Definition and disease code according to ICD-10
With the disease, the death of organ cells is noted due to a strong inflammatory process.
During the development of the disease, defense mechanisms are disrupted. The pancreas begins to digest itself. With this disease, there is a high probability of disruption of the functioning of other organs or systems.
Photo of pancreatic necrosis of the pancreas
The disease code according to ICD-10 is K86.8.1. Pancreatic necrosis develops in three stages:
- At the first stage, bacterial toxins are formed. However, blood tests do not always show the presence of pathogenic microflora.
- In the second stage, an abscess appears. It affects neighboring organs. This stage occurs in the absence of treatment.
- The third stage - purulent processes are formed in the organ itself and in the retroperitoneal tissue. At this stage, there is a high probability of death.
General information about the disease
Chronic pancreatitis is a multifactorial disease that manifests itself with periods of remission and exacerbations. During remission, the clinic is erased, and the pain feels relatively satisfactory.
During exacerbations of life, the patient is at risk of multiple organ failure, which occurs due to the release of many enzymes into the abdominal cavity.
Mortality increases with age and the presence of comorbidities. Risk factors for complications of pancreatitis with necrosis:
- Elderly age;
- Chronic alcoholism, drug addiction;
- Female gender (more often affects postmenopausal women);
- Reduced general resistance of the body (with chronic concomitant diseases, organ failure);
- Late diagnosis, incorrect assessment of the patient’s condition, development of peritonitis, sepsis, shock.
The prognosis improves if organ death is diagnosed in a timely manner and correct treatment is carried out.

Stages of development of acute pancreatitis
Reasons for development
One of the main reasons is an unbalanced diet and occasional alcohol consumption. Studies have shown that alcoholism does not cause this serious illness, but in most cases it begins with an episode of drinking.
People with alcoholism often develop pancreatitis, which is rarely complicated by necrosis of the pancreas.
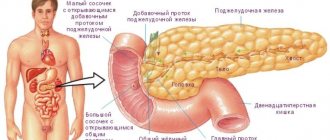
The underlying cause of the disease is a violation of local defense mechanisms. Too much food and drink leads to increased secretion and increased flow. As a result, the outflow of pancreatic juice is disrupted. This provoking factor is called obstructive.
The reflex factor includes the reflux of bile from the duodenum into the pancreas. This activates proenzymes. Typically, in this case, the cause is surgical complications, blunt abdominal trauma, and various endoscopic manipulations.
The risk group includes the following groups of patients:
- with stones in the organ,
- liver failure,
- abnormalities of the pancreas,
- diseases of the digestive tract.
Why does acute pancreatic necrosis occur?
The following factors lead to the development of pancreatic necrosis:
- Food poisoning and severe alcohol intoxication.
- Unsuccessful surgery.
- Organ injuries that contribute to the release of enzymes and destruction of the organ.
- Chronic type of pancreatitis, because the gland tissue has already undergone changes. The situation is aggravated by the patient’s refusal to diet and consumption of sour, salty and fatty foods.
- Autoimmune and viral diseases. In this case, organ damage is a complication.
- Pathologies of the gallbladder and liver: narrowing of the bile ducts, formation of stones, inflammation of the ducts as a result of the penetration of bacteria.
- Genetic disorders: anomalies of organ structure, cystic fibrosis.
These factors indicate that the following people are at risk:
- Alcohol abusers.
- Suffering from diseases of the gastrointestinal tract.
- Having a history of cholelithiasis.
- Taking drugs.
- Having a history of congenital malformations of the digestive system.
Classification
There are two main groups of the disease:
- Total.
- Infected.
Total
Refers to a severe degree of the disease. It affects up to 100% of the retroperitoneal tissue. The patient's condition constantly worsens over 1-3 days, even with therapy. In addition to progressive necrosis, signs of the onset of multiple organ failure and pancreatogenic shock are added.
A blood test reveals an increase in leukocytes and pancreatic enzymes. The death of gland cells occurs without the possibility of recovery.
