Pancreatitis Pancreatitis. Symptoms and Causes is inflammation of the pancreas. The disease is not that common: up to 100 cases The problem of acute pancreatitis in the Krasnoyarsk Territory for every 100 thousand population.
Nevertheless, in Russia, acute pancreatitis has long been the first Acute pancreatitis E-01-01-004-2.0-2019 in the list of causes of “acute abdomen” - that is, severe pain, because of which people are forced to call an ambulance. Today, inflammation of the pancreas has given way to acute appendicitis. However, the disease remains dangerous: approximately 3 people out of every 100 who seek help die.
Therefore, it is so important to be able to recognize pancreatic inflammation in time and not miss the possible development of complications.
Why does the pancreas hurt?
If acute pancreatitis is not treated properly, it can become chronic and lead to other diseases of the pancreas.
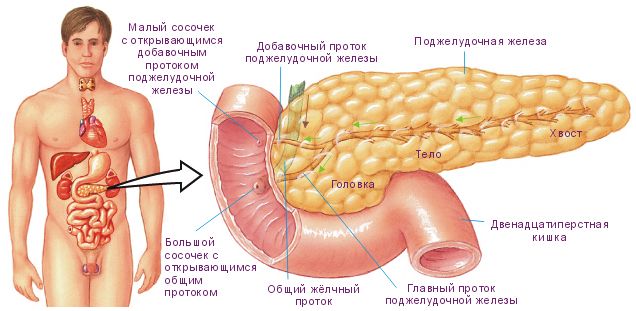
You will learn about all her other diseases in the next article. The pancreas is an important organ of the digestive system, which has a mixed function: external (exocrine) and internal (endocrine). The function of external secretion is to secrete pancreatic juice, which contains digestive enzymes necessary for the complete digestion of food.
The endocrine function is to produce the appropriate hormones and regulate metabolic processes: carbohydrate, fat and protein.
What does the pancreas do?
Main causes and mechanism of disease development
The most well-known diseases of the pancreas include acute, reactive and very common chronic pancreatitis. Also, diabetes and cancer. What causes diseases? These include:
- alcohol abuse;
- smoking;
- cholelithiasis;
- liver inflammation;
- eating fatty, fried, spicy foods;
- inflammation or blockage of the duct area by gallstones;
- endocrine diseases;
- abdominal trauma;
- duodenal diseases;
- long-term use of medications, such as antibiotics.
Main causes and mechanism of disease development
Alcohol consumption and gallbladder diseases (primarily cholelithiasis) are the causes of pancreatitis in 95-98% of cases.
Other risk factors that can trigger inflammation of the pancreas:
- diseases of the duodenum (duodenitis, peptic ulcer);
- operations on the stomach and biliary tract;
- injuries, abdominal wounds;
- endoscopic retrograde cholangiopancreatography (ERCP);
- taking certain medications (furosemide, estrogens, antibiotics, sulfonamides, etc.);
- infections (mumps (mumps), viral hepatitis B, C, etc.);
- parasitic infestations (ascariasis);
- anatomical abnormalities of the pancreatic duct (narrowing, tumors, etc.)
- metabolic disease;
- changes in hormonal levels;
- vascular diseases;
- hereditary predisposition (so-called hereditary pancreatitis).
In approximately 30% of patients, the cause of acute pancreatitis cannot be determined.
Herbs beneficial for the liver and gallbladder
Among the wide range of herbs for the treatment of the liver and pancreas, the following herbs are most often used:
- milk thistle, or milk thistle;
- tansy;
- St. John's wort, or common;
- creeping thyme (thyme);
- yarrow;
- pharmaceutical camomile;
- dandelion root;
- peppermint.
These herbs are used as a single drug to treat inflammatory processes of the liver, pancreas, and gall bladder. But it is much more effective to use herbal infusions, where each component enhances the effect of each other.
Hepatitis
Faced with a disease such as hepatitis, the patient wonders how to effectively treat the liver and pancreas. Folk remedies used in complex therapy must have hepatoprotective, anti-inflammatory, antiseptic and analgesic effects.
