Kinds
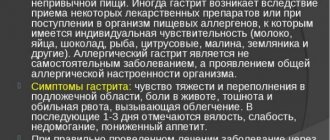
Gastroesophageal reflux disease affects the mucous epithelium of the esophagus and stomach. In medicine, there is a certain classification of the disease, taking into account the course of pathological processes and the area of damage to the digestive system.
| Name | Description |
| Non-erosive | The inflammatory process affects the mucous membrane of the esophagus. Small pathological lesions are distinguished by redness. |
| Erosive | Small erosions form on the affected areas of the mucous membrane, which can merge with each other. The pathological condition in some situations is complicated by the occurrence of bleeding. |
| Barrett's esophagus | A severe form of the disease in which all layers of the stomach are affected. |
In each individual case, pathological changes are accompanied by accompanying clinical signs. They will help the gastroenterologist determine the extent of damage to the digestive system and select the most effective treatment.
Gastroesophageal reflux disease and gastric ulcer
When you have a stomach ache, it affects all areas of your life by causing inconvenience. The pain itself is a distraction because the person is worried about finding out the cause. Gastroesophageal reflux disease
(
GERD
) and
stomach ulcers are common diseases that can sometimes be confused and difficult to diagnose because both diseases have similar symptoms and cause stomach pain.
In addition, gastritis also has similar symptoms; you can read about the treatment of gastritis here. While ulcers do not cause acid reflux, these diseases can sometimes co-exist in a person. Doctors rely primarily on symptoms and tests to diagnose acid reflux and stomach ulcers. The causes and treatments for ulcers and acid reflux vary, so an accurate diagnosis is necessary to determine the best treatment.
In any case, you should schedule a visit to your doctor to find out whether you are worried about GERD or an ulcer. Both ulcers and GERD need to be treated by seeking help from a gastroenterologist.
So, gastroesophageal reflux disease and gastric ulcer - differences:
Ulcer or gastroesophageal reflux disease (GERD): stomach discomfort
Although the two diseases are similar, they are actually different, even if they are accompanied by identical symptoms. According to some reports, every fifth person experiences heartburn at least once a week. Stomach discomfort can easily negatively affect your life, which can lead to the following consequences:
- Losing sleep
- Difficulties related to social activities
- Problems with eating and drinking
Ulcer or GERD: Understanding the Differences
An ulcer is a small sore or lesion on the wall of your stomach or duodenum, or intestines. This disease is often aggravated by stomach acid, but it is not usually the acid that causes the ulcer. Most likely, the cause is either a bacterium known as Helicobacter pylori (H. pylori) or any medications you have been taking for a long time.
Gastroesophageal reflux disease means that stomach acid rises up from the stomach into the esophagus, causing a burning sensation (sometimes called acid indigestion or heartburn) and bad breath. These “attacks” must occur at least twice a week for gastroesophageal reflux disease to be diagnosed. Read also about how to get rid of bad breath.
Most patients with GERD experience heartburn or belching, a feeling that something is coming back into the throat.
Ulcer or GERD: Know the Symptoms
An ulcer is often accompanied by the following symptoms:
- Burning sensation in the intestines, approximately between the navel and chest
- Pain or discomfort two to three hours after eating
- Night abdominal pain
- Pain that is relieved by eating, drinking, or taking special medications
- Blood in the stool or vomiting. You can find out about methods of treating the stomach after vomiting here.
Some symptoms of GERD that are not typical for ulcers:
- Sensation of sour taste in the back of the mouth
- Dry cough
- Sore throat
- Swallowing problems
- Symptoms similar to asthma
- Increased heartburn in response to certain foods
- Symptoms worsen when you lie down or bend over
Ulcer or GERD: diagnostics
When an ulcer is suspected, endoscopy . If GERD is suspected, a therapeutic trial involving acid-lowering medications is done to determine whether these medications control your symptoms.
Depending on your symptoms, your doctor may also refer you to:
- Blood analysis . This will show if you have H. pylori.
- Examination of the esophagus with barium . With this test, you will drink liquid, and then a radiologist will take an X-ray of your esophagus, stomach, and intestines. This can show whether you have ulcers or any structural changes that are causing your symptoms.
- Endoscopy . For this test, the doctor uses a thin, flexible tube with a camera inserted down the throat to look at the inside of the esophagus and stomach. The camera allows the doctor to see ulcers or other problems, such as scarring of the esophagus, that may be caused by GERD.
