What are antispasmodics
Antispasmodics are medications with a special mechanism of action aimed at relaxing muscle microfibers in the walls of blood vessels and any internal organs with a smooth muscle structure. Antispasmodics used in gastroenterology are intended to relieve spasm of the smooth muscles of the abdominal organs, including the pancreas, as well as the walls of blood vessels in areas of spasm.
The therapeutic properties of these pharmacological agents include:
- relaxation of the muscles of the digestive system, including the ducts of the pancreas and bile ducts;
- elimination of pain caused by convulsive contraction of muscle fibers of the digestive system;
- reduction in the excretory activity of the pancreas; decreased secretion of hydrochloric acid;
- dilatation of blood vessels, bronchi, stimulation of the heart, reduction of pressure.
Antispasmodics not only relieve pain, but also activate blood supply to organs. In addition, the use of these medications does not directly affect the mechanism of pain sensitivity and therefore does not complicate the diagnosis in any way.
Indications and contraindications
Pancreatitis is a common disease among all pathologies of the digestive system. The disease can occur in acute or chronic form, which affects treatment and the route of administration of medications. It is important to follow a regimen and diet, especially if it is chronic and the patient is being treated at home. In this case, pancreatic injections may not be necessary.
Indications for injections:
- Acute condition.
- Intense pain syndrome that is not relieved by pills.
- Inability to administer drugs orally.
- High body temperature that cannot be reduced by other means.
Severe pain is an indication for an injection.
Among the contraindications are: intolerance to the drug. Pregnancy and lactation are reasons to refuse injections.
How do antispasmodics act in illness?

If this is the first time an attack has occurred, it can be very difficult to immediately determine the source of pain. For such cases, there is a diagnosis of “acute abdomen” and a standard of care for it - until the causes of this condition are clarified. In order not to miss a catastrophe in the abdominal cavity, such as a perforated stomach ulcer, acute appendicitis, or, worse, developing peritonitis, there are drugs from the group of antispasmodics that will help relieve pain and not blur the picture of the disease. One of the most common causes of pancreatitis is swelling or blockage of the excretory duct. The purpose of the drug is to eliminate this spasm, after which the normal outflow of pancreatic and bile juices is normalized. In case of chronic uncomplicated pancreatitis, Duspatalin, which is available in tablet form, can be used for these purposes. With long-term use of this medicine in patients with chronic pancreatitis, stable remission can be achieved.
In acute pancreatitis, preference is given to the injection of antispasmodic drugs. In an acute process, the pain syndrome is so intense that minutes count. Each additional second of acute pain causes severe suffering to the patient and can lead to painful shock. In these cases, injectable forms of antispasmodics are used, which quickly relieve spasms and partially eliminate pain.
How the medicine is used
Since acute pancreatitis is an urgent condition, drugs are used only by injection for several days from the onset of the disease: in the form of injections for treatment or droppers. This speeds up pain relief and prevents the development of life-threatening complications. The earlier treatment begins, the higher the likelihood of recovery.
Bibliography
- I.V. Maev, Yu.A. Curly. Diseases of the pancreas: practical work. Management. M.: GEOTAR-Media, 2009.
- Mashkovsky, M.D. Medicines: A manual for doctors. M.D. Mashkovsky. M.: New. Wave, 2013
- Kryzhanovsky, S.A. Modern medicines: More than 10,000 items / S.A. Kryzhanovsky, M.B. Vititnova. M.: Ripol-Classic 2009
- Stupin V.A., Mikhailusov S.V., Moiseenkova E.V. Paresis of the gastrointestinal tract with pancreatic necrosis. XII Congress of Russian Surgeons in conjunction with the National Surgical Week “Current Issues in Surgery”, October 7-9, 2015. Rostov-on-Don.
The source of pain impulses in pancreatitis, or “what hurts”
The mechanism of pain development in acute pancreatitis has many components. This is swelling of the gland and overstretching of its capsule, this is a spasm of the sphincter of Oddi, this is a reflex spasm of the bile ducts and gallbladder, this is spastic pain in the small intestine. This is an autonomic reaction in response to a powerful release of cortisol and adrenaline - the hormones of fear and stress - that accompany an attack. Almost everywhere there is a spasm of the smooth muscles of the abdominal organs, which means that by acting on it with the help of specific drugs (antispasmodics), you can significantly alleviate the patient’s condition.
