The pancreas is a parenchymal organ of mixed secretion that performs the following functions:
- production of digestive juice necessary for digesting food,
- the formation of hormones that affect the functioning of body cells (insulin, glucagon, somatostatin).
When the pancreas malfunctions, a dangerous disease occurs - pancreatitis, the prognosis of which depends on certain factors. Statistically, it affects adult men more often than women, and it can shorten a person's life expectancy.
Types of pancreatitis
There are 2 types of illness:
- spicy,
- chronic.
Acute pancreatitis occurs for the first time. The inflammatory process lasts a short time and affects parenchyma cells, which as a result are damaged by activated enzymes.
The following types of acute form are distinguished:
- interstitial,
- hemorrhagic,
- purulent,
- pancreatic necrosis.
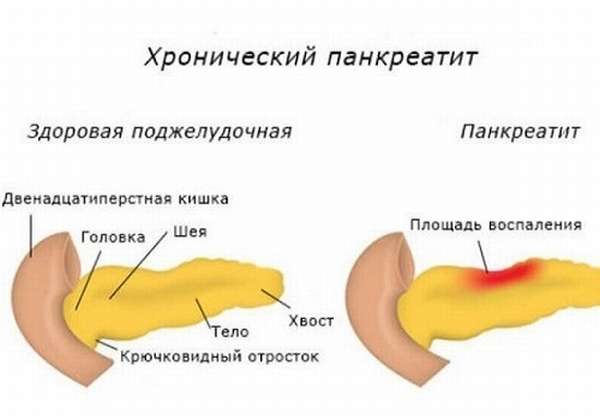
Chronic pancreatitis occurs after repeated repetitions of the acute form of the disease, but with initial changes there are often no symptoms. Pancreatitis bothers patients for quite a long time, as a result of which the parenchymal tissue is replaced by scars and its surface becomes damaged.
The following chronic forms are distinguished:
- alcoholic,
- biliary,
- toxic,
- infectious,
- ischemic,
- idiopathic.
Chronic stage
Variants of the course of chronic pancreatitis:
- Edematous-interstitial (subacute).
- Fibrous-sclerotic (indurative).
- Pseudotumorous, with an increase in the size of the pancreas.
- Parenchymatous, with inflammation of the glandular tissue - parenchyma.
- Cystic, with the formation of cysts up to 15 mm in diameter.
Classification of pancreatitis.
The following stages of disease development are distinguished:
- initial stage - lasts the first 1-5 years;
- a detailed picture of the disease with clinical signs - occurs after 5-10 years;
- the last stage, with the development of complications, appears 10-15 years from the onset of the disease.
According to the clinical manifestation, chronic pancreatitis occurs latently (painlessly) or has a recurrent course.
What affects life expectancy with pancreatitis?
People who are far from medicine often do not know what determines the life expectancy of a person with a history of pancreatitis.
The most significant reasons are:
- The course of the pathology. In the acute form, the likelihood of death is higher than in the chronic form.
- The severity of the condition. The more severe the disease, the greater the risk that it will develop fatally.
- Presence of complications. If tissue necrosis occurs, death occurs in 50% of cases. Internal organs cannot cope with the effects of toxins, and heart and kidney failure develops. Sometimes bleeding occurs, which also causes death.
- Concomitant diseases: diabetes mellitus, malignant tumors, pathology of the gallbladder and duodenum, helminthiasis (in a child). Against the background of severe disorders in the body, the risk of death increases.
- Age. Most often, deaths occur in patients over 70 years of age.
- Timeliness of receipt and quality of medical care. The sooner a doctor begins to treat a patient with pancreatitis, prescribing adequate therapy, the greater the chance of a favorable outcome.
- Impeccable adherence to doctor's prescriptions and diet. When a person takes responsibility for his own health and takes prescribed pills, the survival rate in such cases reaches 80%. If he ignores medical recommendations and does not take medicine, the indicator decreases by 2 times.
- Quitting alcohol. Eliminating a bad habit leads to a reduction in damaging effects.
Features of diagnosing pancreatitis in older people
Pancreatitis in older people can only be detected by a gastroenterologist. However, it is almost impossible to give an accurate forecast of what kind of disease it is based on external signs. The examination begins with general and biochemical blood tests, as well as urine and stool tests. Pancreatitis is characterized by a lack of protein, which can be determined by the results of a biochemical blood test, and an increased level of fat found in the stool.
Ultrasound plays an important role in the diagnosis of pancreatitis. Using it, you can determine how uneven the organ’s shares are, detect the presence of stones, cysts, seals, as well as dilation of the duct. When pancreatitis is detected and a diagnosis is made, it is necessary to treat the disease.
Read material on the topic: Folk remedies for the elderly: healthy recipes
How long do people live with chronic pancreatitis?
Life expectancy is often reduced by 10–20 years. This is due to the fact that when the gland is not working, the body cannot cope with the additional load. What are the prognosis for treating the disease?
According to statistics, with the acute form and severe course of the disease, death occurs in 30% of cases. In 15% of people, recovery occurs, and the remainder will experience a re-exacerbation of the pathology (relapse). A patient with a chronic form and mild course with adequate therapy can live as long as a healthy person.
According to the observations of European specialists, the survival rate of people during the first 10 years of the disease is 70%, 20 years - 45%. If complications arise or surgical intervention is necessary, it is reduced. If a malignant tumor develops in the affected organ, the prognosis is proportionally reduced by 4% over 20 years, provided that the treatment is carried out correctly.
If the patient leads a healthy lifestyle and refuses to drink alcohol, then he will live the first 10 years in 80% of cases. When a person ignores all medical recommendations, does not follow a diet and does not get rid of bad habits, the average life expectancy is reduced by 2 times.
How does pancreatitis manifest in older people?
Elderly people experience acute pancreatitis if, first of all, they feel pain, which varies in intensity and can occur in any part of the abdominal cavity. Sometimes it can be so strong that it even causes painful shock. The pain is of a girdling or constricting nature; tingling may occur in the kidneys or liver, and this occurs either in periodic attacks or constantly over a period of time. The following symptoms may indicate pancreatitis in older people:
- Periodic vomiting in small quantities, which may be accompanied by the release of bile or blood.
- Intestinal paresis, which is characterized by severe pain, softness of the abdomen and lack of tension in the muscles. With such indicators it is quite difficult to make a diagnosis.
- Coated tongue.
- Human skin is pale and bluish in color.
- The whites of the eyes become yellow.
- Rapid pulse, low blood pressure.
- Poisoning with toxic substances.
- Body temperature rises, but in the case of a weakened body it can remain within normal limits.
- Increased body temperature, but in weakened patients it may remain normal.
- Voskresensky syndrome is the absence of a pulse in the abdominal aorta.
Cause of mortality in pancreatitis
The disease is characterized by severity and a high risk of death. Why this condition is dangerous and why the patient dies, we will consider further.
Pancreatic necrosis
Pancreatic necrosis is a complication in which the death of parts or the entire pancreas occurs. The main reason for this condition is damage to the organ by its own enzymes and the occurrence of inflammatory processes. Provoking factors are considered to be alcohol abuse, calculous cholecystitis, abdominal trauma and previous surgical interventions.
Pancreatic necrosis has a far from high survival rate: in 40–70% of cases death occurs. If assistance is not provided in a timely manner, the indicator increases significantly.
Pancreas cancer
It is characterized by an aggressive course and rapid spread throughout the body. In most cases it leads to death. If cancer is detected at an operable stage, surgery is performed to completely remove the organ or its diseased part. The most common causes of cancer are: smoking, poor diet, excessive alcohol intake, impaired digestive function, and genetic factors.
Mortality after surgery
Pancreatic surgery is difficult and has high mortality rates. Removing an organ is associated with difficulties, since it is located in proximity to large vessels, kidneys, and shares blood flow with the duodenum. Highly active enzymes often digest parenchymal tissue, and it is quite difficult to suture it.