Such medicinal herbs include chamomile, calendula, and Rhodiola rosea root. A decoction of these medicinal plants relieves acute inflammation, eliminates bile stagnation, and helps cleanse the liver. We should also highlight the chicory plant, which is used in cooking as a coffee drink. The root of the plant has effective hepatic-restorative properties. Herbalists recommend taking a decoction or alcohol tincture of chicory root for 3 weeks.
The course of herbal treatment lasts no more than 4 weeks. If the course is shorter, the body will not be completely cleansed, and the affected liver cells will not have time to recover. If the treatment lasts more than 30 days, then there is a high risk of addiction, as a result of which the liver cells will become insensitive to the effects of natural medicines.
Biliary dyskinesia
This is a disease that is associated with impaired motility of the gallbladder, as a result of which insufficient or excessive amounts of bile enter the duodenum. For biliary dyskinesia, doctors also recommend using folk remedies for treatment. An infusion or decoction of the vegetative organs of barberry has proven itself well. To prepare the product, take 1 tablespoon of raw material per 200 ml of water, place in a water bath for 30 minutes, leave, filter and drink 100 ml 3 times a day before meals.
For dyskinesia, it is useful to drink yarrow grass, wormwood, celandine, fennel seeds, hop cones, taken in equal proportions. For 500 ml of boiling water you need to take 2 tbsp. collection, pour boiling water. After infusion and straining, drink 35 ml three times a day, 15 minutes in advance. before meals.
Cholecystitis
The inflammatory process in the gallbladder is also stopped thanks to the remedies recommended by traditional treatment. To eliminate the symptoms of inflammation, it is recommended to drink a decoction of oregano herb daily, 3-4 times a day, 50 ml.
Main causes and mechanism of disease development
Most often, actions for discomfort in the pancreas depend on the cause that led to it. Before the pain hits the area of the left hypochondrium, the person will experience a slight malaise that develops into a more intense one.
There are many diseases that can provoke this, but they all invariably lead to pancreatitis and/or exacerbation of inflammatory processes in the pancreas. The reasons that provoke this condition include:
- A malfunction in the digestive system when there is too much fat in the blood. The pancreas activates the production of enzymes that break them down in excess, which leads to pancreatitis, accompanied by high-intensity pain.
- Tobacco smoking and alcohol, excessive consumption of which provokes the constant production of gastric juice, which destroys the pancreas. Bad habits also have a negative impact on the blood supply to this organ, and any oxygen deprivation provokes inflammation.
- Pathological processes in the liver and gall bladder. They disrupt the digestion process, for example, bile can enter the pancreatic duct and activate the enzymes next to it, leading to inflammation.
- Taking a number of medications that can provoke the production of enzymes and destroy the pancreas.
- Failure in the immune system. Incorrect functioning of the protective forces can lead to inflammatory processes, due to which the tissues of this organ also suffer.
- Age-related changes, when all organs weaken and begin to fail.
- An incorrect diet, the imbalance of which leads to pancreatitis, especially if this happens constantly.
Hepatomegaly
Liver diseases are characterized by an increase in its size, when even without palpation the outlines of the organ become noticeable upon examination. One of these diseases is hepatitis. It occurs when infected with hapatitis viruses (there are currently 7 different types), as well as during prolonged exposure to alcohol, drugs, and even infection with parasites.
This is interesting: What does an enlarged liver mean? Symptoms and treatment of hepatomegaly
At first, hepatitis does not show any symptoms, but as the disease progresses more severely, a clinical picture begins that is similar to simple flu. Subsequently, the tissues are destroyed, become inflamed and become completely dysfunctional. If the disease is recognized in time and treatment is started, it is possible to achieve a complete recovery without serious consequences.
Another disease in which the liver significantly increases in size is cirrhosis. It occurs due to poor diet, excessive alcohol consumption, and long-term viral infections. The increase is due to the fact that healthy tissue is gradually replaced by fibrous tissue.
Damage to the liver by parasites (in particular Giardia), causing inflammation and severe digestive disorders.
How to recognize the disease
If you recognize alarming symptoms, pancreatic pain and other signs, consult a doctor immediately. It is unacceptable to take medications on your own, since acute pancreatitis can be confused with a heart attack, because the pain is felt under the ribs on the left side of the body and radiates to the shoulder blade.