Instructions for use
All antispasmodics must be used strictly in accordance with the doctor’s instructions, subject to an accurately established diagnosis.
Antispasmodics for children
Each manufacturer indicates the specifics of taking its form of the drug in children. For example, in some forms drotaverine is not used in children under 2 years of age, in others the recommended daily dose for children aged 1-6 years is 40-120 mg (in 2-3 doses), for children over 6 years of age - 80-200 mg (in 2-5 doses). Hyoscine butyl bromide is prohibited for children under 6 years of age. Pinaveria bromide is not recommended for people under 18 years of age. Natural antispasmodics (infusions and decoctions, as a rule) are prepared from individual plants or from collections containing flowers, roots, leaves, stems. They are prescribed to children for various diseases accompanied by spasms or convulsions.
Antispasmodics for newborns
Antispasmodics for newborns are very limited for use; there are only a few names that pediatricians allow to give to children. The M-anticholinergic drug priphinium bromide in certain forms relieves spasms and relieves pain. Infants up to 3 months. it is prescribed orally in the form of syrup, 1 ml every 6–8 hours; from 3 to six months - 1-2 ml every 6-8 hours, from 6 months. up to one year - 2 ml every 6-8 hours; from 1 to 2 years - 5 ml every 6-8 hours. Children are also prescribed herbal preparations containing natural antispasmodics - peppermint, fennel oil, anise, dill.
Antispasmodics for pregnant women
Antispasmodics should be prescribed to pregnant women with caution, only if the expected benefit from therapy outweighs the potential risk to the fetus. For many drugs there is no clinical data for pregnant women; for some, pregnancy is a contraindication (bencyclane, dicycloverine, hyoscine butyl bromide).
Antispasmodics during lactation
In general, it is not recommended to prescribe antispasmodics during lactation, or drotaverine and bendazole are prescribed with caution (in some forms, only if the potential benefit is greater than the harm to the child). Breastfeeding should be discontinued while taking oxybutynin.

Analgesic injections
It is recommended to anesthetize the pancreas due to the inflammatory process in it in an acute state of the disease with the help of NSAIDs.
Paracetamol. Treatment of inflammation of the pancreas with this remedy is due to its effect on reducing elevated body temperature, eliminating pain and reducing the degree of development of the pathological process in the organ. Injections for pancreatitis with this drug are carried out using a solution with a dosage of 10 milligrams of the active substance per milliliter.
Baralgin. This remedy helps cure the disease due to several of its beneficial properties. Among them, it is worth highlighting pain relief in the pancreas, eliminating spasms of muscle fibers, eliminating inflammation to some extent and reducing body temperature. An adult can use solutions of 2.5 and 5 milliliters, both for injections and for droppers. The drug can also be combined with some other medications that can relieve inflammation.
Analgin. Like many other medications, this drug has three quite important therapeutic effects: pain relief, reduction of elevated body temperature and reduction of inflammation. The drug is available in ampoules of 1-2 milliliters with a solution of 0.25% or 0.5% of the active substance.
Sandostatin. It is a synthetic analogue of Somatostatin. The medicine is prepared in the form of an injection solution or lyophilisate for its preparation. One medicinal ampoule, whose volume is 1 milliliter, may contain a dosage of 0.05 mg or 0.1 milligram of the active substance. Sandostatin can help the pancreas due to the fact that it inhibits the degree of secretion of this organ, as a result of which pancreatic juice is produced in an insignificant volume. Often this drug is prescribed to patients after undergoing surgery. Almost every review about the use of this tool on the Internet is positive.
Injections for the pancreas in the treatment of pancreatitis should only be prescribed by the attending physician of a sick person after a comprehensive examination.
It is prohibited to carry out therapy on your own, since any drug has a whole list of contraindications and side effects.
How does an antispasmodic work for chronic pancreatitis?