Infected
Develops in 40-70% of patients with TOP. Microflora enters the zone of changes from the large intestine. The disease is suspected if health continues to deteriorate 7 days after the start of TOP.
The peak of the disease occurs on days 10-14. The necrotic lesion moves beyond the organ to the omentum and other organs.
Gradually, tissue breakdown products and sepsis lead to poisoning of the entire body, as well as systemic inflammation. The patient goes into shock, which ends in death.
Etiology
List of diseases that can cause the development of pancreatic necrosis:
- Chronic pancreatitis of various etiologies, evolution and stages;
- Long-term diabetes mellitus, with the development of total insulin deficiency and dependence on exogenous insulin;
- Acute intoxication, in particular alcohol poisoning, can occur with a single use or due to prolonged abuse;
- Infections that cause bacteria to migrate through the bloodstream (septicemia);
- Sepsis and multiple organ failure;
- Trauma to the organ, release of enzymes beyond the gland and the development of autodigestion.
It is worth understanding that all of the above reasons in themselves are serious pathologies that lead to life-threatening complications, pancreatic necrosis is one of them.
Kinds
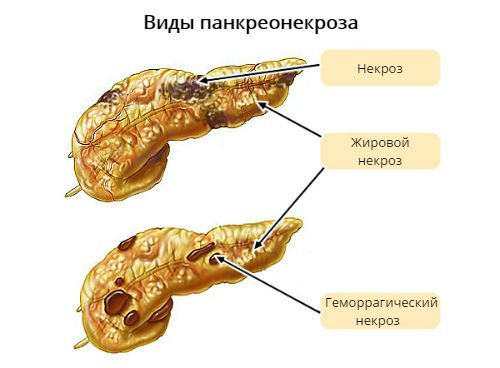
The following types are distinguished:
- fatty,
- hemorrhagic,
- mixed.
Fatty
As the disease develops, metabolic processes and the normal functioning of pancreatic cells fail. There may be a sharp drop in blood pressure.
The disease is characterized by the rapid formation of an inflammatory infiltrate. If the disease is recurrent in nature, then such a focus may appear later. This form is formed with the participation of lipase.
This type of disease progresses slowly. Peripancreatic tissues are gradually involved in the inflammatory process. Patients with this form show fluctuations in alpha-amylase, but changes in its amount do not play a role in the pathological process itself.
Hemorrhagic
With this form, an irreversible process of cell death occurs. The form occurs during acute pancreatitis or develops during exacerbation of the chronic form.
The disease necessarily affects the secretory part of the pancreas. Its cells produce cells that are part of pancreatic juice.
The hemorrhagic form develops due to the aggressive effects of trypsin and some other enzymes that break down protein molecules.
The cause of the development of the disease may be a complex humoral process of regulation and production of digestive enzymes.
Mixed
This form is characterized by signs of several types of necrosis. Under the influence of negative factors, a sharp stimulation of the production of pancreatic juice begins. The ducts can no longer cope with the load, so the juice begins to concentrate.
Young people and middle-aged people are more prone to the disease. The mixed type does not appear at first. When symptoms appear, we are talking about the active phase.
Classification and main signs of pathology
Tissue necrosis, which began in the pancreas due to the digestion of its own cells by digestive enzymes, occurs for the first few days (usually about a week) without the presence of infectious agents. At this time, when no obvious destruction is observed in the pancreas, the patient is diagnosed with sterile, or, as it is also called, aseptic pancreatic necrosis. But then pathogenic microflora begins to join the pathological process.
It infects the gland, which provokes the movement of the necrotic lesion to other intraperitoneal anatomical structures and organs of the abdominal cavity (surrounding tissue, omentum, and so on). According to the degree of the destruction process, the place of their localization and the characteristics of the course of the pathology, the following forms of pancreatic necrosis are distinguished:
- In terms of its prevalence, the destructive process can be local, that is, small-focal, spreading exclusively to one anatomical region of a given organ (body, head or tail). A diffuse type of pathology, which includes total pancreatic necrosis, is often noted. With this type of scourge, necrotic changes affect the entire organ, both tissues and secretory ducts, and, directly, the walls of the blood vessels that penetrate the gland.
