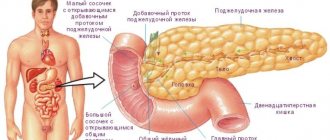
The pancreas (pancreas) is a vital organ of the human body, which simultaneously belongs to two different systems. On the one hand, it produces hormones involved in the processes of food digestion, and on the other, it is responsible for the synthesis of insulin, therefore it relates not only to the digestive system, but also to the endocrine system.
Diseases of the pancreas can be very diverse, ranging from classic inflammation to diabetes mellitus. Pathological processes are characterized by a long course and high risks of complications. They often end in death. What is the treatment for pancreas? This will be discussed in our article.
Causes
There are many reasons for exacerbation of the pancreas. However, more often exacerbation of pancreatitis occurs as a result of:
- alcohol abuse;
- diet disorders;
- taking certain medications;
- poisoning;
- exacerbation of cholelithiasis;
- stress and strong feelings;
- acute infections.
Even a single consumption of alcoholic or low-alcohol drinks can provoke an exacerbation of chronic pancreatitis.
During an exacerbation of the pancreas, the activity of enzymes increases, under the influence of which the tissue and walls of the diseased organ are irritated, swelling and severe pain occur in the abdominal cavity.
Sometimes eliminating provoking factors helps to quickly cope with an attack of pancreatitis, but an aggressive form of inflammation of the pancreas can only be treated in a hospital setting.
Antisecretory drugs
This group of drugs is used for increased secretory function of the stomach. Without them, treatment of pancreatic inflammation becomes difficult. Lack of treatment can contribute to the development of a neoplasm in the pancreas, which can only be surgically removed. Timely prescribed drug treatment will avoid complications and achieve a quick recovery.
The most popular medications for treating pancreatitis are PPIs and histamine H-2 blockers. The list of PPIs includes the following drug names:
- Omeprazole,
- Lansoprazole,
- Pantoprazole,
- Rabeprazole.
GBRs are also highly effective; their list includes drugs such as:
- Cimetidine,
- Famotidine,
- Nizatidine,
- Ranitidine.
Histamine H-2 blockers are used only in cases of severe pain; the use of PPIs is preferable.
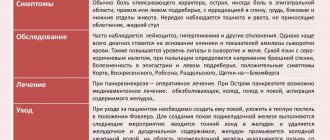
Signs
Symptoms of exacerbation of the pancreas can be confused with signs of other diseases of the digestive system, but it is impossible not to notice them. The patient experiences severe abdominal pain, diarrhea and vomiting begin, which are difficult to stop.
The most characteristic signs of pancreatitis are:
- sharp pain on the left, radiating to the back or shoulder blade;
- diarrhea;
- nausea and vomiting;
- bitterness in the mouth;
- fever, shortness of breath and chills;
- weight loss.
The most dangerous and serious symptom is an increase in body temperature to critical levels, which is accompanied by chills. This symptom most often indicates the secondary development of inflammation, which often ends in internal bleeding.
Bloating, changes in stool, abdominal pain are the first symptoms of an exacerbation of the pancreas
How long does an exacerbation of chronic pancreatitis last?
The chronic form of pancreatic disease is characterized by a long period of exacerbation. Typically, the exacerbation period lasts from 5 to 7 days, but in the case of severe pathology, the duration of the acute phase can be 10–14 days.
The long period of exacerbation is explained by the inability of the pancreas to quickly restore damaged tissue and impaired functions. That is why, at the first signs of the disease, the patient needs to consult a doctor.
If an exacerbation of the pancreas is not treated in time, the chronic form of the disease may turn into a recurrent one, which means that periods of exacerbation will become more frequent and protracted.
Treatment
Therapy for pancreatic diseases has several directions:
- Relieving pain attacks,
- Normalization of the digestive system and enzyme production, restoration of intestinal microflora,
- Getting rid of endocrine insufficiency.
Drugs for the treatment of pancreas are divided into several categories:
- antispasmodics and analgesics;
- enzymes;
- antacids;
- antisecretory drugs;
- herbal remedies.
To understand their effect, it is worth considering each of them separately.
Antispasmodics and analgesics

Due to the fact that the most basic symptom of a disease of this organ is pain, doctors often prescribe medications to patients that help alleviate the condition and remove unpleasant symptoms. The list of such medicines includes:
- Analgesics – Baralgin, Analgin.