Prevention of diseases of the stomach and esophagus:
- Proper nutrition. The basics of proper nutrition are based on the fact that it is necessary to consume all groups of nutrients - proteins, fats, carbohydrates, minerals and vitamins. You should give preference to fresh vegetables, fruits, freshly squeezed juices, whole grain cereals, black bran bread, dietary meat and fish.
- Fatty, sour, spicy - exclude. Foods that are too spicy or sour can harm your esophagus and stomach because they burn the stomach walls. However, if you are a resident of eastern countries and are accustomed to eating spicy food, then you will not have problems, since your stomach has long been accustomed to spicy food.
- Eat often. It is recommended to eat 3-6 times a day. This way you won’t feel hungry during the day and your stomach won’t “recycle itself.” Remember to have healthy snacks in the form of yogurt, fruits, nuts and so on.
- Don't drink coffee on an empty stomach. This negatively affects his work. Read more about the dangers of coffee on an empty stomach here.
- Don't go hungry. In pursuit of an ideal figure, many women decide to give up food, but such a decision will only have a detrimental effect on your health, and it will not bring much benefit to your figure either, since the kilograms lost by such a harsh method will soon return as soon as you return to your normal diet, Yes, and you can gain even more weight. When you fast, due to lack of nutrients, the stomach begins to digest itself, and as a result of these processes, ulcers form.
Stages and degrees
Taking into account the development of pathological processes and the boundaries of damage to the mucous membrane of the digestive organs, in medicine the following degrees of gastroesophageal reflux are distinguished:
| Name | Description |
| I degree | The patient has complaints, but there are no pathological changes on the surface of the mucosal epithelium. |
| II degree | Single shallow foci of the inflammatory process appear on the surface of the mucous layer. |
| III degree | Erosion of varying depths and sizes forms on the walls of the stomach. |
| IV degree | A peptic ulcer of the esophagus develops. A severe form of gastroesophageal reflux, which can lead to dangerous complications (bleeding, perforation of the walls of the esophagus, development of a malignant tumor). |
A comprehensive diagnosis, which is prescribed by a gastroenterologist after examining the patient, will help determine the type of disease and the degree of development of the inflammatory process. The examination results are also necessary to draw up the correct treatment regimen, in the absence of which serious complications will develop.
Symptoms
The clinical picture of gastroesophageal reflux disease depends on the provoking factors and the degree of damage to the digestive system. The gastroenterologist, guided by the patient’s complaints, will prescribe the person the most informative examination in order to establish the correct diagnosis.

GERD (symptoms and treatment are determined by the doctor after a thorough examination of the patient) is accompanied by the following symptoms:
| Name | Symptoms |
| Esophageal signs |
|
| Extraesophageal manifestations |
|

In most cases, GERD symptoms worsen after eating, when the patient does not follow a specially formulated diet. Many people also complain of headaches, general weakness in the body, and sleep disturbances. Patients become weather dependent.
Diagnosis of gastroesophageal reflux disease (GERD)
Provocative tests, pH determination, scintigraphy, biopsy and esophageal manometry help diagnose gastroesophageal reflux disease (GERD). X-rays and esophagogastroscopy can determine whether there is damage to the mucosa. The presence of damage to the mucous membrane cannot, however, absolutely prove that the cause of the patient’s symptoms is reflux. On the other hand, normal biopsy findings do not exclude the possibility of GERD. Many people with typical symptoms of GERD and the abnormal appearance of acidic contents in the esophagus do not have signs of esophagitis. Therefore, an extremely important component of the evaluation are diagnostic tests to establish a causal relationship between the appearance of acidic contents in the esophagus and clinical symptoms.
- Provocative test
Bernstein's provocative test for mucosal sensitivity to acid, which confirms the connection between symptoms and the effect of acid, is 80% effective. It consists of irrigating the esophagus with a 0.1N solution of hydrochloric acid and saline solution (placebo). The test is considered positive when the patient’s symptoms in case of acid irrigation are reproduced. The sensitivity of the test increases with severe forms of esophagitis, but in the case of esophageal metaplasia it decreases. Another difficulty is the differences between techniques. For example, increasing the duration of irrigation increases sensitivity but decreases specificity.