- According to the characteristics of the course, fatty pancreatic necrosis is distinguished, the main role in the development of which is given to the activation of lipase, an enzyme that accelerates the breakdown of fats. This type of pathology is characterized by a very slow course. In second place in the rate of development is the hemorrhagic form of pathology, the occurrence of which is responsible for protease enzymes that have a direct effect on protein structures.
If infected pancreatic necrosis of the pancreas is diagnosed, surgery becomes inevitable, since the prognosis of this form of the disease is extremely unfavorable and very often leads to disability or death due to the development of toxic shock.
But in most cases it is impossible to ensure that the disease completely subsides. The negative prognosis is due to the fact that necrotic lesions often begin to develop again.
Symptoms
Pancreatic necrosis has a pronounced clinical picture, so it is difficult to confuse it with another pathology. Symptoms include:
- Pain. It arises in the left side of the abdomen and radiates to the shoulder, back, groin and chest. The patient cannot describe the localization of sensations. The intensity of the pain depends on the severity of the disease.
- Nausea and vomiting. Immediately after the pain, vomiting appears, which is not associated with food intake. It doesn't bring relief. In addition to bile, the vomit contains blood clots.
- Dehydration. Since vomiting is very difficult to stop, it causes dehydration. The skin and mucous membranes become dry, diuresis decreases.
- Bloating. Since the pancreas ceases to function, the processes of rotting and fermentation intensify in the intestines. This leads to increased gas formation and bloating.
- Intoxication. Bacterial toxins circulating in the bloodstream lead to an increase in body temperature. General weakness appears, heartbeat increases.
- Paleness of the skin. At the first stage, vasoactive substances appear in the blood, which is manifested by redness of the dermis. When intoxicated, the skin turns pale, gray or jaundiced.
What is pancreatic necrosis? Symptoms and treatment
Subscribe to the
YandexZen
channel Pancreatic necrosis: what is it, for what reasons does it develop, what clinical signs and treatment methods does it have? These questions are asked by everyone who has been diagnosed with this disease. What do you need to know about the condition and how to prevent the development of serious complications?
But before we start, please like and subscribe to the channel. Thank you!
Pancreatic necrosis - what is it?
Pancreatic necrosis is a destructive pathology of the pancreas.
, which develops as a particularly severe complication of acute pancreatitis.
The condition leads to dysfunction or complete cessation of function of two or more organ systems in the human body.
During the development of the disease, rapid death of tissues and cells of the gland occurs, which is accompanied by inflammation.
As a result, the pancreas is destroyed and ceases to function, which is accompanied by severe clinical manifestations.
Classification of pancreatic necrosis
Depending on the prevalence of the destructive process, pancreatic necrosis is divided into:
- limited (small-focal, medium-focal and large-focal);
- widespread (subtotal, in which 75-90% of the pancreas is affected (polynecrosis) and total, in which the entire pancreas is destroyed).
According to the course of the disease there are:
Abortive pancreatic necrosis
A distinctive feature of this form of pancreatic necrosis is interstitial edema that develops around the destroyed cells. The process is accompanied by hyperthermia and inflammation. Treatment of this form is carried out with medication.
Progressive pancreatic necrosis
Enzymes produced by the pancreas, coming from the intermediate lymph and bloodstream, have a negative effect on the tissue. The following changes occur sequentially in the body:
- physical inactivity;
- development of pancreatogenic shock;
- development of functional failure of parenchymal organs;
- complications of a purulent and post-necrotic nature.
Recurrent pancreatic necrosis
The disease is typical for patients aged 35-45 years, mainly men, but can be observed in people of all ages who abuse alcoholic beverages. This form is an acute pathology that occurs as a result of various chronic processes.