Fever is a sign of an inflammatory process in the pancreas tissue, while chronic pancreatitis is subtle. Based on the tests, doctors will be able to make a fair diagnosis and prescribe treatment; an x-ray of the organ is also informative.
Knowing where the pancreas is located and how it hurts, you can go to the hospital in time and prevent complications. If the illness worsens, before the doctors arrive, do not eat anything, place a cold compress on your stomach and drink still mineral water, but you should not use painkillers.
Chronic pancreatitis is recognized by symptoms such as periodic nausea, vomiting with bile, loose stools with drops of fat and particles of poorly digested food. A person is also bothered by rumbling in the stomach from time to time, however, many patients do not attach much importance to these symptoms.
The acute type of the disease is accompanied by rapid heartbeat, elevated temperature, pale skin and low blood pressure. The organ located in the abdominal cavity reacts sharply to poor nutrition.
When the pancreas hurts, symptoms, treatment and diagnosis of discomfort depend on the specific disease. Thus, with cystic fibrosis, doctors notice salt crystals on the surface of the skin, the cyst is characterized by increased body temperature, and in the case of tumor formation, pale skin and the development of jaundice are noted.
Diabetes is recognized by symptoms such as extreme thirst, itchy skin, increased sweating and changes in heart rate in the absence of insulin.
Symptoms for various organ pathologies
Pain in the pancreas can also be caused by infection and bacteria entering the body. If a response to such a situation is not timely, harmful microorganisms cause a change in the structure of the organ.
Due to the structure and shape of the pancreas, pain in it can easily be confused with other pathologies in other organs:
- the inflamed head localizes discomfort on the right side, which gives suspicion to the liver;
- problems in the body and tail give unpleasant sensations in the left hypochondrium;
- and acute pancreatitis provokes girdling pain of high intensity.
Important! Similar sensations with pancreatitis always occur after eating, and fasting significantly alleviates the condition.
Pancreatitis, in addition to pain that does not have a trigger point, does not cause tension in the abdominal muscle tissue. The consequences of such inflammatory processes can be fatty or hemorrhagic pancreatic necrosis, as well as primary or metastatic cancer. This can cause severe intoxication of the body and cause respiratory arrest.
Clinical picture of fatty pancreatic necrosis:
- the pain is localized in the left hypochondrium and radiates to the left shoulder;
- it is similar to an acute form of myocardium, but heart medications are powerless, but if you press your legs to your stomach, it becomes easier;
- vomiting does not provide relief and there is blood in its masses.
With hemorrhagic pancreatic necrosis, the pain will be even stronger, as well as:
- due to large amounts of blood entering the enzymes, renal failure will occur, diuresis will decrease, which will lead to increased signs of intoxication of the body;
- due to an excess of hormones and enzymes in the blood, the central nervous system will come under attack, which will affect the patient’s mental state, this will manifest itself in inappropriate decisions and actions, anxiety, depression of consciousness up to coma.
Diseases and dysfunctions affecting the pancreas are not limited to inflammatory processes. Although most pathologies are characterized by pain, dyspepsia and blood count characteristics, symptoms vary depending on the type of disease, its form, stage and extent of the pathology.
Laboratory studies are not very informative. Ultrasound, biopsy Exceeding the reference norms of glucose and glycated hemoglobin in the blood
| Disease/symptom | Chronic pancreatitis | Cancer | Cystic changes in glandular tissue | Diabetes mellitus type I |
| Painful sensations | During periods of exacerbation | Depending on the location and volume of the tumor | Depending on the size and location, they may be absent | None |
| Dyspepsia | During periods of exacerbation and if the diet is violated: constipation, diarrhea, nausea, vomiting | Unstable fatty stools, nausea, at a later stage - profuse diarrhea, vomiting | Depending on the location of the cyst: frequent stools, bloating (cyst on the head of the gland), constipation, nausea, discolored feces (body, tail of the gland) | Feeling of nausea, vomiting with ketoacidosis. Increased hunger during hypoglycemia |
| Features of the clinical picture | Exacerbations due to violation of dietary rules | Jaundice, pale skin, weight loss to the point of exhaustion | Expressed in late stages and bacterial suppuration by pain and the possibility of palpation of cysts | Increased thirst, frequent urination, itchy skin, dry mucous membranes. Ketoacidosis, hypoglycemia |
| Laboratory indicators and diagnostic methods | In exacerbations similar to acute pancreatitis | The blood picture shows anemia, leukocytosis, increased ESR. Ultrasound, biopsy |
Ulcerative changes in the glandular tissue of this organ are classified depending on the stage: erosive, exacerbation and chronic, with possible complications upon penetration into the tissues and organs of the peritoneum. The symptoms of the ulcer are similar to the clinical picture of pancreatitis with the additions of heartburn and salivation.