The patient has to remain in bed, spending a lot of time lying down. All this threatens the development of complications in the postoperative period, which increases the risk of death. If the operation is successful, the patient faces a long road to recovery.
Diagnostics
It is a very difficult matter, but when stones are visible in the projection of the pancreas during an X-ray of the abdominal cavity, this is considered sufficient to make a diagnosis. But ultrasound is not used to detect chronic pancreatitis because it is not informative; the gland is not visible at all.
CT helps to make a diagnosis and monitor changes in the pancreas, but MRI is much worse in quality.
Endosonography is the same sensitivity as CT - a combination of endoscopy and ultrasound, plus you can immediately take a puncture from the gland. If the instrumental examination is uncertain, functional tests can be performed that indirectly assess the working capabilities of the organ in the later stages, when secretory insufficiency has flourished, but their information content leaves much to be desired.
How to extend lifespan?
Despite the danger of the pathology, there are ways to improve the approximate prognosis and give the patient additional years of life.
Prevention and lifestyle
In addition to taking medications that the treating doctor indicates in the medical history, you need to adhere to rules that prevent the progression of the disease and the risk of complications. By following these recommendations, the patient will live much longer.
It is necessary to pay attention not only to physical health, but also to psychological health. Experts advise people with pathology to change their lifestyle, avoid nervous strain and undergo timely medical examinations.
Despite the positive reviews about the use of traditional medicine, it is still worth consulting with your doctor first to avoid complications.
It is recommended to adhere to the following rules:
- completely eliminate alcohol, cigarettes and drugs,
- moderate exercise,
- the daily routine should include a full night's sleep,
- developing a positive attitude and resistance to stress.
Diet
Patients at home can cope with pain and nausea by reducing the load on the digestive system:
- Excluding fatty, fried and spicy foods from the menu. Preference should be given to boiled, baked or stewed foods.
- Frequently eating small meals. It is advisable to eat at least 6 times a day, and the volume of one serving should not exceed 250 g. The break between meals is 2.5–3 hours.
- The daily amount of carbohydrates should not exceed 300 g, and fats - 70 g. They have an extremely harmful effect on the pancreas.
- Carrying out processing of products. To reduce the severity of the inflammatory process, doctors advise eating foods cut into pieces, chewing them thoroughly, or pureed.
- The diet is selected so that it has a high protein content. The substance must be added to the diet up to 150 g per day.
- Maintain drinking norms. People need to consume about 2 liters of water. Doctors recommend taking a few sips every half hour.