As is known, the cause of the development of pancreatitis is most often a blockage of the main pancreatic duct due to spasm of the sphincter of Oddi - the opening through which pancreatic juice and bile enter the duodenum. Relieving spasm and further normalizing sphincter tone - this problem is successfully solved by duspatalin in chronic pancreatitis. This drug is used only in oral forms - tablets and capsules, and is therefore not suitable for emergency care. However, its long-term use (up to 24 weeks) for chronic pancreatitis allows achieving stable remission.
Remedies for pancreas
In case of development of pancreatitis, injections are prescribed not only for the purpose of relieving painful sensations. With prolonged progression, the disease transforms into a chronic form. This helps to reduce the concentration of insulin in the blood, after which diabetes develops.
Chronic pancreatitis requires injections of the hormone insulin. During an exacerbation of the pathology, the patient is prescribed antibiotics. Gentamicin is considered the most powerful drug. It is injected into the muscle 2-4 times/day. Prescribing this medicine helps to avoid the occurrence of purulent complications.
Basic painkillers for acute pancreatitis
With pain in the pancreas, inflammatory mediators are released that have a destructive effect on other organs of the digestive system: the symptom increases and can last for several days if emergency assistance is not provided. Painkillers are prescribed as quickly as possible, since not only the patient’s physical health suffers, but also his psychological state.
If pain relief is necessary, in order to quickly alleviate the patient’s condition, any drug from the following groups is used:
- myotropic antispasmodic;
- non-steroidal anti-inflammatory drugs (NSAIDs);
- non-narcotic or narcotic analgesic;
- anesthetic.
It is possible to relieve pain before the ambulance arrives by taking an antispasmodic. This drug will partially relieve pain and will not blur the overall clinical picture of the disease.
A suitable painkiller for the pancreas is No-shpa (Drotaverine): an adult can give the injection themselves. There is no point in taking a pill in this state, since severe pain is accompanied by nausea and vomiting.
Narcotic analgesics and anesthetics are prescribed exclusively in hospital settings under the supervision of a physician. They are used in an unsuccessful attempt to relieve pain with antispasmodics and NSAIDs, which are non-narcotic painkillers.
Fentamil or Promedol are prescribed in case of severe complications (for example, necrosis) and increased pain. The presence of indications and hospital conditions allow for pain relief with narcotic painkillers.
Anesthesia involves the use of novocaine medications (Novocaine, Lidocaine). This is carried out by medical specialists; the condition for this is that the patient is in the surgical department or in the intensive care ward. Sometimes novocaine blockades of the solar plexus are carried out in gastroenterology conditions.
Acute inflammation with severe pain must be relieved by parenteral administration of drugs: with this method of administration, they act almost immediately. Painkillers for pancreatic pain are used for mild exacerbation or for chronic disease.
Mechanism of pain
The intensity, nature and localization of pain in pancreatitis is influenced by multiple processes that occur in the tissues of the pancreas - obstruction and inflammation of its ducts, ischemia, degenerative changes. However, as most patients note, pain occurs 30 minutes after eating.
In acute pancreatitis, an intolerable burning pain occurs that increases every minute. Traditional methods of pain relief do not help a person - neither the “fetal position” nor the semi-sitting position. Usually the pain is localized in the upper abdomen, sometimes in the left hypochondrium.
The main symptom of acute pancreatitis is sudden pain that rapidly increases. Also, the acute form of the disease may be accompanied by the following symptoms:
- increased body temperature;
- increased heart rate;
- nausea and vomiting.
In the chronic form of the disease, a person is usually bothered by pain of varying degrees of intensity, which can be localized in the upper abdomen, back and even lumbar region. Typically, pain intensifies after eating or drinking alcohol.
Sometimes it happens that after severe pain relief comes. You should not rejoice in advance, because this situation may be a sign of necrosis of a large area of the pancreas.
The main difference between acute pancreatitis and the chronic form of inflammation of the pancreas is the rapid development of the first option. In this case, 3–7 days pass from the appearance of the first symptoms to the onset of irreversible processes in the diseased organ.

The following factors can provoke an acute attack of pancreatitis:
- unhealthy diet and overeating;
- drinking alcohol;
- exacerbation of gastrointestinal diseases;
- taking certain medications;
- poisoning;
- abdominal trauma;
- stress.