Therapy is carried out under the strict supervision of specialists. During treatment, it is necessary to remember that without following a diet, limiting fatty, fried, smoked foods, certain types of foods (mushrooms, tomatoes, honey) and alcoholic beverages, the disease will worsen and progress.
In case of severe pain, during an exacerbation of pancreatitis, most patients, as a rule, immediately seek medical help. The danger of pain in the pancreas is that in the chronic form of the disease, it is not expressed acutely and can be permanent, but very sluggish (aching) in nature.
Over time, a person gets used to such discomfort and stops paying attention to it altogether. At the same time, inflammation and destruction of pancreatic cells in the body slowly continues.
It is necessary to understand that pain is a direct symptom that something has gone wrong in the body and you should not delay your visit to the doctor. With properly selected therapy, as well as following the recommended diet, all the unpleasant symptoms of pancreatitis can be eliminated quite easily.
If a person systematically ignores pain in the left side, constant heaviness and discomfort, this can have more than serious consequences. Such as the development of diabetes mellitus or pancreatic cancer.
Related Posts
How to recognize the disease
Unfortunately, pancreatic diseases are difficult to diagnose in the early stages. At this time there are no pronounced symptoms yet.
Although, provided that the disease is detected early, the treatment initiated does not transform the inflammation into a chronic form. There are diagnostic methods such as clinical, laboratory and instrumental.
They allow us to determine the characteristics of the development of the disease. Thanks to this, doctors make an accurate diagnosis.
In the clinical method, the doctor examines the patient and talks with him. Based on this, a preliminary diagnosis is made.
This is not always objective, because often the signs of pancreatic diseases are similar to the symptoms of other diseases. To clarify, laboratory diagnostics are prescribed.
These are blood and urine tests. The presence of enzymes in them makes the situation clearer.
Instrumental methods include ultrasound examination, but computed tomography is more informative. Both of these methods examine the anatomical features of the pancreas:
- define contours;
- dimensions, density;
- duct diameter;
- the presence of inflammation and cysts;
- presence of stones;
- existence of tumors.
Child examination
Diseases of the liver and pancreas in children, unfortunately, occur frequently. The most common pancreatic disease in children is pancreatitis. Unfortunately, it can be asymptomatic or refer pain to other organs, so the disease of this organ is often confused with gastritis, dysbacteriosis and others.
In any case, at the slightest suspicion of pancreatitis in a child, you should consult a doctor who, with the help of several tests and examinations, can confirm or refute the diagnosis.
Tests and studies that the doctor may prescribe:
- Analysis of urine;
- saliva analysis;
- stool analysis;
- Ultrasound
- endoscopy.
At the moment, the risk of liver disease in newborns is quite high. This depends on many factors, but early detection of the problem will increase the chances of recovery and reduce the risk of complications if surgery is required.
Treatment of pancreatic diseases
What to do if the pancreas hurts and all the symptoms of the disease are present? First of all, consult a doctor. Similar symptoms occur in other diseases.
You will be prescribed tests and examinations. Based on the results, the doctor will decide how to treat the disease.
He will tell you what diet to follow. He will describe in detail how to treat, what medications to take.
These could be enzymes and pain pills. You cannot self-medicate.
Medicines must be prescribed by a doctor. He also prescribes control blood tests for enzymes and ultrasound examination.
How to cure the pancreas? This can only be done when the disease is not advanced and irreversible changes in the tissues have not occurred. But timely and correctly prescribed treatment is not everything.
Much depends on the actions of the patient himself. It is necessary to strictly follow the diet.