Fulminant pancreatic necrosis.
An instantly developing form of the disease. Rapid intoxication of the body occurs and pancreatic shock develops. In 90% of cases, the chances of survival are 5-10%.
Depending on the presence of infectious agents in the organ, the disease is divided into:
- sterile;
- infected.
Sterile pencric necrosis is divided into 3 forms:
- Fatty pancreatic necrosis, which is characterized by an inflammatory process and the rapid formation of an infiltrate. The pancreas enlarges, its surface becomes tuberous and has gray-yellow necrotic foci, sometimes interconnected. Cells are a mass without a specific structure; they are not differentiated during examination. Fluid may accumulate in the peritoneal cavity. After the intensity of the inflammatory process decreases, a connective tissue capsule forms around the foci of necrosis.
- Hemorrhagic pancreatic necrosis. The most severe form of pancreatic necrosis, which is characterized by rapid development and accompanying internal bleeding. With this form, irreversible death of tissues and cells of the gland is observed. The development of hemorrhagic necrosis is associated with the negative effects of the main pancreatic enzymes. The organ gradually enlarges and acquires a dark red color with a blue-black tint. Hemorrhagic necrosis is large-focal, in which 2 or more parts of the organ are involved in the process.
- Mixed form of pancreatic necrosis.
Mechanism of development of pancreatic necrosis
The initial stage of pancreatic necrosis can be judged long before the first clinical signs appear.
The development of pathology occurs in 3 stages:
- Toxemia. After the influence of the provoking factor on the gland, increased secretion of the organ and stretching of the gland ducts are observed. As a result, the pressure in it increases and the process of death begins. In other words, the gland begins to digest itself. When lipase is activated, fat cells undergo necrosis (fatty paranecrosis). When elastase is activated, destruction of blood vessels (hemorrhagic necrosis) is observed.
- Abscess. At this stage, inflammation of the gland develops, which further spreads to neighboring organs, forming purulent cavities.
- Formation of purulent foci. The final stage of pathology development, upon reaching which a favorable prognosis is unlikely.
Reasons for development
The development of pathology is a consequence of:
- chronic alcoholism or excessive consumption of alcoholic beverages;
- peptic ulcer of the duodenum, stomach;
- eating disorders, namely regular overeating;
- infectious and viral diseases;
- cholelithiasis;
- previous operations;
- cancer;
- abdominal trauma.
Symptoms of pancreatic necrosis
The symptoms of pancreosis are almost impossible to confuse with the manifestations of other diseases.
The disease is characterized by pain, nausea, vomiting, dehydration, increased gas formation, signs of general intoxication, and changes in skin color.
Pain in pancreatic necrosis is a cardinal symptom.
Pain is felt in the left side of the abdomen, radiating to the back, groin, shoulder and chest. As a rule, the patient cannot clearly indicate where the pain syndrome is localized and describes it as shingles. The intensity depends on the course of pancreatic necrosis.
The more destruction has occurred in the body, the less intense the pain a person feels (due to the death of nerve endings in the organ).
After the onset of pain, a person begins to vomit profusely, uncontrollably, which has no connection with food intake and does not alleviate the patient’s condition. The vomit consists only of bile mixed with blood.
Vomiting that cannot be controlled leads to dehydration. Signs of dehydration in pancreas pathology are constant thirst, dry skin and mucous membranes, the formation of plaque on the tongue, urination becomes rare and scanty (often the urine is very dark) until urination completely stops.
Toxins that circulate in the bloodstream lead to rapid poisoning of the entire body. Intoxication manifests itself as weakness, heart rate increases, breathing becomes shallow, and blood pressure decreases significantly. The temperature during intoxication reaches subfebrile values. Exposure to toxins in the brain leads to the development of encephalopathy.
With minor intoxication, the pancreas releases substances into the blood that dilate blood vessels, which promotes hyperemia (reddening of the skin). Further, when the influence of toxic substances is pronounced, the skin turns pale and cold. Sometimes hematomas appear throughout the body.