The effect of antispasmodics in acute pancreatitis
Acute pancreatitis is sometimes accompanied by a pain syndrome of such intensity that it can cause the development of painful shock and lead to the death of the patient. Therefore, you cannot hesitate here: only injection antispasmodics bring quick relief. These are well-proven no-spa, platyphylline and papaverine. If the patient does not vomit, no-shpa can also be used in tablets, but when administered intravenously, its effect begins already from the second minute. Which is important for the patient’s psychological state - after all, every minute filled with pain becomes an hour for him.
Papaverine is similar in its effect to no-shpa; it is a drug with a minimum number of side effects and a selective effect on the smooth muscles of the abdominal organs. Its disadvantages, perhaps, include a relatively short period of action - about four hours, after which the injection must be repeated.
The most powerful remedy that permanently eliminates spasms of smooth muscles of internal organs is platiphylline; it is administered every 12 hours in a dose of 1-2 mg, subcutaneously or intramuscularly. However, symptoms of side effects with platyphylline are more frequent and more serious than with other antispasmodics. Therefore, the use of the drug is recommended only under medical supervision.
Signs indicating the development of pancreatitis
Inflammation of the pancreas is preceded by several factors. Initially, the patient begins an attack of cholecystitis, which is caused by drinking alcoholic beverages or overeating fatty, spicy foods.
Various forms of pancreatitis are most often observed in women who suffer from gallstone disease, as well as in representatives of the stronger sex who abuse alcohol. Discomfort in the pancreas area can be caused by pressure on the abdomen from a belt or belt. Then the pain increases, the patient complains of a strong, bursting pain inside, radiating to the upper part of the abdominal cavity. Pain surrounds the whole body.
The acute phase of inflammation of the pancreas is accompanied by severe vomiting, which does not bring relief. Sometimes blood clots are present in the vomit. The temperature, as a rule, does not rise. The patient experiences severe pain, which can be relieved only after an injection with painkillers or antispasmodics.
Painkillers for chronic pancreatitis
Chronic pancreatitis is also characterized by pain. But in most cases it depends on how severe the inflammatory process is. The intensity of the attack of pain is inferior to that that accompanies acute pancreatitis. There may be no high temperature, and vomiting does not always occur. Therefore, in some cases it is possible to take any drug in tablet form:
- No-spa, papaverine, Duspatalin (Meteospasmil) - pain relief with these antispasmodics is effective, even if other nearby digestive organs are involved - the stomach, gall bladder, liver, and gastritis and cholecystitis are aggravated.
- Analgin, Baralgin are analgesics, the use of which is permissible if the disease is chronic, with moderate pain symptoms.
- Indomethacin, Movalis, Ketanov are NSAID drugs; taking them at home allows for good pain relief, even if you do not give an injection, but take a pill.
If the tablet does not produce the desired result, the drug is prescribed in the form of intramuscular, intravenous injections or infusions. This method of administration has advantages: it quickly and effectively relieves pain of any intensity.
Features of action for pancreatitis
One of the basic symptoms of pancreatic inflammation is pain. The reasons for its occurrence are several main factors:
- obstruction of the main excretory duct of the gland due to spasm of the so-called sphincter of Oddi - a muscular ring with an opening through which pancreatic juice and bile flow into the duodenum;
- abnormal stretching of the capsule of the inflamed organ;
- reflex spasm of the bile ducts and gallbladder;
- spasmodic contractions in the small intestine.
In acute attacks of pancreatitis, cutting, often unbearable, girdle pain can lead the patient to a state of painful shock and death. To relieve the intensity of pain and prevent shock, antispasmodics are immediately used to relax the muscle ring of Oddi, eliminate obstruction of the excretory ducts and open the way for juice and bile into the small intestine.
An acute attack of pancreatitis requires injection of medicinal solutions that have a powerful and accelerated therapeutic effect. Antispasmodics are intended to relax the smooth muscle organs of the gastrointestinal tract, spasmed in the local area of the abdominal cavity, head, heart, etc. For mild dull pain and the absence of vomiting, medications to relax the smooth muscles of the abdominal organs and eliminate pain syndrome are prescribed antispasmodics in the form of tablets.
Destination Features
Before moving on to complex treatment of pancreatitis and prescribing injections, the doctor establishes an accurate diagnosis, the stage of the disease, and identifies the presence of complications and concomitant pathologies.