Other provocative tests induce reflux during a barium esophagogram or a standard acid reflux test. These tests are important, but give false positive results in at least 20% of healthy people. There is also a scintigraphic detection of reflux. A common method is the use of an intragastric portion of labeled technetium, after which reflux is provoked by the methods described. The sensitivity of this method ranges from 14% to 90%. Recent studies have shown that scintigraphy, compared with 24-hour pH monitoring, is less sensitive (36%) and gives positive results in only 50% of patients with esophagitis.
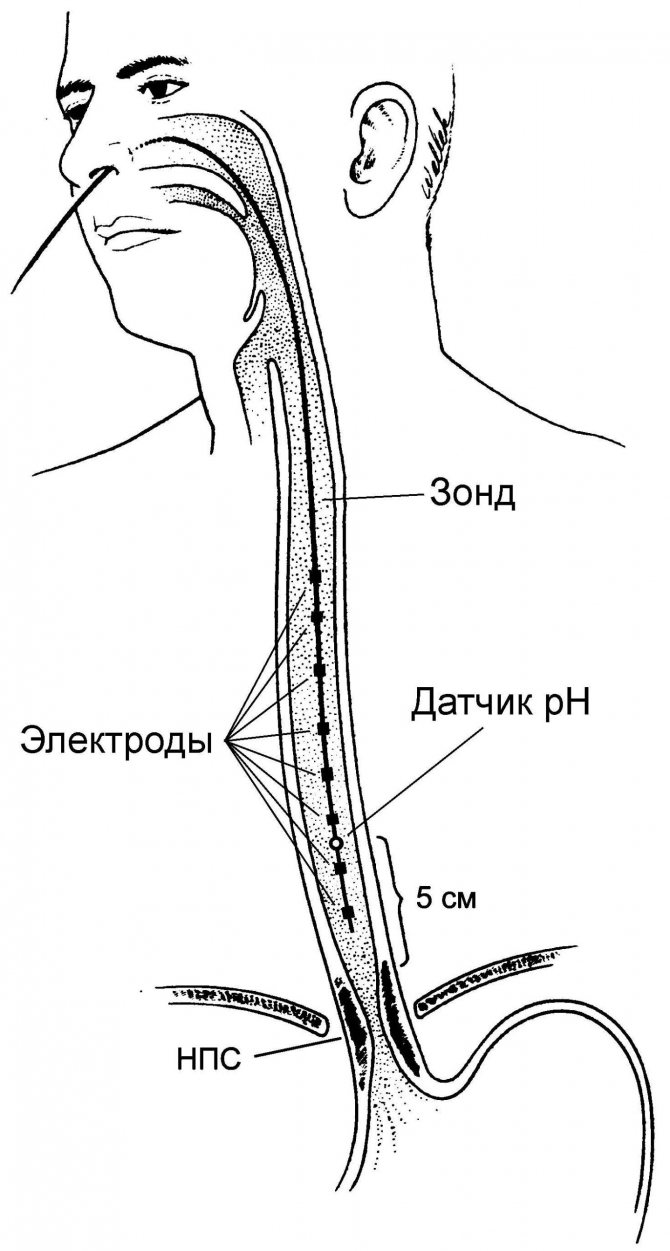
- pH determination
Long-term ambulatory intraesophageal pH monitoring detects excess reflux with or without appropriate clinical care. The reproducibility of ambulatory pH determination is 84-93%.
Because pH testing is normal in 23% to 29% of patients with proven esophagitis, and the severity of reflux varies when esophageal pH is monitored with two parallel tubes, this has raised doubts about whether pH testing can be considered the “gold standard” for GERD. The sensitivity and specificity of the method are difficult to assess without an additional standard that would make it possible to compare its data with the results of ambulatory monitoring. Although pH determinations are usually carried out over a 24-hour period, it has been found that short periods of monitoring in individuals can provide adequate information.
In patients with symptoms typical of GERD and proven esophagitis, there is little benefit from pH testing. But in patients with atypical symptoms of reflux, especially with pain of unknown origin in the chest and without signs of esophagitis, in people with pulmonary symptoms or chronic hoarseness, ambulatory pH-metry helps determine the causes. Identifying signs of reflux by monitoring pH provides valuable prognostic information, since reflux only in a horizontal position or both in a horizontal and vertical position is more resistant to treatment than reflux that occurs only in an upright position. An additional use of pH monitoring is to assess the condition of individuals who have resistant symptoms despite treatment. In some of these patients, even intense inhibition of the acid-forming function of the stomach does not reduce the pathological reflux of acidic contents into the esophagus.