Prognosis after surgery
With timely treatment, the mortality rate of patients is slightly less than 50%; with the treatment of severe forms, the mortality rate reaches 95%.
Let's like and subscribe to the channel. Thank you for your attention!
You may also be interested in:
What is chronic pancreatitis? Symptoms and treatment
What is superficial gastroduodenitis?
What are the causes of cutting pain in the lower abdomen in women?
Causes and treatment of gas formation in women
What types of intestinal diseases exist?
Source: https://zen.yandex.ru/media/id/5a7bf2178139baa694016d48/5a8a955b8139ba0d23cf85bd
Complications
Pancreatic necrosis is complicated not only by purulent processes, but also by disturbances in the functioning of other organs. The incidence of infectious complications occurs in every third patient.
The likelihood of their occurrence depends on the area of the lesion. The most life-threatening are the first three weeks of illness.
Complications include:
- shock,
- peritonitis,
- abdominal abscess,
- bleeding,
- enzyme deficiency,
- ulcers,
- thrombosis,
- fistulas
Consequences
Pancreatic necrosis can be fatal within 24 hours after the first signs appear. The prognosis of life with a fatty-type disease is determined not only by the area and extent of necrosis, but also by the size of pancreatic edema. Pancreatic necrosis can have the following consequences:
- Rupture of the bile ducts.
- Decomposition of the stomach and pancreas due to bleeding.
- Brain swelling.
- Acute lung injury.
- Intoxication of the gastrointestinal tract.
Diagnostics
Initially, the diagnosis is made based on the patient's complaints. Laboratory research methods are prescribed, which reveal:
- Increase in liver enzymes.
- Increase in C-reactive protein.
- Calcitonin in the blood.
- Increased blood sugar.
- The amount of elastase, amylastase, and trypsin in the urine increases significantly.
Plain radiography allows you to identify indirect signs of inflammation. Fistulas are visualized using a contrast agent. Additionally carried out:
- Ultrasonography. It indicates the presence of stones, enlargement and changes in the structure of the gland, and foci of necrosis are identified.
- MRI allows a more detailed assessment of pathological changes.
In the most difficult cases, laparoscopy is performed. This is the most accurate way to make a diagnosis and assess the condition of the organ and surrounding tissues.
During the diagnostic process, studies are carried out regarding intestinal obstruction and acute inflammatory diseases.
Treatment
Treatment is carried out using:
- medicines,
- surgical impact,
- diets.
During illness, any physical activity is prohibited, and therapeutic fasting is prescribed. Parenteral nutrition is prescribed using nutrients.
Medicines
Taking medications is necessary to reduce pain and eliminate the cause that led to the disease. It is necessary to prescribe medications to restore water balance.
To relieve pain, antispasmodic drugs and non-narcotic analgesics are administered. In extreme cases, it is allowed to take narcotic painkillers.
To reduce the secretory activity of the pancreatic gland, antienzyme agents and proton pump inhibitors are administered. If there is no cholelithiasis, choleretic drugs are prescribed to unload the ducts.
For aseptic necrosis and to suppress pathogenic microflora in infected cases, antibiotics are prescribed. Typically, cephalosporins with fluoroquinolones are used in combination with metronidazole.
Operations
The most effective treatment method is surgery. It allows you to remove inflammatory hemorrhagic exudate, stop bleeding and drain the retroperitoneal space.
Such treatment is possible after the acute process has stopped and the patient’s condition has stabilized.
Emergency surgical intervention is indicated for total or subtotal necrosis, as well as for the development of purulent peritonitis. If the infected destructive process affects the gland, laparotomy surgery is used, providing good access to other organs.
Often it is necessary to remove neighboring organs: gallbladder, spleen . Doctors note that sometimes repeated surgical treatment is required if the gland continues to deteriorate.