In acute form
To block the development of pancreatitis, a medical specialist prescribes antispasmodics and analgesics in combination with antienzyme medications and antacids.
In this case, injections help cope with inflammation of the pancreas and prevent the development of complications. The choice of drug depends on the cause of the exacerbation and the patient’s condition.
In the chronic stage
In the chronic form of pancreatitis, injections are prescribed to normalize the process of food digestion, absorption of nutrients, and also to prevent the development of diabetes.

In chronic pancreatitis, injections are prescribed to prevent the development of diabetes.
Therapy occurs with the use of those drugs that provide the pancreas with the necessary enzymes. If pain occurs, it is important to immediately administer an anesthetic injection so as not to cause additional damage to the person’s health and prevent dehydration.
During exacerbation of the disease
In case of exacerbation of pancreatitis, painkillers are prescribed carefully and only after the cause has been established. Injections are used to relieve pain, produce enzymes and secretion, reduce the load on the pancreas and relieve swelling.
Cholecystopancreatitis
For cholecystitis, the doctor prescribes antispasmodics (to relieve pain and spasms), antibiotics (to eliminate inflammation), enzymes (to normalize digestion) and vitamins.
In this case, the use of drugs in the form of injections is especially important, since such treatment avoids negative effects on the stomach and gives immediate results.
For pancreatitis and gastritis
With this form of the disease, the doctor prescribes injections that help reduce the production of hydrochloric acid and inhibit the action of enzymes. Antacids are also used to protect the gastric mucosa.
How do antispasmodics work?
Pain caused by pancreatitis can be caused by many factors, for example:
- swelling of the pancreas;
- gallbladder spasm;
- spasm in the small intestine;
- almost always - a spasm of smooth muscles.
The main purpose of antispasmodics (in gastroenterology) is to reduce spasm of smooth muscles in the complex treatment of abdominal pain of varying intensity. Once in the body, the active substance dilates blood vessels and has a myotropic effect.
All antispasmodic drugs must be prescribed by a doctor; self-treatment can lead to a worsening of the condition and erase the clinical picture of the disease, which will make it very difficult to make a correct diagnosis.
In the complex treatment of pancreatitis, several types of drugs are used to help relieve pain from smooth muscle spasms. These include:
- Nosh-pa (or Drotaverine);
- Papaverine;
- Atropine;
- Nyaspam;
- Duspatalin.
Anti-inflammatory
The mechanism of action of nonsteroidal anti-inflammatory drugs (NSAIDs) for pancreatitis is aimed at inactivating the processes that cause pain and fever. In addition, injections with NSAIDs promote vasodilation and the influx of leukocytes to the affected area.
Inflammation is effectively eliminated by injections with Diclofenac solution. This group of drugs includes Indomethacin, Ketoprofen, Ibuprofen, and Aspirin.
The latter is prescribed to patients with pancreatitis and concomitant cardiovascular pathologies.
Injections with NSAIDs are used in conjunction with coating agents (Maalox, Almagel) or antisecretory agents (Pariet, Omez, Omeprazole) and are prohibited for gastrointestinal diseases. The dosage of medications for injections is prescribed by the doctor, depending on the nature of the inflammation and the stage of development of pancreatitis.
Effective antispasmodic drugs
The degree of therapeutic effect of antispasmodics is largely determined by the severity of the manifestations of pancreatitis, the course of the disease (acute or chronic), the dosage form of the drug (tablets or injections), age and other internal diseases that complicate inflammation in the pancreas. Let's look at the list of the main antispasmodic drugs prescribed for pancreatitis.
Popular Nosh-pa
A very common medicine for abdominal pain, which has proven itself to be an effective remedy. The active ingredient of Nosh-pa is drotaverine - it is a myotropic substance with antispasmodic action. This drug exists in tablets and ampoules for injection. To relieve pain during an attack of pancreatitis, both forms of medication are used. Injections are used to relieve intense pain, since the effect occurs faster (almost immediately after administration of the substance) than after taking pills. The tablets begin to act 20–30 minutes after administration. The maximum daily dose of the drug is 240 mg.
This medicine is sold without a doctor's prescription, but since it has a number of contraindications, it is recommended to consult a specialist before purchasing Nosh-pa.