- Esophageal manometry
Read also Acute intestinal obstruction - causes, classification, symptoms, diagnosis, treatment
Esophageal motility studies can provide valuable diagnostic and prognostic information. Manometric localization of the lower esophageal sphincter (LES) facilitates accurate determination of esophageal pH. Thus, catheter intubation is often necessary to obtain complete manometry. Detection of a high percentage of pathological contractility and/or the presence of decreased tone of the LES not only indicates the severity of GERD, but also provides for great difficulties with long-term treatment.
The role of peristaltic dysfunction in GERD remains unclear, but recent studies have found that 50% of patients with various forms of esophagitis had some degree of esophageal motility dysfunction. Transient relaxation of the LES may be a major mechanism of GERD, but is rarely detected during diagnostic manometry. Esophageal manometry, confirming the presence of effective esophageal peristalsis, may be useful when considering antireflux surgery.
Causes
Gastroesophageal reflux disease, as the inflammatory process progresses, damages the mucosal epithelium to varying degrees. Erosion and ulcers appear, the esophagus becomes inflamed. A serious complication of pathological processes is the proliferation of connective tissue or cell degeneration.
There are the following provoking factors against which gastroesophageal reflux occurs:
- poor nutrition;
- bad habits (abuse of alcohol and tobacco products);
- stressful situations, emotional stress, nervous exhaustion;
- extra pounds, varying degrees of obesity;
- hormonal imbalance (gestation period, menopause, menstrual cycle);
- treatment with certain medications;
- genetic inheritance;
- damage to the esophagus;
- neuromuscular disorders of the esophagus against the background of frequent exacerbations of the inflammatory process;
- damage to the respiratory organs (bronchial asthma, obstructive bronchitis);
- great physical activity;
- staying in a forward leaning position for a long time;
- high pressure in the abdominal area.
A hiatal hernia can also provoke the reflux of stomach contents into the esophagus. The main reason is impaired functioning of the lower esophageal sphincter as a result of neurovegetative failures.
GERD - what kind of disease is it?
GERD (gastroesophageal reflux disease) is a disease of the esophagus and upper stomach, characterized by the presence of reflux of gastric juice from the underlying sections into the esophagus. GERD is a common condition with an increasing trend in all countries of the world.
Reflux is a pathological reverse reflux of stomach contents into the upper parts of the digestive system, during the long-term existence of which specific changes in the mucous membrane form and progress in the esophagus, due to the long-term maintenance of an unusually acidic environment in the esophagus.
The esophagus and stomach are separated from each other by a muscle called the sphincter, which does not allow (with some exceptions) the food bolus from the stomach to enter the esophagus. Under the influence of various pathological factors, the presence of predisposition, discoordination of neuromuscular transmission, increased intra-abdominal pressure and other reasons, conditions are created for the possibility of the existence of permanent gastroesophageal (gastroesophageal) reflux and disease, abbreviated (from the first letters) as GERD.
Being a pressing problem in gastroenterology, GERD can cause a lot of problems for a person with gastroesophageal reflux. In severe cases, GERD significantly affects the patient’s well-being and reduces the patient’s quality of life.
GERD is often hidden under the guise of other diseases of adjacent organs, and often with this pathology, patients present numerous complaints that mimic diseases of the heart, spine, muscles and even lungs. This is due to the proximity of these organs to the esophagus. The opposite situation is also common, when completely different diseases are mistaken for GERD.
It should be noted that GERD can cause many diseases of the esophagus and bronchopulmonary system (esophagitis, ulcerative esophagitis, asthma, chronic bronchitis, laryngitis, pharyngitis). Difficulties in diagnosis and the variety of symptoms of GERD dictate that the patient must consult a doctor when symptoms of GERD or any other symptoms that bother the patient appear.
Despite the polysymptom nature of the disease and the ability to hide under the guise of other diseases, GERD has very clear symptoms and clinical manifestations, which, however, only a doctor can understand. Let's try to look at the main causes, signs and symptoms of GERD, as well as the principles of treatment for this common disease of the digestive tract.
Diagnostics
GERD (symptoms and treatment are recommended to be discussed with a gastroenterologist) requires a comprehensive diagnosis to establish the cause of the inflammatory process and the area of damage to the digestive organs.