- Antispasmodics – Nosh-pa, Drotaverine, Atropine.
These are medications that relieve organ spasms and reduce acute pain.
When pain occurs, doctors first use remedies that can eliminate it. Sometimes it is necessary to use narcotic analgesics, such as Promedol or Tramal. These drugs are used for severe pain that cannot be relieved with other drugs.
Nonsteroidal anti-inflammatory drugs are not used as painkillers. Diclofenac and Ibuprofen have an irritating effect on the gastric mucosa, which can provoke an exacerbation of the disease.
All analgesics for pain in the pancreas are allowed to be taken only as prescribed by a doctor. Self-therapy can hide the symptoms of an incipient disease.
Enzymes
When the patient's condition improves enough that he is able to eat, doctors prescribe medications containing special enzymes. The use of such drugs leads to the following:
- due to the fact that enzymes come additionally from outside, the load on the inflamed organ is reduced,
- thanks to these medications, the absorption of carbohydrates and proteins occurs quickly and without complications,
- the digestive process is normalized,
- symptoms of dyspepsia are relieved.
These drugs are divided into two groups:
- Medicines containing only enzymes. These include Pancreatin, Mezim. The products have a beneficial and restorative effect on the pancreas. Taking such medications helps improve appetite, normalize intestinal function, and get rid of nausea and gases. However, they cannot be used for a long time to avoid worsening the malfunction of the organ.
- Medicines containing bile in addition to enzymes. This is Festal, Enzyme. The drugs have an excellent therapeutic effect, but are prohibited for use in case of pancreatitis, along with which the patient is diagnosed with gastritis, cholelithiasis, and ulcers.
Enzyme preparations are prescribed strictly individually, taking into account the patient’s diet.
In rare cases, anti-enzyme drugs may be prescribed. These are agents that reduce the activity of enzymes that destroy protein. Most often used for acute pancreatitis, when an excessive amount of enzymes begins to destroy the protein of the gland itself. Such drugs include Contrikal, Ingitril, Pantripin.
Antacids
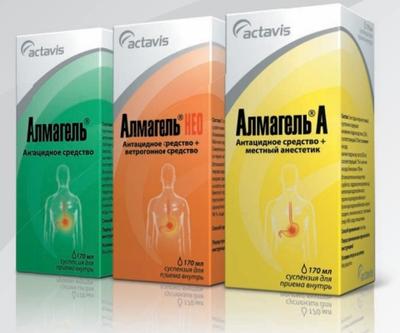
To treat pancreatic diseases, specialists often use antacid medications. Their action is that they neutralize hydrochloric acid that forms in the stomach. In this case, there will be no irritation of the mucous membrane. Such drugs include:
- Almagel, Phosphalugel, Maalox. Create a protective film on the gastric mucosa. Reduces acidity, reduces the destruction of enzymes. They contain magnesium and aluminum, adsorb pepsin and bile acids.
- Hilak Forte. Smecta will help cope with intestinal problems and restore its function.
- In case of intoxication, drugs such as Enterosgel and activated carbon help.
Thanks to such medications, the pancreas remains at rest, which has a beneficial effect on its recovery. During therapy, antacids must be combined with secretion inhibitors.
Antisecretory drugs
These medications include H2 blockers - Ranitidine, Famotidine. The action of these medications is aimed at suppressing the production of hydrochloric acid in the stomach. These also include:
- Omez and its cheaper analogue Omeprazole. It is considered a fairly important drug in the treatment of the pancreas, it reduces even severe pain symptoms and eliminates heartburn.
- Gastrozole is an analogue of Omeprazole with similar properties.
- Acidex is a drug used for many diseases of the digestive system, including increased secretion of gastric juice.
Experts also advise drinking more alkaline mineral water. It also helps normalize the condition of the stomach.
Diagnostics
The condition of the pancreas, the degree of damage to its tissues and functions are determined using a variety of research methods. In particular, the patient is prescribed:
- general blood and urine analysis;
- Ultrasound of the abdominal organs;
- gastroscopy;
- magnetic resonance imaging.

Correctly diagnosing an exacerbation of the pancreas is possible only through the integrated use of various research methods
Which doctor should I contact?