Diet for pancreatic necrosis: sample menu
In case of exacerbation of the disease, fasting is prescribed before and after surgery. To prevent exhaustion of the body, artificial nutrition is introduced. Nutrients enter directly into the blood, bypassing the gastrointestinal tract. After this, you must adhere to diet No. 5 for a week.
Immediately after the operation, you are allowed to drink tea, mineral water and rosehip decoction. If the condition is stable, after a week, foods low in calories, salt and fat are gradually introduced. Products are steamed or boiled. At the same time, they are thoroughly crushed and wiped.
As for fruits, soft varieties of apples and pears are allowed. You can eat no more than 10 grams per day. butter. You can start your morning with an omelet, but you should cook it only with protein. Crackers and cookies are allowed.
To maintain the required amount of calcium, you are allowed to eat a small amount of cottage cheese and drink low-fat milk.
Soups with mushroom, fish and meat broth are contraindicated. You will have to give up bread and other flour products. You cannot drink grape juice, coffee and cocoa. Meat, fatty fish, grapes, bananas, dates and figs are strictly prohibited.
Symptoms of pancreatic necrosis of the pancreas and methods of its treatment
Pancreatic necrosis of the pancreas is an extremely dangerous destructive disease, which in most cases develops against the background of an attack of acute pancreatitis.
This pathological condition is extremely dangerous, since even with timely comprehensive treatment there is a high risk of death.
Pancreatic necrosis of the pancreas is an extremely dangerous destructive disease, which in most cases develops against the background of an attack of acute pancreatitis.
Most often, young people from 20 to 35 years old suffer from pancreatic necrosis.
This pathological condition, even with a favorable outcome of the acute period, further reduces the duration and quality of life of the patient. The pathology affects both men and women equally.
Classification
There are several classifications of the disease. Depending on the extent of the process, pancreatic necrosis can be:
- widespread;
- limited.
In addition, pathology is divided into types depending on the presence of an infectious agent. According to this parameter, pancreatic necrosis can be:
- sterile;
- infected.
There are several classifications of the disease. Depending on the extent of the process, pancreatic necrosis can be: widespread and limited
The sterile variant of the disease is divided into 3 clinical and anatomical forms, including:
- hemorrhagic;
- fat;
- mixed.
Depending on the characteristics of the course, this disorder can be progressive and abortive.
Causes
Despite the fact that pancreatic necrosis can occur in any person under some circumstances, it affects certain categories of people more often. Predisposing factors include:
- chronic alcoholism;
- pathologies of the pancreas and liver;
- cholelithiasis;
- poor nutrition;
- chronic diseases of the gastrointestinal tract;
- long-term use of injecting drugs;
- congenital malformations.
In most cases, pancreatic necrosis occurs as a result of drinking large doses of alcohol or fatty foods. The simultaneous influence of these two factors during heavy feasts increases the risk of developing a pathological condition. This is a nutritional mechanism for the development of the disease.
Somewhat less frequently, pancreatic necrosis appears as a result of obstruction of the bile ducts. In this case, the advancement of stones leads to blockage of the ducts, which increases the pressure inside the organ and the permeability of the vascular walls. There is an early activation of enzymes produced by the pancreas, which leads to the digestion of this organ.
There is also a reflux variant of the development of pancreatic infection. In this case, bile is refluxed into the pancreas from the duodenum, resulting in a severe enzymopathic reaction.
Often, the pathological process occurs after endoscopic operations performed on the abdominal organs, after blunt trauma to the abdomen and with thrombophlebitis and vasculitis of the pancreatic vessels.
Symptoms of pancreatic necrosis of the pancreas
The clinical picture of the development of pancreatic necrosis of the pancreas is difficult to confuse with other diseases.
This pathological condition occurs in an acute form.
Patients complain of intense pain in the right hypochondrium, radiating to the shoulder, shoulder blade, groin area or chest. A person cannot accurately determine the location of unpleasant sensations.
The severity of pain directly depends on the extent of damage to the pancreas.