Contraindications to the use of the drug:
- individual intolerance to components;
- renal failure;
- heart failure;
- lactation period;
- severe forms of liver failure;
- children under 6 years of age.
This drug also has serious side effects:
- cardiopalmus;
- dizziness;
- decreased blood pressure;
- allergic reactions (itching, redness and rashes on the skin);
- injections in rare cases can cause paralysis of the respiratory center.
Considering possible side effects, it is better to use the drug after a complete medical examination of the body.
Drotaverine
Drotaverine for pancreatitis is one of the most common, effective and affordable antispasmodics. The medicine has a long-lasting and pronounced relaxing effect on the smooth muscles of internal organs and blood vessels. It is on the basis of drotaverine that such a well-known drug as No-shpa has been developed, which eliminates spastic contractions of the muscles of the abdominal organs, including the pancreatic ducts.
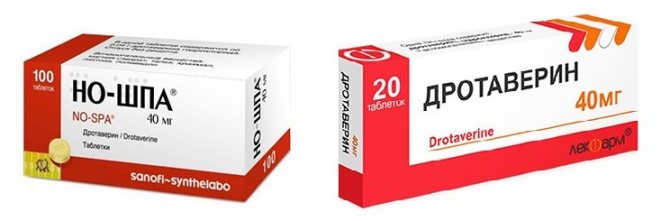
Drotaverine tablets begin to act 25-40 minutes after administration, so they are used in the absence of severe pain and vomiting in the patient. An intramuscular injection of Drotaverine or No-shpa has a therapeutic effect within 5-7 minutes. Contraindications for prescribing drugs based on drotaverine include:
- serious cardiac pathologies, including cardiogenic shock;
- low blood pressure;
- severe kidney and liver dysfunction;
- admission for children under 7 years of age;
- individual intolerance.
During pregnancy and breastfeeding, use with caution.
Papaverine
Papaverine relieves pain in pancreatitis by reducing pressure in the organ caused by spasm of the glandular ducts and restoring the outflow of bile and pancreatic juice. The medication is used in the form of suppositories, tablets and 2% injection solution. Papaverine works most effectively when administered subcutaneously or by drip intravenous infusion. In pediatrics, Papaverine is also prescribed to children. In tablets and suppositories - starting from the age of 6 months, in the form of injections - from 1 year. The dosage is selected by the doctor in accordance with the age and severity of pancreatitis.
There are several forms of release of Papaverine:
- solutions for injections;
- suppositories;
- pills.
Contraindications for Papaverine are the same as for Drotaverine and No-shpa. But Papaverine is also not used in patients with glaucoma and hypothyroidism.
Experts do not prescribe Papaverine in the following cases:
- with some types of arrhythmia, for example, with atrioventricular block;
- severe liver failure;
- for glaucoma;
- decreased blood pressure levels;
- intolerance.
In addition, there is no data on the safety of the use of this substance by children, as well as women during pregnancy or breastfeeding.
Atropine
Atropine for pancreatitis is prescribed as an antispasmodic, which relieves increased tone and spastic contractions in the pancreas. In practice, Atropine is used only in the acute phase of the pathology. Due to the universal mechanism of action and the rapid onset of the therapeutic effect, antispasmodics are often prescribed to eliminate pain due to pancreatitis.
In case of an acute attack of pancreatitis, Atropine is prescribed in the form of injections to block pain only under strict indications and with mandatory medical supervision. The peculiarity of the therapeutic effect of Atropine is due to its ability to enhance the analgesic effect of analgesics - Analgin, Baralgin. Therefore, for spastic pain against the background of pancreatitis, Atropine solution is often administered in combination with painkillers. This can significantly reduce the duration of an acute attack.
Atropine reduces the severity of adverse reactions from drugs, for example, morphine, which must be resorted to in case of painful shock. It should be borne in mind that the medicinal substance in Atropine is an alkaloid that is found in the fibers of poisonous plants - henbane, belladonna, and datura. Therefore, the medicine has serious contraindications and pronounced undesirable effects. In this regard, in pediatrics they avoid prescribing Atropine to children or use it, calculating the dosage strictly in accordance with the child’s body weight.