There are clear signs of acute pancreatitis that indicate the need for specialist help. These include the following:
- sharp girdle pain in the umbilical region, which begins in the left side. There may also be a stabbing or cutting pain in the right upper abdomen. The pain syndrome intensifies when lying on your back, as well as when consuming food and alcoholic beverages;
- vomiting with bile secretions;
- temperature increase;
- flatulence;
- diarrhea with impurities of undigested food.
Important! In case of an acute attack of the disease, an ambulance should be called.
When the first alarming symptoms appear, you should consult a therapist. This specialist is responsible for ordering initial examinations, making a diagnosis and finding out its cause. First of all, the doctor must collect anamnestic data.
He is interested in when and after what unpleasant symptoms appeared. It is also important for him to clarify the clinical picture of the pathology. An important role is also played by the identification of concomitant diseases, for example, disorders of the liver, stomach, and duodenum.

When the first symptoms of pancreatic disease appear, you should consult a physician.
To assess the nature of the pancreatic disease, the following examinations are carried out:
Drugs for the treatment of pancreas
- general tests. This includes blood and urine testing, as well as an electrocardiogram. A study of heart function helps differentiate from diseases such as heart attack and angina pectoris;
- ·biochemical tests (enzymes, total protein, glucose);
- coprogram. Stool examination may reveal the presence of undigested fibers and fat droplets;
- Ultrasound of the abdominal organs can show structural abnormalities, as well as the presence of cysts and tumor processes;
- endoscopy of the stomach.
In the presence of chronic pancreatitis, digestive disorders and concomitant pathologies of the gastrointestinal tract (GIT), the therapist refers the patient to a gastroenterologist. A specialist will help you develop the right diet, as well as select the right dose of enzymatic agents.
Sometimes destructive processes in the pancreas affect the islet apparatus, which produces hormones. In this case, you will need the help of an endocrinologist. Your doctor may prescribe hormone replacement therapy. Patients with diabetes mellitus are registered at the dispensary and their condition is monitored. Inpatient therapy in endocrinology may be required.
Attention! Symptoms of liver disease may be similar to manifestations of pyelonephritis, osteochondrosis, and herpes zoster. A qualified specialist can make an accurate diagnosis.
If treatment involves surgery, then you cannot do without consulting a surgeon. His help will also be required if acute pancreatitis is detected. Surgical intervention may also be required if gland ducts are blocked by stones for drainage, cysts, tumors, or the need to remove part of the organ.
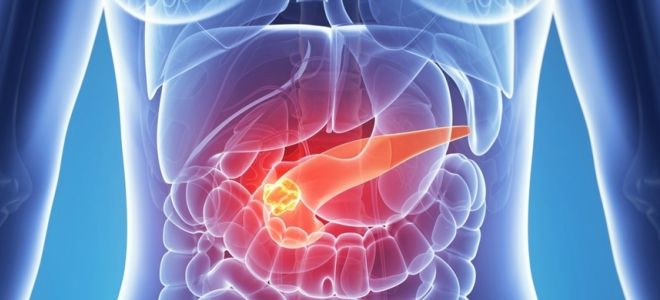
Advanced forms of pathological processes in the pancreas can cause the development of tumor processes. To confirm the diagnosis, CT, MRI, or ultrasound may be required. In such a development of the situation, a consultation with an oncologist will be required.
What to do in case of exacerbation?
In the case of an acute and rapid relapse of the disease, intense pain occurs, which has an increasing character. The result of severe pain can be loss of consciousness and painful shock, so the person needs urgent hospitalization.
What to do if there is an exacerbation of the pancreas?
- Provide the patient with complete rest. A person experiencing pain is recommended to take a semi-sitting or semi-lying position. This will help reduce blood flow to the diseased organ, and therefore slow down the development of the inflammatory process.
- Do not eat food. For three days, it is best for the patient to refrain from eating any foods. This will help reduce enzyme production.
- Apply cold to the diseased organ. A cold heating pad or ice will help relieve swelling and pain.
- Take antispasmodics.