The clinical picture of the development of pancreatic necrosis of the pancreas is difficult to confuse with other diseases.
In most cases, the further the pathological process has advanced, the less pronounced the pain syndrome becomes, which is the result of the death of nerve fibers located in the tissues of the organ.
If the patient lies on his right side and presses his legs towards his stomach, the discomfort may become less pronounced.
Pancreatic necrosis is often accompanied by the following signs of the pathological process:
- nausea;
- vomit;
- dry skin and mucous membranes;
- bloating;
- increased gas formation;
- redness or paleness of the skin;
- gastrointestinal bleeding.
Pancreatic necrosis of the pancreas is often accompanied by nausea.
Approximately 5-9 days after the onset of the disorder, the appearance of post-necrotic and purulent complications is observed. The pancreas greatly increases in size due to ongoing inflammatory and necrotic processes.
First aid
If symptoms of a pathological condition appear, it is necessary to call emergency doctors, since therapy for pancreatic necrosis should be carried out in a hospital setting.
Before doctors arrive, it is necessary to measure the patient’s temperature and blood pressure. A heating pad with cold water should be applied to the area of the right hypochondrium. A person needs to be provided with complete rest, because...
sudden movements can worsen the condition. You need to open the windows to allow air flow.
If symptoms of a pathological condition appear, it is necessary to call emergency doctors, since therapy for pancreatic necrosis should be carried out in a hospital setting.
The patient should breathe shallowly without taking sharp breaths. This will reduce the intensity of pain.
It is advisable to perform a gastric lavage and an enema to free the rectum from feces. The patient should completely refuse food. Water can be consumed in small portions not exceeding 50 ml. To reduce the intensity of pain, you can use No-shpu, Papaverine and Drotaverine.
It is better not to use other medications until doctors arrive.
Diagnostics
When a characteristic clinical picture of this pathological condition appears, the patient requires urgent consultation with a gastroenterologist. To make a diagnosis, the doctor conducts an external examination, collects an anamnesis and prescribes the following studies:
- general and biochemical blood tests;
- determination of liver enzyme levels;
- Ultrasound of the pancreas;
- CT;
- MRI;
- vascular angiography;
- retrograde cholangiopancreatography.
To make a diagnosis, the doctor conducts an external examination, collects an anamnesis and prescribes an ultrasound.
Diagnostic laparoscopy may be indicated to determine the nature of the damage to the gland in the tail, body or head.
Treatment of pancreatic necrosis
In most cases, therapy is carried out using conservative methods. The patient requires hospitalization and adherence to a gentle diet throughout the entire period of the acute course of the pathology.
To relieve the manifestations of pancreatic necrosis, drug therapy is prescribed.
In cases where conservative therapy does not achieve significant improvement, doctors may prescribe surgical intervention to eliminate the focus of necrotic tissue damage and sanitation of abscesses.
The patient requires hospitalization and adherence to a gentle diet throughout the entire period of the acute course of the pathology.
Diet
During the first 3-10 days after the onset of an acute attack of pancreatic necrosis, the patient is prescribed therapeutic fasting. After this, the patient must follow diet No. 5b according to Pevzner. Allowed products and dishes include:
During the first 3-10 days after the onset of an acute attack of pancreatic necrosis, the patient is prescribed therapeutic fasting. After this, the patient must follow diet No. 5b according to Pevzner.
It is necessary to completely exclude fresh bread and baked goods, canned food, sausages and semi-finished products from the diet. In addition, you should not consume strong meat and mushroom broths, dishes with a high content of spices, fast food, pickles, marinades and sweets.
Medication
To eliminate the inflammatory process and symptomatic manifestations, drugs belonging to the following groups are prescribed:
Directed detoxification treatment is required. For this purpose, infusion therapy is prescribed. In addition, peritoneal dialysis is often used to stabilize the condition.