Eat five times a day. Remove fatty, fried foods and alcohol from your diet.
It is not advisable to eat sweets and starchy foods. Food should be low in calories.
The diet should contain:
- lean meat, poultry;
- dairy products;
- fruits other than citrus fruits;
- porridge with milk;
- eggs;
- slimy soups.
Herbal treatment is also used at home. Infusions of chamomile and burdock help well.
Dandelion tea and golden mustache treatment help improve the condition. Propolis, honey, and potato juice are used.
Why is it recommended to coordinate treatment with folk remedies with your doctor? It’s just that the use of these techniques has many contraindications. And only the doctor will determine what is right for you.
Treatment with oatmeal jelly, which is drunk every day, gives good results. To prepare you need:
- Pour 1 kg of oatmeal with three liters of water.
- Add 2 tablespoons of kefir.
- Leave in a warm place for a day until the mass rises.
- Strain through a colander into a large saucepan.
- Gradually add another 3 liters of water to the mixture remaining in the colander. It is necessary to squeeze out everything useful from oats.
- Leave the pan for 16-18 hours.
- Then drain the liquid from above, leaving the filtrate at the bottom.
- To prepare jelly, add 100 g of starter diluted in cold water to half a liter of boiling water.
Diagnostics
If pancreatitis is suspected, the doctor questions and examines the patient, paying attention to the color of his skin and mucous membranes. Sometimes the pain can have different localization depending on which part of the gland is damaged.
If there is pain above the navel in the right hypochondrium, it means that the head of the gland is involved in the pathological process, if in the left it is the tail. Vague girdle pain in the upper abdomen indicates damage to the entire gland.
You can differentiate problems with the pancreas and transverse colon as follows: the doctor palpates the painful area, first in a supine position, and then on the left side.
If the pancreas is affected, the pain in the side position will be less severe; if there are problems with the transverse colon, it will remain the same.
Laboratory tests include determining the levels of amylase, lipase, and trypsin in the blood serum. A general blood test shows an increase in the level of leukocytes.
Additionally, the activity of liver enzymes can be examined: ALT and alkaline phosphatase, as well as bilirubin; their increase may be a sign of an attack of pancreatitis provoked by gallstones.
Urine is also tested for amylase using the PABA (PABA) test, and feces are tested for the presence of chymotrypsin, trypsin and high fat content. To identify disorders of carbohydrate metabolism, the amount of glucose in the blood is determined.
Instrumental methods can be used:
- X-ray – with its help it is determined whether the pancreas is enlarged or not;
- Computed tomography or MRI - to clarify the diagnosis, identify pancreatic necrosis or fluid accumulation in the abdominal cavity;
- Ultrasound – to study the structure and nature of the contours of the gland, the condition of the common excretory duct, and determine the presence of gallstones.
Treatment
Diet is a very important element in the treatment and prevention of exacerbations of pancreatitis. If this is neglected, any medicine may be powerless.
Since the qualitative and quantitative ratio of enzymes produced by the gland changes depending on the composition of foods consumed at one meal, it is recommended to switch to separate meals in order to reduce the load on the gland, i.e. Eat proteins and carbohydrates at different meals.
You should also not overeat: the daily calorie intake should not exceed the norm corresponding to age, gender and physical energy expenditure.
Prohibited products:
- Fatty foods, fried foods;
- Sausages, canned food, smoked meats, pickles;
- Jellied meat, aspic;
- Alcohol;
- Sour juices;
- Strong tea and coffee;
- Confectionery (cakes, pastries), ice cream;
- Hot spices, herbs and seasonings, mustard, horseradish.
Medicines to improve liver function and treat pancreatitis
The range of drugs intended to improve liver function and pancreatic disease is large. If the pancreas and liver hurt at the same time, the victim is immediately admitted to the hospital for treatment, and joint therapy for the diseased organs is prescribed.
The following drugs are used to restore the liver and for pancreatitis, to treat the pancreas:
- To eliminate pathogenic microflora, antibacterial tablets are prescribed - Biseptol, Sigmamycin, Bactrim. Treatment of pancreas for pain in the liver is carried out over 7 days, a prerequisite is the intake of probiotics. Antibiotics are not used for pathogenic liver manifestations or during pregnancy;
- to get rid of acute spastic pain, medications with an analgesic effect and relieving spasms are used - Drotaverine, No-Shpa;
- To protect the digestive organs from destruction, they take hepatoprotectors - Heptral, Karsil, Gepabene.