There is a list of prohibited foods, due to which pancreatic juice begins to be produced intensively. It is highly undesirable to eat the following foods:
- meat and fish of fatty varieties,
- canned food,
- sausages,
- high fat dairy products,
- caviar,
- sauces, including mayonnaise, ketchup,
- legumes,
- vegetables - tomatoes, sorrel, cabbage and radishes,
- sour fruits,
- cereal products – millet, corn and barley,
- confectionery.
Sample menu for the week
You need to come out of fasting for the first few days after an attack gradually: on the 3-4th day you can eat some crackers from uneaten bread or a loaf, add jelly, fruit drink, cranberry or currant juice diluted with water to clean water.
If the condition is stable, there is no deterioration in health, then the diet is supplemented with liquid ground porridge (semolina, buckwheat, oatmeal, rice), liquid mashed potatoes, dry bread or biscuits.

You need to come out of fasting in the first few days after an attack gradually: on the 3-4th day you can eat some crackers from uneaten bread or a loaf.
To facilitate the selection of foods allowed after an attack of pancreatitis, below is a sample menu for the week. It will help you understand the principle of the diet, which must be followed for at least several months after an acute attack, so as not to provoke a relapse of inflammation.
Monday
- breakfast: crackers, mineral water without gas;
- lunch: a handful of raisins, baked apple;
- lunch: pureed vegetable soup, chicken meatballs;
- dinner: rice, cottage cheese, tea or rosehip decoction.
Tuesday
- breakfast: low-fat milk or cottage cheese, crackers;
- lunch: beet salad, boiled meat;
- lunch: steamed omelette, bread, jelly;
- dinner: meatloaf, steamed vegetables, jelly.
Wednesday
- breakfast: yogurt, oatmeal;
- lunch: steamed cutlets, pumpkin puree;
- lunch: vegetable broth with lean fish or boiled veal, crackers;
- dinner: thin rice porridge, tea or jelly with dry cookies.
Thursday
- breakfast: porridge with low-fat milk, egg white omelette, weak tea;
- lunch: low-fat yogurt, kefir or cottage cheese;
- lunch: vegetable soup, cottage cheese casserole;
- dinner: boiled or steamed chicken meat, oatmeal, tea or rosehip decoction.

Mashed potatoes are an optimal side dish for pancreatic problems.
Friday
- breakfast: semolina porridge with water, apple, tea with 1 tsp. honey;
- lunch: steamed diet cutlets, broccoli puree;
- lunch: vegetable soup with meatballs (possibly with potatoes);
- dinner: rice porridge, tea.
Saturday
- breakfast: oatmeal, cottage cheese, mineral water;
- lunch: steamed omelette, baked apple;
- lunch: vegetable soup (can be pureed), boiled fish fillet;
- dinner: beet salad, mashed potatoes, kefir.

Snacks in the form of yogurt, yogurt or kefir are acceptable.
Sunday
- breakfast: steamed stuffed peppers, yogurt, bread;
- lunch: boiled meat with vegetables, tea;
- lunch: rice porridge, steamed cutlets;
- dinner: fish meatballs, boiled carrot or pumpkin puree, baked apple.
During breaks, snacks in the form of raisins, baked apples, yogurt, yogurt, etc. are permissible, so as not to irritate the stomach and glands with a feeling of hunger and excess gastric juice - this can provoke a repeat attack.

The amount of liquid is not limited: thirst can be quenched not only with water and tea, but also with various berry fruit drinks, decoctions, juices (preferably diluted with water), as well as warm water with honey.
The amount of liquid is not limited: thirst can be quenched not only with water and tea, but also with various berry fruit drinks, decoctions, juices (preferably diluted with water), as well as warm water with honey.