Rehabilitation
If the patient survives an acute attack of pancreatic necrosis of the pancreas, he becomes temporarily disabled for at least 3-4 months. Discharge from the hospital is carried out 1.5-2 months after the attack. In the first month, the patient needs to moderate activity and avoid physical overload.
After stabilization of the patient’s condition, physiotherapy and therapeutic exercises are prescribed.
You need to follow the diet prescribed by your doctor and take medications necessary for the normal functioning of the gastrointestinal tract.
After stabilization of the patient’s condition, physiotherapy and therapeutic exercises are prescribed.
In most cases, patients require maintenance medication and a special diet throughout their entire lives.
Nutrition
Dishes for patients who have survived acute pancreatic necrosis of the pancreas are steamed or boiled. Portions should be small. Products are introduced into the patient’s diet gradually.
Food should be consumed 6 times a day at the same time. Dishes should be served to the patient in crushed form. Hot and cold should be excluded. The temperature of the food should be at room temperature.
Alcohol must be eliminated completely.
Alcohol must be eliminated completely.
Consequences
Progressive necrotic decomposition of the pancreas leads to complete disruption of its function. Many patients who have suffered this pathological condition develop chronic pancreatitis, which cannot be completely cured. In places where purulent abscesses are localized, false cysts can form.
Diabetes mellitus is one of the severe consequences of pancreatic tissue necrosis.
In addition, due to impaired production of necessary enzymes, patients experience various digestive dysfunctions.
Often, after the end of the acute period of pancreatic necrosis of an organ, a persistent disturbance in the lipid composition of the blood is detected. Diabetes mellitus is one of the severe consequences of pancreatic tissue necrosis.
Complications
In most cases of pancreatic necrosis, patients experience severe complications.
In the process of damage to the pancreas by the necrotic process, other vital organs and systems are often affected.
Organ
Against the background of acute pancreatic necrosis, the inflammatory process often spreads to the liver tissue, which leads to the development of hepatitis. Frequent organ complications observed with pancreatic dysfunction include:
- carditis;
- nephritis;
- encephalopathy;
- respiratory disorders.
Frequent organ complications observed with pancreatic dysfunction include carditis.
This often becomes the cause of the development of multiple organ failure. In the presence of such complications, death occurs in almost 100% of cases.
Purulent
Even with a favorable course, the necrotic process in the pancreas becomes the cause of such purulent complications as:
- peritonitis;
- phlegmon of retroperitoneal tissue;
- abscess of the abdominal organs;
- fistulas;
- ulcers.
Even with a favorable course, the necrotic process in the pancreas becomes the cause of purulent complications such as peritonitis.
When purulent contents from the pancreas enter the bloodstream, septic shock can develop. The occurrence of these complications requires immediate surgical intervention.
How long do they live after pancreatic necrosis of the pancreas?
In young people, the chances of survival during acute pathology are no more than 50%. Among patients over 45 years of age, the mortality rate reaches 70%. In older people, the probability of recovery is no more than 4-12%.
Approximately 25% of patients who survive an acute attack of pancreatic necrosis of the pancreas subsequently develop diabetes mellitus, pseudocysts form, and chronic pancreatitis is observed.
Complete recovery with complex treatment is observed in no more than 5% of patients.
Reviews about life forecast
Oleg, 40 years old, Moscow
My uncle suffered from an attack of pancreatic necrosis due to alcoholism. Before this, he had had exacerbations of pancreatitis several times, but this did not bring him to his senses and he continued to drink. The death occurred one day after the onset of an attack of pancreatic necrosis of the pancreas.
Vladislav, 35 years old, Vladivostok
In my youth I did not lead a very healthy lifestyle. As a result, at the age of 23 I was hospitalized with this diagnosis. Having survived an attack of pancreatic necrosis, it took more than 2 years to recover, but even now I try to stick to my diet. I completely eliminated alcohol from my life, because even a small dose of it provokes an exacerbation of pancreatitis.
Source: https://pankreatit.guru/vidy/ostryj/pankreonekroz