Hunger, rest and cold are the main conditions for relieving exacerbation of pancreatitis
Pancreatic diseases
This organ is considered one of the most important in the digestive system. A disruption in its functioning is felt throughout the entire body. It provokes dysfunction of neighboring organs. Here are the most common pancreatic diseases:
- Pancreatitis
is a disease that can occur in acute and chronic forms. In the first type of course, inflammation and destruction of pancreatic tissue is observed. - Oncological disease
- cancer at the initial stage may be accompanied by nonspecific symptoms. In the active stage, the tumor grows rapidly. As the disease progresses, the patient experiences "cancer wasting." As the tumor grows, nearby organs are compressed. Education can grow in them, which causes a malfunction in their work. - Cysts on the pancreas
- formations can be localized in any area of this organ, but more often they are found on the body and tail. If the capsules are small in size (less than 5 cm), they do not cause discomfort to the patient. Larger cysts can cause pain, fever and rapid weight loss. - Stones in the pancreas
are formed both in the parenchyma and in the ducts. More often, calcifications appear after pancreatitis. - Diabetes mellitus
- due to dysfunction of the gland, the organ produces insufficient amounts of insulin. As a result, this causes the development of this disease.
How to treat?
For the treatment of the acute phase of pancreatitis, which is carried out in a hospital setting, a whole range of medications is used.
The main task of drug therapy:
- relieve pain;
- restore pancreatic function;
- eliminate concomitant diseases.
For this purpose, it is advisable to use the following drugs:
Antispasmodics
Pancreatitis and diabetes mellitus
The key symptom of an attack of pancreatitis is pain. Sometimes the pain is so severe that it is impossible to bear. Drugs from the group of antispasmodics, which have a vasodilator and myotropic effect, will help alleviate a person’s condition.
To quickly relieve pain during acute pancreatitis, it is best to use injectable antispasmodics. For example, it could be No-shpa or Papaverine. These medications have minimal side effects. When these drugs are administered intravenously, their effect begins instantly, which is very important for the psychological state of the patient, for whom every second is filled with severe pain.
However, both Papaverine and No-shpa have a relatively short duration of action. Platiphylline will help relieve severe pain for a longer period, however, compared to other antispasmodic drugs, it has many more contraindications and side effects.
In case of painful shock, narcotic painkillers are used.
How to relieve pain from pancreatitis
First of all, you need to remember: in this case, the patient should be given complete rest, and he also needs a “starvation” diet.
Sometimes, if only these conditions are met, it is possible to achieve a significant reduction in pain. Also read: Treatment of pancreatitis with folk remedies - the most effective
It is allowed to drink mineral water (alkaline, still). Apply cold (ice pack) to the abdominal area.
Pancreatitis has worsened - the pain can be relieved with painkillers, which are administered by injection; tablet forms are excluded. This is explained by the fact that this pathology is accompanied by nausea and often vomiting, as a result of which the drugs do not have time to be absorbed by the body and do not have the desired effect. Taking enzymes in the acute period is strictly prohibited.
As a rule, painkillers are prescribed by a doctor, and only in complex treatment, which implies:
- restoration of water-salt balance;
- decreased activity and production of pancreatic enzymes;
- suppression of infection.
Important! You should not take painkillers for pancreatitis on your own, without medical advice, because by eliminating the pain syndrome, you will “veil” the symptoms of the disease. This will make it difficult to diagnose.
To the question: is it possible to cure a stomach or duodenal ulcer at home, a gastroenterologist, head of the gastroenterology department, Mikhail Vasilievich Arkhipov, answers.
Nutrition for exacerbation of the pancreas
The main condition for eliminating unpleasant symptoms during exacerbation of the pancreas is following a diet. As a rule, patients are assigned table No. 5.
The patient is allowed to eat foods rich in protein (lean meats and fish), eat pureed cereals, drink tea, and rosehip decoction. All dishes should be steamed and served to the patient pureed or chopped.

Diet and proper nutrition are the main conditions for successful treatment of pancreatic inflammation and its prevention
The list of prohibited foods that should not be consumed during exacerbation of pancreatitis includes:
- smoked meats, sausages;
- canned food;
- strong meat broths;
- hot seasonings, sauces and spices;
- mushrooms;
- cocoa, coffee, carbonated drinks;
- fatty dairy products (cottage cheese, sour cream, cream);
- fast food (nuts, chips, pistachios).
Despite the wide list of prohibitions, the patient’s menu should be varied and balanced, i.e. it should include not only porridge, but also low-fat varieties of fish and meat rich in protein and vitamins.
In case of an acute attack of pancreatitis, patients may be given a three-day fast, during which they are allowed to drink only still water.
Diet
Treatment of the pancreas during an exacerbation is a long process, during which not only doctors must make efforts to stabilize the patient’s condition, but also the patient himself.
In the acute period, it is forbidden to consume any foods until the excessive secretion of enzymes ends. How long this period will last depends on the treatment and the patient’s endurance.
