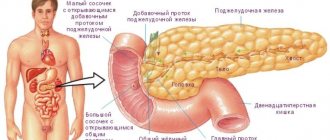
Not many people know the signs of pancreatic inflammation in adults. This gland is an important internal organ. It produces pancreatic juice, which helps digest food.
Pancreatitis in adults most often develops against the background of poor nutrition and alcohol abuse. If treatment is not started, inflammation of the pancreas can lead to serious consequences, including death. What are the etiology, clinical picture and treatment of this disease?
Causes of the disease
Almost always, the disease appears due to excessive consumption of alcoholic beverages and gallbladder diseases. Often the disease is a consequence of the appearance of calcifications in the gallbladder. There are other reasons that can cause the development of this serious disease.
These include:
- various ailments of the duodenum. (In many cases, the disease develops with ulcers and duodenitis);
- surgical operations on gastric tissues, the gland in question;
- injuries, wounds in the abdominal area;
- cholangiopancreatography;
- exposure to certain medications (antibiotics, drugs containing large amounts of estrogen, etc.);
- hepatitis B or C, epidemic infectious diseases;
- infection with helminths (roundworms);
- tumors and abnormal development of the canals of the said gland;
- incorrect metabolic processes;
- disruption of hormone levels;
- cardiovascular diseases;
- heredity.
It is noteworthy that the true source of the development of pancreatitis can be detected in only 30% of patients. Correction of the disease should always be carried out under the supervision of a doctor. If a person develops symptoms of pancreatitis and treatment at home can only harm the patient and lead to serious complications.
Diagnosis of the disease
At the initial stage, acute pancreatitis sometimes cannot be recognized even by an experienced doctor. Therefore, in diagnosing this disease, the gastroenterologist takes into account the data from the following studies:
- General blood analysis. It allows us to draw a conclusion about the presence of inflammation in the body.
- Blood chemistry.
- Cholangiopancreatography.
- CT scan.
- Blood sugar test shows elevated glucose levels.
- Analysis of urine.
- Ultrasound of the abdominal organs.
- Stool analysis.
- Gastroscopy - to assess damage to the stomach, etc.
Diagnosis of pancreatitis begins at the stage of patient's treatment by palpation
Symptoms of pancreatitis
The main symptom of acute pancreatitis is acute cutting pain in the abdominal cavity. Constantly changing localization of pain is typical for patients diagnosed with pancreatitis: symptoms depend on the site of inflammation of the pancreas. If there is an inflammatory process in the head of the pancreas, the pain will appear in the right hypochondrium, if in the body of the pancreas, the pain will be in the epigastric region, if the tail - in the left hypochondrium. Acute pain of a girdle nature, although less common, still occurs if a person has acute pancreatitis - these symptoms indicate inflammation of the entire pancreas. Pain behind the sternum and left shoulder blade should also be regarded as signs of pancreatitis.
Symptoms of pancreatitis in adults most often bring patients to the surgical hospital. Most likely, first aid for pancreatitis will be provided to you by ambulance staff - few people can withstand acute attacks. This is understandable - if you have unbearable pain in the pit of the stomach, radiating to the left hypochondrium or encircling and squeezing the upper half of the body, which lasts for hours and is accompanied by vomiting, then it will be difficult to withstand such a test and you will have to resort to the help of doctors.
Severe acute pain, shock or collapse are clear signs of pancreatitis in adults. These pains during pancreatitis torment a person for hours, exhaust him, and the fear of death is mixed in with them as an unpleasant psychological factor.
As a rule, they are localized in the area under the pit of the stomach and radiate to the costal arch, shoulder, and kidney on the left. They can compress the torso around the circumference, spreading to the other side of the chest, into the shoulder. This can confuse and confuse the patient and his relatives, who begin to suspect renal or biliary colic, myocardial infarction, or angina. Often, only a doctor can determine the signs of acute pancreatitis and distinguish them from a heart attack and other diseases after an instrumental examination.
Diagnosis of pancreatitis is carried out using ultrasound. The device shows an increase in the size of the pancreas, a significant change in the shape of its head, characteristic of acute pancreatitis.