Patients are prescribed the following examination methods:
| Name | Description |
| pH-metry of the stomach and esophagus | The results will help determine the duration and severity of gastroesophageal reflux. |
| pH-impedancemetry | Diagnostics allows you to identify acidic, slightly acidic or slightly alkaline refluxes, as well as differentiate their structure.
|
| Endoscopy | The doctor examines the digestive organs, determines the degree and stage of the inflammatory process. |
| Radiography | A diagnostic method that is prescribed to patients to exclude the development of a hernia. |
| Ultrasound examination (ultrasound) | The specialist examines the internal organs, assesses their condition, functioning and identifies pathological processes. |
| Esophagogastro-duodenoscopy | During the examination, the doctor performs a biopsy. The taken material is examined in the laboratory. The results will help identify malignant processes. |
| Esophageal manometry | During the examination, the contractility of the esophagus and pressure in the area of the lower sphincter are assessed. |
To avoid damage or injury, many patients are prescribed proton pump inhibitors by gastroenterologists. The patient takes the medicine for a week and comes back for diagnostics. If the pathological symptoms have disappeared, the doctor assumes that the person has GERD. This diagnostic method helps if other tests have not revealed inflammation and damage to the gastric mucosa.
When to see a doctor
You should visit a gastroenterologist when the first disturbances in the functioning of the digestive organs appear. Timely diagnosis and properly selected therapy will prevent serious consequences that radically worsen a person’s quality of life.
It is important to undergo a comprehensive examination and differentiate the disease, since many pathologies are accompanied by similar clinical signs. Considering the provoking source of GERD, the patient may need to consult other specialized specialists (pulmonologist, otolaryngologist, cardiologist, surgeon).
Prevention
Simple recommendations from a doctor will help prevent gastroesophageal reflux or exacerbation of pathological processes:
- A person needs to eat right and give preference to healthy foods.
- Monitor your weight and prevent weight gain.
- Completely eliminate any provoking factors that cause stomach contents to reflux into the esophagus (physical activity, heavy lifting).
- To refuse from bad habits.
- Take medications only as prescribed by your doctor.
You should not try to treat diseases or disorders of the digestive system on your own. A gastroenterologist must make a diagnosis, as well as prescribe medications.
Treatment methods
Complex therapy is prescribed to patients after a thorough examination. The gastroenterologist, taking into account the patient’s condition and diagnostic results, selects the most effective methods of therapy.

Medicines, folk remedies and other measures help eliminate the symptoms of gastroesophageal reflux and also improve the patient’s condition.
Medications
GERD (symptoms and treatment require a full diagnosis) cannot be eliminated without traditional medications. Drug therapy is aimed at eliminating the symptoms of gastroesophageal reflux and improving the patient’s quality of life.
Medicines will help restore the functioning of the digestive system and prevent complications. Patients should adhere to the prescribed dosages or carefully read the instructions before starting therapy.
| Group of drugs | Name | Application |
| Proton pump inhibitors | Omeprazole, Rabeprazole | Medicines reduce the negative effects of stomach acid on the esophageal mucosa. It is preferable to take the drug in the morning. The recommended dosage for an adult patient is 20 mg. The course of treatment lasts 2-4 weeks. |
| Antacids | Phosphalugel, Gastal | Medicines eliminate the process of reflux of stomach contents into the esophagus, preventing the development of the inflammatory process. It is recommended to dilute the product in a small amount of liquid or wash it down with water. Patients are prescribed 1-2 sachets 2-3 times a day. |
| Adsorbents | Smecta, Diosmectite | The agents neutralize hydrochloric acid and remove bile acids. The medicine should be taken 3 g 3 times a day for 3-7 days. Mix the contents of the sachet in 0.5 tbsp. water. |
| Prokinetics | Metoclopramide, Domperidone | The drugs improve the motor-evacuation function of the digestive system. The medicine should be taken orally with a sufficient amount of water. Adults are prescribed 10 mg 3 times a day. |
| H2 receptor antagonists | Ranitidine, Famotidine | For adult patients, the medicine is prescribed 0.15 g in the morning and evening or 0.3 g at bedtime. The duration of treatment is 4-8 weeks. |
| Gastroprotectors | Sucralfate, Venter | Medicines form a certain layer on the mucous epithelium, protecting it from the negative effects of aggressive factors. Adult patients are prescribed 1 g 2 times a day. The duration of therapy is 1-1.5 months. |
| Ursodeoxycholic acid | Ursofalk, Ursosan | It is recommended to take the capsules whole with a sufficient amount of water. Patients are prescribed 250 mg 1 time per day, preferably in the evening. The course of treatment lasts 10-14 days. |
Additionally, patients are recommended to drink special mineral water (Kazachinskaya, Essentuki). In severe situations, when drug therapy has not given a positive result or when erosions or complications occur, patients are advised to undergo surgery. The same applies to the formation of a stricture or scarring in the stomach area.