Patients with this pathology are overweight or alcohol dependent, which is why they often relapse. If you break your diet in the first days of treatment, the consequences will be more dangerous than the severity of the previous attack.
It is impossible to completely cure chronic pancreatitis - it is a permanent lifelong condition, but maintaining normal metabolism is possible if you correctly follow all doctor’s prescriptions.
Traditional treatment
There is an opinion that pancreatitis can be cured at home using folk remedies. However, modern gastroenterologists insist that the use of various herbal preparations and medicinal plants can be beneficial and improve the functions of the pancreas only with chronic pancreatitis in remission. Using such means in the acute phase is sometimes not only useless, but also dangerous.

By experimenting with various herbal decoctions and infusions during an exacerbation of the pancreas, you can lose precious time and miss the chance to quickly restore all the functions of the diseased organ
However, as modern experts note, traditional methods can be used to eliminate associated symptoms. So, to activate the outflow of bile and normalize liver functions, you can use corn silk, rose hips, and immortelle. And to improve the psychological state of the patient, decoctions of chamomile, linden and mint are excellent.
What medications should be used to treat the pancreas?
Drug therapy helps to simultaneously cope with the following tasks:
- relieve pain;
- restore microflora and improve the functioning of the digestive system;
- compensate for enzymatic deficiency.
Medicines for the treatment of the pancreas will help to cope with all this. They should only be prescribed by a doctor: self-medication can worsen the situation. An integrated approach is important in therapy. The following medicinal and non-medicinal agents can be used in treatment:
- pills;
- injections;
- Dietary supplements.
What tablets should be used to treat the pancreas?

During therapy, medications with different effects can be used. If the pancreas is inflamed, how to treat it - what pills:
- Papaverine;
- No-Shpa;
- Atropine;
- Platyfillin;
- Gastrocepin.
All these medications are antispasmodics. They help relieve pain. Antacids may be prescribed at the same time. These drugs reduce the acidity of gastric juice, which provides the pancreas with functional rest and helps it recover faster. The following medications are most often prescribed:
- Maalox;
- Almagel;
- Phosphalugel;
- Omez;
- Zoran;
- Pepsidil;
- Ocid.
The doctor knows how to treat the pancreas with tablets, so he will definitely prescribe enzyme agents. This group of drugs does not restore organ function. They deliver enzymes, thereby normalizing the digestion process. The following drugs are most often prescribed:
- Creon;
- Mezim;
- Pangrol;
- Enzistal;
- Pancreatin;
- Festal.
Antibiotics have proven themselves to be effective in treating inflammation of the pancreas. Such drugs prevent the development of possible complications. The most commonly prescribed antibiotics are:
- Vancomycin;
- Abaktal;
- Ceftriaxone.
In complex therapy, medications can be prescribed to help get rid of the following negative symptoms:
- for diarrhea - Smecta and Hilak;
- if intestinal motor function is impaired - Trimedat;
- for intoxication - Enterosgel.
Injections for the treatment of the pancreas

For acute pain, the following injections may be prescribed:
- Atropine (1 ml subcutaneously);
- Analgin (1 ml intramuscularly);
- Papaverine (2 ml intramuscularly).
Before treating the pancreas at home, you need to consult a doctor. If the inflammatory process worsens, he may prescribe the following injections:
- Baralgin;
- Paracetamol.
More often, the following antihistamines are prescribed simultaneously with antispasmodics:
- Diphenhydramine;
- Tavegil;
- Suprastin.
Dietary supplements for the treatment of pancreas
The domestic market offers a huge variety of supplements that help normalize the functioning of the gastrointestinal tract. Before treating your pancreas at home with these pills, it is important to consult your doctor. He will help you choose the best option and prescribe the right dosage. The following dietary supplements are especially popular:
- Evalar;
- Siberian Health;
- Tianshi;
- Vision.
Prevention
To prevent exacerbation of chronic pancreatitis, gastroenterologists recommend:
- follow diet No. 5;
- completely stop drinking alcohol;
- undergo regular examinations and visit a doctor;
- lead a healthy lifestyle;
- control cholesterol and blood sugar levels;
- take enzyme preparations prescribed by your doctor;
- eliminate the toxic effects on the body of uncontrolled use of medications;
- carry out treatment in sanatoriums of the appropriate profile.