Symptoms of chronic pancreatitis in adults appear against the background of vomiting that does not bring relief. Diarrhea with pancreatitis is also a common occurrence, it leads to dehydration. This causes a person’s facial features to become sharper, and the skin becomes unusually dry. Constipation, hardening of the abdominal muscles, and bloating also foreshadow an attack of pancreatitis - the symptoms are very contradictory.
An attack of pancreatitis is accompanied by high blood pressure, palpitations, and shortness of breath. Subsequently, the pressure, on the contrary, can drop significantly. In addition, a urine test may reveal kidney failure and jaundice. On the lower back and around the navel, bluish spots appear, which give the skin a marbled tint. In the groin areas, these spots may have a greenish-blue tint. They appear due to the penetration of blood from the inflamed pancreas under the skin of the abdomen. It should be remembered that the patient is getting worse every minute, so you should not delay calling an ambulance. Doctors know how to relieve an attack of pancreatitis.
You should not be afraid of hospitalization - patients are not always operated on. But even one stay in the hospital is enough to be under the close attention of surgeons for the rest of your life.
Possible complications
Both acute and chronic inflammation of the pancreas can lead to complications in the absence of proper therapy. Acute pancreatitis is dangerous due to the following complications:
- inflammation of the peritoneum (peritonitis);
- shock;
- sepsis;
- formation of an abdominal abscess;
- fistula formation;
- total necrosis of the gland;
- impaired liver and kidney function;
- bleeding;
- acute thrombosis;
- DIC syndrome;
- inflammation of the pleura;
- pneumonia.
All complications can be divided into early and late.
The latter develop 2-3 weeks after the appearance of the first symptoms of the disease.
Chronic pancreatitis is also very dangerous.
Its consequences can be compression of the duodenum, the development of jaundice, the formation of cysts and pseudocysts, bleeding, diabetes mellitus, gland cancer, portal hypertension, anemia, ascites.
Treatment of pancreatitis
If the first signs of pancreatitis in adults have been confirmed by examination results, then it is necessary to begin treatment immediately.
Acute pancreatitis
If an adult experiences acute symptoms of pancreatitis, he or she urgently needs to be taken to the hospital and treated only in a hospital setting. And before the ambulance arrives, you can apply a cold heating pad to your stomach and take antispasmodics (papaverine, drotaverine).
During the treatment of acute pancreatitis, special attention is always paid to hunger, cold and rest. In a hospital setting, the following drugs are usually used:
- Plasma substitutes and saline solutions (reopolyglucin, reosorbilact) are administered intravenously;
- diuretics to prevent swelling of the pancreas (furosemide, Lasix, Diacarb);
- to relieve pain - antispasmodics and painkillers (no-spa, papaverine, ketanov, dexalgin);
- with persistent vomiting (cerucal, metoclopramide);
- in the acute period, enzymatic inhibitors are used (contriven, trasylol);
- antisecretory drugs (quamatel, omeprazole);
- vitamin therapy to maintain a weakened body.
The patient is advised to fast for 4-5 days. If the course of the disease is particularly severe and you have to fast for more than 14 days, then parenteral nutrition is prescribed. The patient is administered intravenously protein hydrolysates and fat emulsions. Gradually, yogurt and cottage cheese appear in the patient’s diet, and after another 3 days you can switch to diet - table No. 5P.
In some cases, if destructive pancreatitis is suspected and conservative therapy is ineffective, surgical intervention is indicated.
Chronic pancreatitis
The symptoms of chronic pancreatitis in adults and treatment are almost identical, as in the case of the acute course of the disease. Following a diet for such a patient should become a lifestyle. He must also take enzyme preparations and periodically antispasmodics. In addition, it would be good to visit resorts specialized in the treatment of gastroenterological diseases.
A diet for pancreatitis may seem very strict, since it excludes from the diet the most beloved foods by many (chocolate, sweets, barbecue, mushrooms, fried, spicy, fast food). Food processing methods that should be a priority are boiled or stewed. You need to eat small and often, and also do not mix different types of proteins, fats and carbohydrates.