Traditional methods
Symptoms of GERD can be eliminated with unconventional remedies. Numerous herbs and natural ingredients have healing properties. Recipes from healers and healers can be used for GERD only in complex treatment after consultation with a doctor.
It is important to choose the most effective remedy to prevent the occurrence of an allergic reaction or individual sensitivity.
| Name | Recipe | Application |
| Aloe juice | Grind the leaves of the plant and squeeze out the juice. Mix 1 tsp. with natural honey (0.5 tsp). Leave the resulting mass for 2-3 hours and take orally. | It is recommended to take 1 tsp of the finished medicine. after meal. Aloe juice reduces inflammation and promotes healing of damaged mucous membranes. |
| Nettle | Wash the leaves of the plant, dry and chop. Pour boiling water (1 tbsp) into 2 tbsp. spoons of the resulting mass. Leave and strain the solution. | The resulting product is recommended to be taken orally 2-3 times a day for 2-3 weeks. For taste, you can add a small amount of sugar or natural honey (1 tsp) to the nettle decoction. |
| Flax seeds | Pour 2 tbsp. seeds with boiling water (500 ml). Leave for 8 hours and strain well. | A decoction of flax seeds is recommended to be taken orally 3 times a day before meals. The adult dosage is 0.5 tbsp. The course of treatment lasts 5-6 weeks. |
| Marshmallow root | Grind the plant and pour 6 g of powder with warm water (1 tbsp.). Place the resulting mass in a water bath and heat for another 30 minutes. | It is recommended to take the finished marshmallow decoction chilled, 0.5 tbsp. 3 times a day. |
| Herbal collection | Mix marshmallow and licorice root, flax seeds and coltsfoot leaves in equal proportions. Pour 1 tbsp. herbal mixture with boiling water (1 tbsp.). Leave for 30-40 minutes and strain. | The resulting decoction should be taken orally, 1 tbsp. 5-6 times a day before meals 30 minutes. |

For gastroesophageal reflux, it is recommended to drink a decoction prepared with chamomile. The plant has anti-inflammatory and analgesic effects. Various herbal infusions in folk medicine help damaged tissues of the mucous membrane of the stomach and esophagus to heal and recover faster. Herbs also have a calming effect.
Diet
A specially formulated diet for the development of gastroesophageal reflux will help reduce the load on the organs of the digestive system.
| Recommended Products | Prohibited Products |
|
|

It is necessary to eat small portions, the food should be warm. Dishes should be boiled, steamed, and it is also recommended to reduce salt consumption.
Other methods
GERD (symptoms and treatment are determined by a gastroenterologist) requires not only complex therapy, but also changes in the patient’s lifestyle.
The following recommendations must be followed:
- Monitor your body weight and avoid gaining extra pounds.
- It is necessary to completely abandon bad habits. Nicotine enhances the production of hydrochloric acid.
- You should not overeat or eat food before bed.
- Patients are not recommended to wear tight belts, corsets, bandages or tight clothing. In this case, intra-abdominal pressure increases.
- You cannot lift weights or stress your abdominal muscles.
It is not recommended to take a horizontal position for 1-2 hours after eating, as the risk of worsening the disease increases. The same applies to physical activity, exercises and bending the torso forward.

Additionally, in complex therapy, patients with GERD are recommended to attend physiotherapeutic procedures that improve the functioning of the digestive organs and reduce the development of the inflammatory process:
- radon baths;
- mud treatment;
- electrophoresis with antispasmodics;
- sinusoidal modulated currents.
Magnetic therapy and electrosleep eliminate the manifestations of pathological processes.
Symptoms of GERD
What symptoms can be used to determine the presence of GERD? Doctors divide the symptoms of GERD into two groups:
- esophageal;
- extraesophageal.
Esophageal symptoms:
- belching;
- heartburn;
- sour taste in the mouth;
- frequent regurgitation;
- disruption of the normal swallowing process;
- vomit;
- frequent hiccups;
- a feeling of heaviness behind the sternum, a lump in this area.
