirmation of oncology.
Careful preparation for colonoscopy is the key to a high result of the procedure:
- Eating light, diet foods for several days. You should exclude foods that cause gas formation: legumes, carbonated drinks, cabbage.
- The day before the colonoscopy, meals are canceled and you are allowed to drink water and herbal decoctions.
- Colon cleansing is carried out by the patient independently the day before the procedure or in the clinic. As a result, the stool should be transparent.
- Those suffering from constipation need to take laxatives until the intestines are completely cleansed.
The examination procedure is contraindicated in case of hemorrhoidal bleeding or severe inflammation of the rectum. The session lasts about half an hour, during which the patient may feel some discomfort in the form of bloating and intestinal spasms. Goes through the following stages:
- Local anesthesia is administered.
- The doctor carefully inserts the colonoscope rectally.
- The intestinal walls are sequentially examined.
- For a painless examination, gas is injected into the colon to straighten out the kinks of the intestine so the patient may feel bloated.
Magnetic resonance imaging

This is a highly accurate method for examining the thin and thick digestive organs, which helps to detect the smallest problems in the early stages. MRI is an absolutely safe and painless method. Depending on the complexity, the procedure lasts from ten minutes to half an hour. The results of the study can be obtained on the same day. MRI perfectly distinguishes soft tissues, and an experienced specialist can easily see all the most remote areas of the organs being examined. Indications for tomography:
- inflammatory diseases of the digestive tract;
- frequent constipation;
- polyps of the intestinal mucosa;
- pathological changes during pregnancy;
- hemorrhoids at different stages;
- intestinal oncology.
Before performing an MRI, the following preparations must be made:
- the day before, the patient is prescribed a diet that must be followed for three days before the procedure;
- do not eat food 12 hours before the procedure;
- purging with a laxative until the stool becomes clear.
- How often should you wash your hair with shampoo?
- Chocolate sausage from cookies: recipes
- HIV infection - how it is transmitted. Symptoms of human immunodeficiency virus and treatment, diagnosis and prevention
During magnetic resonance imaging, a specialist has the opportunity to most accurately assess the condition of the organs being examined thanks to the display of a three-dimensional image on the monitor. The procedure is carried out as follows:
- the patient must remove all metal products;
- the patient is placed on the exit surface, fastened with fixing belts;
- the patient is then placed in a tomograph, where a magnetic field is used to create a scan of the organs being examined.
The entire session takes about one hour, during which the patient can relax and even sleep. The only discomfort of this procedure is the obligatory complete immobility of the body. Magnetic diagnostics is contraindicated in the following cases:
- Tomography cannot be performed if the patient has built-in, internal metal elements: cardiac stimulators, intrauterine device in women, dental implants, plates for healing bone tissue in fractures;
- Magnetic tomography is dangerous in the first two months of pregnancy;
- The procedure is impossible for young children; at this age, a child cannot maintain complete body stillness for a long time.
Colonoscopy technique
Endoscopic examination is indicated in the case of:
- suspicion of an oncological process in the intestine;
- inflammation of the colon;
- intestinal polyposis;
- the presence of erosive, ulcerative colitis.
One of the decisive points in prescribing an invasive diagnostic method using an endoscope is the possibility of taking biopsy material, as well as simultaneously converting colonoscopy into a treatment procedure for removing polyps.
The question of what study the patient needs: CT scan of the intestines or colonoscopy is decided only by the attending physician.
Patients' attitude
Patients who are scheduled for a colonoscopy worry about the pain of the upcoming procedure. Often these fears are justified, since the presence of intestinal pathology (strictures, ulcerations, abdominal adhesions) increases the discomfort when passing the endoscope through the intestinal loops. Tomography from this position involves minor discomfort when air is pumped into the intestine to improve visualization, but is generally perceived painlessly.
Thus, with CT there is no need for anesthesia, in contrast to the often arising need to use sedation during colonoscopy. It is known that patients react differently to the effects of sedatives, from calm recovery from drug-induced sleep to intolerance to anesthesia. Therefore, it is important to fully inform the anesthesiologist about your state of health and the presence of allergies.
Only when prescribing a tomographic examination in childhood, doctors resort to the use of sedation, since it is difficult for a small patient to maintain a strictly motionless posture at the time of the examination.
Objective differences between methods:
- Computed tomography is based on the physical action of x-rays and has a low radiation dose. Colonoscopy is based on a simple examination of the intestinal mucosa through a magnifying device.
- Tomographs currently used can withstand patient weights of up to 150 kg, while endoscopic examination has no restrictions on the weight of the subject.
- When performing a CT scan, there is a high probability of missing space-occupying formations up to 1 mm in size; colonoscopy allows you to see any changes in the intestinal mucosa and tumors in the submucosal layer.
- Tomography gives an idea of all the organs of the abdominal cavity; using an endoscope, the doctor assesses only the condition of the intestinal wall.
- CT scanning does not result in complications such as intestinal damage up to perforation.
- Only colonoscopy allows you to take a biopsy specimen for histological examination, remove polyps, and stop bleeding.
Indications for MRI of the intestine
In the vast majority of regions of the Russian Federation, the price for an MRI of the stomach ranges from 2.5 to 5–7 thousand. However, medical institutions that use ultra-precise professional equipment can indicate a cost of 10–24 thousand rubles.
Doctors strongly discourage patients from saving on their health: conscious consent to diagnostics using an old-generation device with poor quality resolution in some special cases is fraught with serious consequences.
Most often, magnetic resonance imaging is used to identify malignant tumors in the stomach and intestines. This method allows you to detect metastasis. To obtain more detailed information, a contrast agent is used, which is injected into the patient’s body on the eve of the study.
Indications for MRI:
- Determination of anomalies in the development of the vascular network and internal organs.
- Lack of alternative diagnostic options.
- Detection of foreign bodies in the large intestine.
In the presence of intestinal cancer, magnetic resonance imaging can be used to identify the nature of the formation, the area of localization and the structure of metastases, if any. After surgery, during the rehabilitation period, using this diagnostic measure, you can monitor the scarring process.
Your doctor may prescribe a magnetic resonance imaging scan of the stomach if:
- suspects that the walls of the stomach are affected by cancer;
- there are anomalies in the structure of the abdominal organs that are congenital in nature;
- there is bleeding and its source is known;
- the problem is related to intestinal obstruction;
- there are stones;
- the symptoms of the disease are quite weak;
- an inflammatory process develops in the gastrointestinal tract cavity, which complicates diagnosis, affecting its accuracy;
- correction of the course of therapy for oncology is required;
- the ulcer affects large areas, accompanied by hemorrhage;
- it is necessary to confirm the presence of metastases in oncological processes and determine the stage of metastasis;
- there are foreign objects in the intestines;
- It is not possible to examine the gastrointestinal tract in other ways.