Traditional methods of treatment have also proven themselves well in the treatment of chronic pancreatitis. Herbal infusions (with chamomile, calendula, dandelion roots, corn silk, plantain, mint) are used to prepare infusions or decoctions. Taken, as a rule, 30 minutes before meals or 1 hour after meals.
Regardless of how pancreatitis manifests itself in adults, it is necessary to combine various treatment methods in such a way as to maintain the functioning of the pancreas and avoid relapses and exacerbations. A healthy lifestyle and timely recognition of the symptoms of the disease will help in the fight against this disease.
Waiting for an ambulance
If the attack is taken by surprise, many cannot immediately figure out what to do in case of acute pancreatitis at home. No one except specialists can help the patient, so you can’t hesitate. The only correct solution is to call an ambulance.
It should be remembered that it is not recommended to relieve pain on your own in this situation by taking any medications.
To alleviate a person’s painful condition while there is no qualified help, you can perform a number of measures that will help reduce pain and not aggravate the situation:
- promptly call a doctor;
- eat nothing;
- give water to drink no more often than every 30-40 minutes and little by little;
- Avoid taking any medications;
- make sure that the patient does not make sudden movements;
- You can apply a cold compress to the sore spot.
When the disease worsens, you should try to provide the patient with complete rest.
Attention! The most comfortable position for the patient is a sitting position.
In this case, the torso must be tilted forward. If the patient has bouts of vomiting, this condition can be alleviated a little by applying auxiliary pressure with your fingers on the root of the tongue. To reduce pain, you should breathe shallowly and hold your breath. This will help you calm down and restore your breathing.

Sitting position is the most comfortable position for pancreatitis
Traditional methods of treating pancreatitis
In order not to learn from your own experience what pancreatitis is, you should take care of yourself, take care of your nerves, eat moderately and not abuse alcohol, and monitor proper and nutritious nutrition. Do not panic if you are still bothered by unpleasant symptoms and think that you have pancreatitis - treatment with folk remedies has proven itself since ancient times. Herbal treatment of pancreatitis will help you without the use of harmful drugs.
- Prepare a mixture of herbs: 3 parts mint leaves and dill seeds, 2 parts immortelle flowers and hawthorn berries, 1 part chamomile flowers. At 5 gr. Add a glass of boiling water to the mixture and keep the infusion in a water bath for half an hour. After this, the brewed mixture is infused for an hour. Drink 50 ml 3 times a day. strained liquid. Hypertensive patients should use this decoction with caution due to the presence of hawthorn in it;
- A mixture of mint leaves, elecampane grass, and string grass, taken in equal parts, helps well. For 1 ½ cups of boiling water, take 3 tablespoons, brew the tea for 4 minutes in a container covered with a lid. Take 100 grams of infusion in the morning and evening before meals;
- Calendula infusion is prepared in the following way: 1 tablespoon of flowers is poured with one glass of boiling water and wrapped for 8 hours. The herbal infusion is filtered and taken half an hour before meals, 100 g;
- An infusion of immortelle flowers, motherwort, and St. John's wort, taken in equal parts, will help soothe severe pain. For ½ liter of boiling water you will need 2 tablespoons of the mixture. The infusion should stand for at least an hour, then it is filtered and taken in 50 g doses. before each meal;
- Try herbs for pancreatitis. 3 tablespoons of the collection of coltsfoot leaves, elecampane herb, succession herb in a ratio of 1:1:2, pour ½ liter of water, boil for 4 minutes, leave in a covered container for 2 hours. Drink the warm infusion in small sips before meals;
- Potato juice helps with pancreatitis in combination with carrot juice. There is such a method: thoroughly wash one or two carrots and 2 - 3 large potato tubers. Carefully remove the eyes from the potatoes, being careful not to damage the skin. You need to squeeze juice out of these vegetables, which is drunk 30 minutes before meals for a week, then 7 days of rest, and again a course of juice therapy. In total, you need about three courses - depending on how you feel;
- It is useful to drink sauerkraut juice before meals. It contains a specific substance necessary for the production of pancreatic juice;
- Buckwheat with kefir will cleanse the body well for pancreatitis. Pour boiled buckwheat with kefir in the evening. In the morning, drink half of the porridge instead of breakfast, and for dinner - the second half (certainly 2 hours before bedtime). And so on for 10 days. Then take a break for 10 days and repeat the course. During the pause, eat 5-10 apricot kernels 3 times a day;
- Pass 6 lemons with peel through a meat grinder, after removing the seeds, then add 300 grams each. chopped garlic and parsley, stir, place in an enamel pan. Take 1 teaspoon 3 times a day ¼ hour before meals.