Antispasmodic Niaspam
Antispasmodic myotropic action - Niaspam. Like other drugs, it affects smooth muscle fibers and does not have an anticholinergic effect. The main substance is mebeverine, available in the form of capsules in a dosage of 200 mg.
The drug is dispensed in pharmacies according to a doctor's prescription. This antispasmodic agent has a number of serious side effects, such as:
- Quincke's edema;
- hives;
- exanthema;
- itching and redness of the skin;
- swelling of the face.
These signs are very dangerous for human health, so before taking the drug it is necessary to take tests and undergo a full examination of the body in order to prevent their occurrence.
The drug is contraindicated for children under 12 years of age, with individual intolerance to the main substance; it is prescribed with caution to pregnant women and women during breastfeeding.
Platyfillin
Platiphylline is a medicine from the group of atropine-like substances, which, in addition to its antispasmodic effect on the smooth muscle tissue of the gland, has a weak sedative effect. A 0.2% solution is used for subcutaneous injection as an emergency treatment to relieve acute attacks of pain. The medicine has an extended list of serious side effects, therefore, like Atropine, it is used only under medical supervision, especially in children.
In cases of exceeding the dosage of Platiphylline for pancreatitis causes the following consequences:
- rapid heartbeat against the background of low blood pressure;
- dry mouth;
- hoarseness of voice;
- intestinal atony;
- disruption of the process of urine emission;
- attacks of severe headache and dizziness;
- seizures;
- photophobia.
Also, when prescribing such a medicine, gastroenterologists take into account such contraindications for use as:
- glaucoma;
- intestinal atony;
- muscle weakness;
- heartbeat disturbance;
- renal and liver failure;
- colitis of ulcerative nature.
The course of treatment of the disease with this drug is from ten to twenty days.
Duspatalin
Antispasmodic, produced in tablets and capsules with the active ingredient mebeverine.
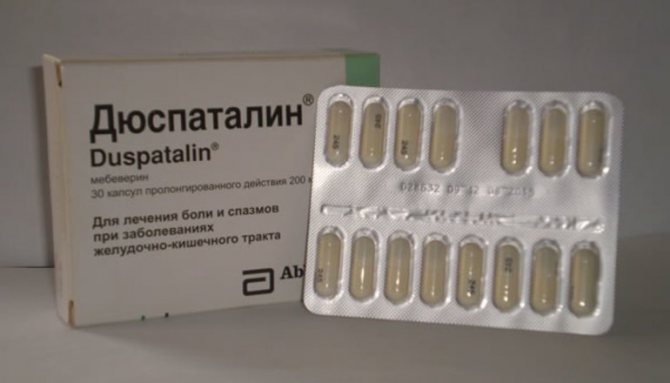
The drug has several positive features for exacerbation of pancreatitis:
- reduces spasm of the main pancreatic duct;
- affects the tone of the muscular sphincter of Oddi;
- improves the functioning of the pancreas, preventing stagnation of pancreatic juice;
- with long-term use shows a minimum of serious undesirable effects.
Duspatalin is not used for emergency care during an acute attack of pain. But long-term treatment (up to 6 months) with a chronic process allows it to achieve a persistent weakening of the manifestations of pancreatitis. Duspatalin relieves only pathologically increased motility, without reducing normal one, and does not cause one of the common complications when using antispasmodic therapy - intestinal atony.
Other drugs used for pathologies of the pancreas, which are accompanied by spasm of smooth muscle cells: Niaspam, Sparex. Effective products based on mebeverine, but less expensive than Duspatalin. Riabal (prifinium bromide). An antispasmodic in the form of a syrup, which is used in pediatrics for infants from 3 months of age. Eliminates pain due to inflammation of the gland, intestinal spasms (colic), and bloating in infants.
Dicetel (pinaverine bromide). Halidor (in tablets and injections). Buskopan. It is one of the effective means for relieving spastic pain in chronic pancreatitis. Prevents the development of an acute attack, relaxes the sphincter and eliminates stagnation of bile and pancreatic juice. At the same time, it eliminates pain from spasms of smooth muscles of all organs of the gastrointestinal tract, nausea, bloating, and diarrhea.
Spasmoanalgesic Spazmalgon (in tablets and injections).