These medications for the pancreas and liver are considered basic and are prescribed as a result of the cumulative manifestation of an acute inflammatory phenomenon in the organs.
However, carrying out treatment only with the help of these groups of medications is regarded as irrational. For more effective treatment, the patient also needs to take pills that help restore digestion. From the available list of medications, doctors often give preference to Creon and Panzinorm.
Use of hepatoprotectors
Hepatoprotectors are medications that can have a positive effect on the basic functionality of the liver, normalize the production of digestive enzymes, help protect cells from decay and restore the affected parenchymal tissue of the organ.
The following types of hepatoprotectors are distinguished:
However, their effectiveness has not been proven. However, if treatment is carried out in conjunction with drugs of this group, then favorable dynamics are observed.
Indications for the use of medications as treatment and prevention of the liver will be various conditions that aggressively affect the structure of the organ.
- If toxic hepatitis is observed or is of a viral nature.
- There is organ damage caused by alcoholic beverages.
- Primary boliary cirrhosis develops.
- Obesity.
- Conditions that occur with a progressive disorder of fat metabolism.
Children are often prescribed this group of drugs after suffering from mononucleosis, which is manifested by severe enlargement of the spleen and liver.
Lipotropic hepatoprotectors to support the organ, stimulate fat oxidation procedures, improve cholesterol metabolism with lipids, and reduce fat infiltration in the liver. Certain vitamin groups B and E provide a hepatoprotective effect and favor liver recovery, which is why they are included in joint therapeutic projects in the case of liver dystrophy and other related diseases.
Hepatoprotectors for protecting the liver are divided into:
- phospholipids - can improve the biochemical parameters of the organ, eliminate the dystrophic phenomena that have arisen, stabilize the membrane of hepatocyte cells, and also inhibit the necrosis of healthy areas. Phospholipids are prescribed as a complex therapy for alcohol dependence. The best medicines - Essentiale is taken in the presence of hepatitis, Essliver, a good drug for alcohol damage, Phosphogliv, it is recommended to drink in case of fatty hypostasis and alcohol intoxication, Livenciale;
- amino acids - help protect liver cells from the influence of toxins and products, normalize protein synthesis and lipid metabolism - Ornithine, Methionine. Drugs with ademetionine - Heptor, Heptral are prescribed in combination with addiction to alcohol, to slow down the formation of fibrosis and accelerate cell recovery;
- synthetic geapatoprotectors - have all the properties of the other groups, protect and restore the liver - Acetylcysteine, Ursodeoxycholic acid.
The best of the products, a group of hepatoprotectors, is Liv 52. The medication is endowed with a cumulative effect, the main components of which are:
- yarrow;
- chicory;
- capers;
- nightshade;
- Chinese cinnamon.
This medication has the following effects on the liver:
- Promotes restoration of the membrane structure of cells.
- Helps organ cells resist the toxic effects of pathogens.
- Increases the presence of P450 enzymes.
- Increases the production of proteins and complex lipids.
- Inhibits the process of transformation of adipose tissue and the occurrence of fibrosis.
- In case of metabolic disorders, it helps to improve.
It is important to remember that you need to take hepatoprotectors for a fairly long period of time, until the negative period of exposure to negative factors completely ends. This group of drugs is also used as a result of additional treatment, and is not a replacement for the main treatment.
Antiviral drugs for liver pathology
If changes in the functionality of the pancreas and liver were caused by microorganisms of viral origin, then the treatment course is aimed at using medications to eliminate the virus.
In the treatment of the liver, a combination of effective drugs is used - Interferon, Ribavirin. Thanks to Interferon, immunity against the virus is increased and the growth of pathogenic cells is suppressed. In addition, the agents do not allow viral synthesis to occur. Joint treatment is used in the presence of hepatitis B and C of viral origin.
However, such medications are contraindicated for use in patients who have chronic liver failure, the destructive effects of these organs, and autoimmune diseases. Drugs are also judiciously prescribed during pregnancy and lactation.