Causes of pancreatic pathology
The cause of the development of pancreatitis is the retention of pancreatic juice in the gland and disruption of its outflow. An acute attack most often develops due to alcohol consumption and blocking the release of enzymes due to stones (cholelithiasis).
The causes of acute pancreatitis can be divided into 3 groups:
- Blockage of the duct and resulting delay of enzymes in the gland. This can occur due to stones, tumors and pathologies of nearby tissues.
- Increased production of enzymes, exceeding the required amount.
- Bile reflux into the pancreatic duct.
Various life factors in children and adults lead to the development of these causes.
In adults
Frequent causes of the development of the acute form and exacerbations of the chronic form are:
- nutritional errors - overeating, infatuation with fatty, spicy foods, irregular meals;
- use of certain medications;
- abdominal injuries, including complications after surgery;
- stones in the bile ducts;
- endocrine diseases (diabetes mellitus) and vascular pathologies with impaired blood supply to the pancreas;
- consequences of viral infection;
- oncological pathologies, renal failure.
A common cause of the development of the disease in men is alcohol abuse in combination with heavy fatty foods. There is even a term “alcoholic pancreatitis”. The disease often affects bachelors who eat processed foods and sandwiches.
Additional factors that provoke the disease in women are a love of dieting and fasting. An unbalanced diet creates additional stress on the organ. Hormonal disorders, pregnancy, and use of contraceptives also lead to the development of the disease.
Data on the incidence of pancreatitis vary depending on the area and climate. This is due to food traditions, the population’s tendency to drink alcohol and different gastronomic preferences.
Video about the causes and symptoms of pancreatitis:
In children
The underdeveloped immune system in children means that they are often susceptible to acute forms of disease.
Pancreatitis can be caused in a child by:
- irregularity in eating, long breaks between meals;
- parasites (in particular, worms);
- allergic reactions to products;
- cystic fibrosis is a congenital pathology;
- eating food inappropriate for age, spicy, salty, fast food;
- fatigue and increased physical activity, for older children, after school classes in clubs, sections, and electives;
- abdominal injuries.
Pathology can develop as a result of a complicated viral or bacterial infection (chickenpox, herpes, mumps), as well as other problems of the gastrointestinal tract. Dysbacteriosis often leads to the development of a chronic form in children.
Video from Dr. Komarovsky:
Therapeutic nutrition for pancreatitis
When treating pancreatitis, you should pay attention to the following nutritional principles:
- meals should be frequent - approximately every 3-4 hours;
- food should not be plentiful;
- to avoid mechanical irritation of the gastric mucosa, products should be consumed in pureed form;
- it is necessary to increase the consumption of foods containing proteins (fish, meat, cottage cheese) to 140-160 g;
- you need to reduce the consumption of foods containing carbohydrates (sugar, honey) to 300-350 g;
- it is necessary to reduce the consumption of foods containing fats to 70~80 g;
- the diet should not include products that have an increased juice-containing effect (cabbage broth, fish and meat broths);
- if severe pain occurs, it is necessary to follow therapeutic fasting, but no more than 1-2 days.