Thanks to the interaction of three active components, it has a pronounced therapeutic effect for pancreatitis. Spazmalgon contains two types of antispasmodics (fenpiverinium bromide, pitofenone) and the analgesic metamizole sodium (analgin), which enhance each other’s effects. It is used in tablets for moderate spastic pain. When injected, it has a stronger effect for acute pain. Additionally acts as an anti-inflammatory and antipyretic agent.
Other combination drugs: Bral, Revalgin (in injections), Spazgan (in tablets and injections), Maxigan, Spazmalin.
Alkaloid Atropine
This drug is an anticholinergic plant alkaloid. It is used mainly in combination with painkillers. Atropine introduced into the body blocks M-cholinergic receptors, reduces pancreatic secretion, and also reduces the tone of smooth muscle organs.
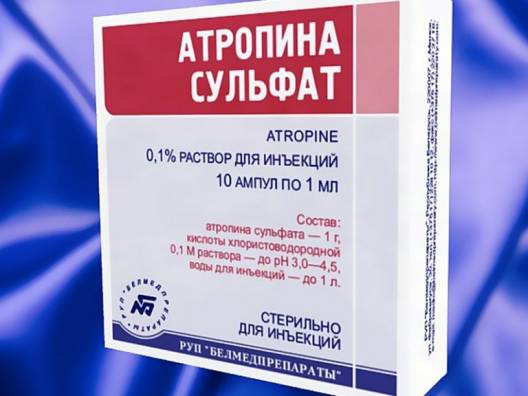
Available in tablet form, 1% solution. There is also 1% ointment and eye drops. The drug must be used under medical supervision, as it has a number of serious side effects and contraindications.
Atropine is contraindicated in persons who have:
- hypersensitivity to the main substance;
- with closed-angle and open-angle glaucoma.
It is prohibited for children under 7 years of age and patients with cerebral palsy to take it. With caution - with Down syndrome, esophageal achalasia, coronary heart disease, arterial hypertension.
- headache and dizziness;
- bowel dysfunction;
- increased eye pressure;
- dry mouth;
- tachycardia;
- difficulty breathing;
- photophobia.
If there are signs of side effects, you should immediately consult your doctor.
Antispasmodic Niaspam
Another myotropic antispasmodic is Niaspam. Like other drugs, it affects smooth muscle fibers and does not have an anticholinergic effect. The main substance is mebeverine, available in the form of capsules in a dosage of 200 mg.

Important: in pharmacies the drug is dispensed with a doctor’s prescription. This antispasmodic agent has a number of serious side effects, such as:
- Quincke's edema;
- hives;
- exanthema;
- itching and redness of the skin;
- swelling of the face.
These signs are very dangerous for human health, so before taking the drug it is necessary to take tests and undergo a full examination of the body in order to prevent their occurrence.
The drug is contraindicated for children under 12 years of age, with individual intolerance to the main substance; it is prescribed with caution to pregnant women and women during breastfeeding.

Duspatalin
The drug is used to relieve pain in chronic pancreatitis. In most cases, chronic pancreatitis with periodic relapses is the result of dysfunction of the sphincter of Oddi. Duspatalin affects this smooth muscle, relieves obstruction and alleviates the condition. Available in the form of capsules at a dose of 200 mg and tablets at a dose of 135 mg. This medicine has few contraindications:
- hypersensitivity to components;
- allergic reactions;
- children's age up to 12 years.
Special warning: the drug affects the ability to drive.
Duspatalin is considered a medicine that causes virtually no side effects, but some manifestations may occur in the form of:
- stool disorders;
- headache;
- itching;
- hives;
- swelling of the face;
- nausea and vomiting.
Note that Duspatalin cannot be combined with alcohol, since the latter has an irritating effect on the gastrointestinal tract and increases spasms. In this regard, the drug may not have the desired effect or may be completely useless.
The use of antispasmodics is necessary in the complex treatment of pancreatitis to alleviate the patient’s condition. But it is necessary to prescribe these drugs taking into account the full clinical picture of the disease, the individual characteristics of the body, and the occurrence of unwanted side reactions. And most importantly: in order not to harm your own body, you should not self-medicate and purchase antispasmodics without a doctor’s prescription.