Other inexpensive antiviral agents.
The treatment procedure using medications that relieve inflammation takes 5-10 days. It is permissible to combat the symptoms of liver and pancreatic diseases only after consulting a doctor and prescribing a dosage for adult patients and children, in each specific situation. In the joint treatment of pancreatic and liver failure, the organs are treated using folk remedies.
How to get rid of pain
Before treating the disease, it is necessary to take tests and undergo a comprehensive examination. A sick person is prescribed bed rest and avoidance of unhealthy and fatty foods. A prerequisite is drinking plenty of fluids, which helps reduce attacks of pain, and doctors also advise applying ice to the abdominal area.
Drug treatment is carried out in a hospital setting and includes the use of anticholinergic drugs such as Gastril and Pirenzepine; in addition, specialists prescribe antibiotics, antispasmodics and enzyme preparations to the patient.
A healthy diet plays a significant role in eliminating pain in the pancreas. As the person feels better, he is allowed to take food in small portions, however, his menu must be agreed with the attending physician.
Drugs such as Mezim and Festal promote complete digestion of food, and in case of chronic disease, enzymes should be taken constantly.
A diet for pancreatic health involves eating steamed dishes, as they retain nutrients and do not harm the body.
It is important to know that the break between meals should be on average 2 hours, and the food should be served warm; hot and cold treats are contraindicated. All foods must be crushed, and most of the usual dishes are prohibited to the patient.
So, you can’t eat smoked, fatty and fried foods, canned food and confectionery; you need to exclude alcoholic drinks, strong coffee and rich black tea from the menu.
The diet for diseases of the pancreas consists of low-fat fermented milk products - kefir, cottage cheese, fermented baked milk, you can add cheese without spices to the menu. For meat, it is preferable to choose chicken, turkey, rabbit, veal and beef, cooked in a double boiler.
Fish dishes are also considered healthy and reduce pain; pike, pike perch, cod and bream are suitable for this purpose.
The diet allows the consumption of boiled and baked vegetables; it is best to grind them and make them in the form of soups. It is allowed to introduce steamed omelet into the patient’s diet; it is advisable to choose rice, buckwheat, oatmeal from cereals; it is also allowed to eat pasta.
It is best to replace juice and other drinks with natural homemade compotes and jelly, and it is also useful to drink a medicinal herbal decoction. In general, a healthy diet helps keep pancreatic pain to a minimum.
Possible pathologies
A person may encounter different diseases, so it is difficult to tell from the symptoms what exactly they are dealing with. After the examination, the doctor will prescribe additional examinations in order to make an accurate verdict. You can only guess on your own which diseases of the liver and pancreas have affected the organs.
Common liver diseases
The liver cleanses the human body of toxic substances and is involved in digestion. If the condition of the organ worsens, then health problems arise in general.
What diseases can you encounter:
- Cirrhosis. With it, the structure of the liver vessels and tissues changes. If a problem with the bile ducts is added to the pathology, then biliary cirrhosis is diagnosed. The disease progresses rapidly and is fatal.
- Infectious hepatitis. Diffuse damage to the organ is observed, that is, a disruption of the structure occurs. The patient's stool and urine color changes, and his stomach often hurts. Specific signs depend on the type of hepatitis.
- Worms. If parasites have settled in the liver, then its tissue will change. Symptoms can be either absent or severe. Only laboratory tests can help identify the presence of worms. If parasites are found, you will have to immediately begin fighting them.
- Hepatosis. The patient experiences a metabolic disorder in hepatocytes. Instead of normal tissue, adipose tissue appears, which causes the size of the organ to change. Pathology can be provoked by abuse of alcoholic beverages and fatty foods.

If the disease is not treated in time, then diabetes, oncology, pancreatitis, cysts and other problems may develop against its background. You cannot ignore warning signs or choose medications on your own, as your health depends on it.
Pancreatic diseases
The pancreas is made up of different tissues. From them the stroma is formed - a connecting frame responsible for support. There is also parenchyma - these are the cells responsible for the synthesis of juice and hormones. Diseases of the liver and pancreas lead to inflammatory processes.