Products that can be consumed in the treatment of pancreatitis:
- bread and bakery products (grade I and II wheat bread, dried, crackers);
- soups (vegetable, chicken, cereal, vermicelli);
- dishes from lean meats (chicken, beef, veal) - cutlets, soufflé, meatballs, rolls, mashed potatoes);
- fish dishes (low-fat fish, boiled, steamed, in pieces);
- eggs (omelet);
- milk and dairy products (cottage cheese, milk, kefir, cheese);
- fats (unsalted butter, olive, refined sunflower);
- vegetable dishes (from carrots, potatoes, pumpkin, beets, zucchini - mashed, boiled);
- cereals and pasta (pasta, noodles, oatmeal, semolina, buckwheat, pearl barley, boiled rice, porridge);
- fruits (unsweetened, baked apples, pears);
- sweet dishes (compotes, jellies, jelly);
- drinks (weak tea, rosehip and wheat bran decoction).
Foods that should be excluded from the diet when treating pancreatitis:
- soups (cabbage, millet, strong meat, mushroom and fish broths);
- dishes made from fatty meats, fried;
- fried fatty fish dishes;
- beef and lamb fat;
- vegetables and greens (radish, cabbage, turnip, radish, rutabaga, sorrel, spinach);
- smoked meats, sausages and canned food;
- spicy dishes;
- bread and bakery products (rye bread, butter dough);
- ice cream;
- alcoholic drinks.
Prevention measures
To avoid the development of pancreatitis, it is necessary to follow the rules of prevention:
- give up alcohol;
- adhere to proper nutrition, do not overload the organ;
- do not overeat;
- eat more vegetables, fruits, and fiber-rich foods;
- maintain normal weight;
- promptly treat infectious processes in the body (sinusitis, otitis media, cholecystitis);
- limit the intake of medications that negatively affect the gland, take medications strictly as recommended by your doctor.
Learn more about how to prevent the development of acute pancreatitis of the pancreas after watching the following video:
Gymnastics for pancreatitis
It is recommended to perform breathing exercises, which have the effect of massaging the internal organs. Perform the exercises 2-3 times a day - lying, sitting or standing. Start with 3-4 repetitions, gradually increasing to 9 times. Gymnastics are performed after an attack of pancreatitis subsides.
Inhale, exhale and hold your breath. Smoothly, but quite strongly drawing in your stomach, count to three, and then relax your abdominal muscles
Inhale, exhale and hold your breath. During the breathing pause, “inflate” your stomach as much as possible and count to three. As you exhale, relax.
Halfway through the inhalation, hold your breath for 1-2 seconds and continue inhaling further, as if directing the air into the stomach and protruding the abdominal wall. Having inflated your stomach, hold your breath at the end of the inhalation. Count to three. Then begin to slowly draw in your abdominal wall, continuing to count to six. Exhale and relax your abdominal muscles.
Draw your stomach in as you exhale. Hold your breath for a few seconds and relax your abdominal muscles. Actively inflate your stomach as you inhale and draw it in again as you exhale.
Types and classification of the disease
Pancreatitis is divided into types due to its occurrence:
- Primary occurs due to damage to pancreatic tissue. It is caused by dietary errors, toxic poisoning from medications and foods. The cause may be genetic predisposition and congenital diseases. Inflammation can appear at any age. Timely diagnosis and adequate therapy can return organ tissue to normal.
- The secondary (reactive) form is determined if inflammation has developed due to other diseases. The cause may be cholelithiasis (GSD), viral infections, parasitic lesions of the biliary tract, and cardiovascular diseases. The success of treating pancreatitis in this case depends on identifying and eliminating the causes, that is, the primary disease. Often these reasons cannot be identified and eliminated.
Often the cause of inflammation is gastritis and biliary dyskinesia.

Pancreatitis has acute and chronic forms.
The acute form is characterized by a rapid onset of inflammation and a sharp increase in symptoms. Pancreatic juice, stagnating in the pancreas, begins to destroy its cells. The body of the gland increases in size due to edema. The acute form is more common in people aged 30 to 60 years and children.
The chronic form of the disease occurs in the form of periods of exacerbation and attenuation of symptoms. The initial stage usually does not have any sharp deterioration in the condition. At this time, the pancreas tissues lose their functions and are replaced by connective tissue. Enzymes and hormones are produced in smaller quantities and can no longer ensure full digestion and metabolic processes.
If the diet is violated or stress, an exacerbation begins. With significant tissue changes, constant symptoms of pancreatic dysfunction are observed.