There is the so-called Montreal classification of GERD symptoms.
Esophageal symptoms:
- Clinical manifestations of GERD (typical manifestations and non-coronary pain in the sternum).
- Symptoms of esophageal damage (adenocarcinoma, reflux esophagitis, Barrett's esophagus, peptic stricture of the esophagus).
Extraesophageal symptoms:
- In which a relationship has been established (reflux-associated laryngitis, cough, erosion of tooth enamel, bronchial asthma).
- Manifestations that can presumably be associated with gastroesophageal reflux (sinusitis, pharyngitis, recurrent otitis media, idiopathic pulmonary fibrosis).
Why do extraesophageal lesions occur? This is due to the fact that the refluxant enters the respiratory tract and has a significant irritant effect. In this case, reflexes are triggered: esophagobronchial and esophagocardial.

Extraesophageal symptoms:
- Pulmonary syndrome (shortness of breath that appears when a person lies down, cough).
- Otorhinolaryngopharyngeal syndrome (reflex apnea, rhinitis, otitis, pharyngitis or laryngitis may develop).
- Dental syndrome (periodontal disease, caries).
- Anemic syndrome. It manifests itself at a late stage of development of the disease and is associated with the fact that erosions appear on the walls of the esophagus. They can bleed, causing hemoglobin levels to decrease.
- Cardiac syndrome (arrhythmia is observed, the patient feels pain in the heart area).
Heartburn, or a painful burning sensation localized behind the sternum, along the esophagus, is a very common symptom of GERD, occurring in most cases with reflux. The symptom of heartburn with GERD is a typical manifestation of this disease and is caused by the release of acidic contents into an environment that has a neutral pH. According to statistics, 20-40% of the population constantly or periodically experience heartburn.
Chest pain and heaviness with GERD are also a common occurrence that forces the patient to consult a doctor. The pain in this case is caused by spasm of the esophagus and the irritating effect of hydrochloric acid on the epithelium. Pain and burning with GERD intensify after errors in diet (rich, fatty foods, high-carbohydrate foods, fried and spicy foods, coffee, chocolate, sour foods).
Sour belching is often combined with pain in the chest, behind the sternum and is a typical symptom of GERD. Often, patients are forced to take quick-acting antacids to relieve these and other unpleasant symptoms.
A cough, dry or wet, long or protracted, often with GERD at the onset of the disease is not associated with esophageal pathology. Patients are unsuccessfully treated for “bronchitis and acute respiratory infections.” In patients with GERD, due to constant irritation of the upper respiratory tract and pharynx by acid, chronic laryngitis, sinusitis, pharyngitis with corresponding symptoms (sore throat and hoarseness, constant tickling sensation) occur and are diagnosed.
In some cases, GERD can initiate the appearance and progression of even a disease such as bronchial asthma, with typical attacks of shortness of breath or dry cough, chronic bronchitis.
Possible complications
Gastroesophageal reflux disease must be treated under the supervision of a gastroenterologist.
Otherwise, the patient will face serious complications:
| Name | Description |
| Perforation of the stomach walls | Violation of the integrity of the walls of the stomach most often occurs in the area of the mediastinal organs. As a result, sepsis develops, there is a high probability of respiratory arrest and severe bleeding, as a result of which the patient dies. |
| Formation of bleeding ulcers | There are obvious or hidden ulcers. The latter are the most dangerous to human life; they are difficult to identify, even during a medical examination. Hidden bleeding prevents the doctor from making an accurate diagnosis. Incorrectly selected therapy can be fatal. |
| Narrowing of the lumen of the esophagus | Stenosis leads to the patient completely refusing to eat, since food has difficulty passing through the esophagus. |
A dangerous complication of GERD is the formation of adenocarcinoma, when the affected tissue degenerates and a malignant tumor develops.
GERD does not threaten human life if the inflammation in the stomach and esophagus is treated in a timely manner. Symptoms of the disease cannot be ignored, since complications that appear as a result of the progression of pathological changes can disrupt the usual way of life.
Symptoms of reflux disease
The main symptom of GERD is heartburn, the second most common manifestation is pain behind the sternum, which radiates (gives) to the interscapular region, neck, lower jaw, left half of the chest and can simulate angina. Unlike angina, pain with GERD is associated with food intake, body position and is relieved by taking alkaline mineral waters, soda or antacids. Pain can also occur in the back, in which case it is often considered a symptom of spinal disorders.