When the parenchyma is affected, this condition is often caused by ethanol, fatty and spicy foods. The cells gradually die, connective or adipose tissue appears. The problem often worries people with diabetes.

Replacement tissue can form in both chronic and acute pancreatitis. In any case, the functions of the pancreas are significantly impaired. If a person is not treated, then his health will quickly deteriorate. Diseases of the pancreas and liver worsen the condition of the entire body and especially affect digestive function.
Diagnostic methods used
Pathology in the pancreas and transverse colon is defined as follows:
- patient interview;
- palpation of the pain site while lying on your back, on your left side;
- ordering laboratory tests.
If the pancreas is affected, then lying on your side the discomfort will subside a little. And if the cause is in the transverse colon, then its intensity will not change. The laboratory will check the level of essential enzymes in the blood serum. They will take a general blood test to determine the number of white blood cells and whether there is an increase in them.
They may also prescribe determination of the activity of liver enzymes and bilirubin, because this patient’s condition is sometimes provoked by gallstones. You will need to submit your urine for a PABA test and feces for chymotrypsin, trypsin, and fats. Problems with carbohydrate metabolism will be determined by the level of glucose in the blood.
Simultaneous treatment
If changes are observed in the activity of the liver, pathologies of the pancreas often develop, because these organs are involved in the functioning of the digestive system together.
In the case of simultaneous appearance of symptoms of hepatitis with pancreatitis, therapy for this form of the disease is carried out under the supervision of a doctor, adhering to certain principles. Joint treatment of the liver and pancreas favors:
- taking medications with a defensive barrier - Phosphogliv, Essentiale, Heptral. These medications can protect the diseased pancreas and liver from extraordinary diseases provoked by alcoholic drinks and fatty foods. In addition, any of the drugs reduces stagnant processes;
- taking herbal medicines - Silimar, Gepabene, Legalon 140. Medicines prevent the development of the destructive process, restoring liver failure, and normalize the production of secretions by the pancreas;
- infusion treatment is prescribed - preparations of salts and insulin are injected into the vein, which makes it possible to reduce the occurrence of poisoning that develops after inflammation of the digestive organs, as well as restore the acid-base balance;
- With the help of vitamin complexes, the immune system is strengthened.
A strict diet is inevitable in treatment. The doctor will tell you which foods are good for the human liver and pancreas. He will also recommend some effective recipes from the people.
When adjusting the table and prescribing traditional methods of treatment, the doctor pays attention to the patient’s condition. Special care is given to children and the elderly when medications are selected. Medicines to prevent relapse of pathology are also prescribed only by a doctor.

The work of all internal organs is closely interconnected. A disruption in the functioning of one provokes dysfunction in the second. This connection is especially pronounced between the organs of the gastrointestinal tract, hepatobiliary system and pancreas. When diagnosing inflammatory processes accompanied by functional disorders, conservative therapy is used. In consultation with your doctor, you can supplement the treatment of the liver and pancreas with folk remedies.
Complications
Quite often, cholecystitis (inflammation of the gallbladder) is associated with pancreatitis, and, on the contrary, cholecystitis can provoke the development of pancreatitis. Often, acute pancreatitis is accompanied by infection (purulent complications).
Cellulitis or abscess of the pancreas develops. In some cases, intra-abdominal bleeding develops.
Another serious complication of pancreatitis is the destruction of the pancreas and the development of deadly peritonitis.
After acute pancreatitis, the disease becomes chronic. Exacerbation of chronic pancreatitis is usually provoked by irritating foods and alcohol. Chronic pancreatitis can cause the development of diabetes mellitus.
Contraindications to treatment with folk remedies
Despite the benefits of traditional therapy, its remedies are not always approved for use. Before you start taking such drugs, you must carefully study the properties and contraindications for the use of each plant. It is not recommended to use herbs independently during the acute stage of inflammation of the liver, pancreas and gall bladder. In order not to provoke complications, it is necessary to carry out herbal medicine according to the rules:
- preliminary examination and consultation with a doctor;
- using only natural raw materials that have a quality certificate;
- strict compliance with the instructions for use in compliance with the recommended doses.
You cannot stop or prescribe new medications yourself. Following these recommendations will improve your health and will not cause harm.