In the digestive canal, as a result of chemical processing of food, aqueous solutions of food breakdown products are formed, which enter through the epithelial cells of the mucous membrane into the blood and lymphatic vessels.
The layer of food adjacent to the walls of the digestive canal is naturally first digested by the action of enzymes of digestive juices secreted by glands located in the mucous membrane, and the products of its breakdown are absorbed as digestion proceeds. Therefore, in layers of food distant from the wall of the digestive tract, digestion and absorption decrease increasingly with increasing distance from the mucous membrane of the digestive canal.
Absorption is a physiological process characteristic of living cells of the digestive canal, located between the external and internal environments.
In the stomach, only slow absorption of the breakdown products of carbohydrates, as well as salts, water and alcohol occurs. A very small portion of food is absorbed in the duodenum, no more than 8%.
The main sites of absorption are the jejunum and ileum. The total absorption surface of the intestine reaches 5 m2 in humans.
Since the intestinal mucosa contains about 4 million villi, increasing its surface by 8 times, it reaches 40 m2. But if we consider that on each square millimeter of the surface of the ciliated epithelium covering the villus there is a brush border consisting of 50-200 million cylindrical outgrowths of the cytoplasm, visible only under an electron microscope, then the total absorption surface of the intestine is 500-600 m2.
Each villus receives from 1 to 3 small arteries - arterioles. Each arteriole in humans branches into 15-20 capillaries located directly under the epithelial cells. When absorption does not occur, most of the capillaries of the villi do not function, and blood from the arterioles flows directly into the small veins. During absorption, the capillaries of the villi open and their lumen expands. The surface of the capillaries makes up approximately 80% of the epithelial surface, and therefore the intestinal epithelium is in contact with the blood over a large surface area, which facilitates absorption. There is also a lymphatic vessel inside the villus. Due to the existence of valves in the lymphatic vessels, lymph flows out of the villi in only one direction. Before lymph enters the thoracic duct, it certainly passes through one of the lymph nodes.
The villus contains smooth muscle fibers and a nerve network connected to the Meissner plexus, which is located in the submucosal layer. These smooth muscle fibers contract. In this case, the villi are compressed, blood and lymph are squeezed out of them, and after the villi relax, aqueous solutions of nutrients penetrate through the epithelial cells, i.e., they are absorbed again.
Contraction and relaxation of the villi occur within several hours after feeding. The frequency of these contractions is approximately 6 times per minute.
The villus contracts when the food mass touches its base. The contraction is caused by the participation of the Meissner plexus and is enhanced by irritation of the splanchnic nerves. Hydrochloric acid extracts the hormone villikinin from the mucous membrane, which stimulates contraction of the villi, which increases absorption.
Onions, garlic, pepper, and cinnamon in large dilutions increase the activity of villi by more than 5 times.
Absorption in the mouth
Saliva contains enzymes that break down carbohydrates into glucose. The first is ptyalin or amylase, which breaks down starch (a polysaccharide - the most complex type of compound) to maltose (a disaccharide consisting of two monosaccharide residues). The second enzyme is called maltase and must break down disaccharides into glucose. But due to the short period of stay of food in the oral cavity - 15 - 20 s, starch does not completely break down into glucose, for this reason monosaccharides are just beginning to be absorbed. Saliva exerts its digestive effect to a greater extent in the stomach.
The role of hydrochloric acid in digestion
One of the components of gastric juice is hydrochloric acid . Parietal take part in the formation of hydrochloric acid , forming H + and transporting Cl– ions from the blood into the stomach cavity.
Functions of hydrochloric acid:
- denaturation of food proteins,
- bactericidal effect,
- releasing iron from the complex with proteins and converting it into a divalent form, which is necessary for its absorption,
- conversion of inactive pepsinogen into active pepsin,
- reducing the pH of gastric contents to 1.5-2.5 and creating an optimal pH for pepsin to work,
- stimulation of the secretion of the intestinal hormone secretin .
Absorption of nutrients in the stomach
The digestion process is enhanced by the action of hydrochloric acid and enzymes - protease (destroys protein), lipase (breaks down fats) and amylase (breaks down carbohydrates).
Some types of nutrients take longer to process than others. For example, fat and protein take longer to digest compared to carbohydrates, because... later enzymes are released.
Despite the fact that the stomach is the center of digestive activity, a small number of nutrients are absorbed there. The following can be absorbed in the stomach:
- some amino acids;
- partially glucose;
- a larger volume of water and dissolved minerals (copper, fluoride, iodide, molybdenum);
- Alcohol is well absorbed.
Tissue breakdown of proteins. The role of chaperones and ubiquint in this process.
Amino acids formed as a result of the digestion of proteins in the gastrointestinal tract enter the blood and are delivered to the liver, where some of the amino acids are used for the synthesis of blood proteins, and the other part is carried by the blood to various tissues, organs and cells. The second source of free amino acids is endogenous hydrolysis of proteins. The process of updating amino acids in tissue protein molecules occurs at high speed (blood proteins - 18-45 days). The breakdown of tissue proteins is carried out with the participation of an active system of proteolytic enzymes, collectively called tissue proteinases or cathepsins. But they cannot act in full force in the animal’s body, because... this requires an acidic environment of 4-5, and such a concentration of H ions that occurs in tissues after death or in a focus of inflammation, which is accompanied by self-digestion of the tissue. But, nevertheless, the activity of proteinases at pH 7.2-7.8 completely ensures the constant self-renewal of proteins.
In tissues, proteinases 1,2,3 and 4 , which, according to their mechanism of action, are close to the corresponding gastrointestinal enzymes: 1-pepsin, 2-trypsin, 3-carboxypeptidase, 4-aminopeptidase. These enzymes ensure constant hydrolysis of proteins and contribute to the formation of a pool of free amino acids in cells, intercellular fluid and blood.
Chaperones
Chaperones are universal conservative proteins that bind other proteins and stabilize their conformation. They can correct deficiencies in proteins both after their synthesis and during synthesis on ribosomes, be included in multimeric complexes or pass through various cell membranes. Chaperones prevent protein aggregation before completion of folding and prevent the formation of dysfunctional or unproductive conformations during this process.
Ubiquitin
In general, the role of ubiquitin looks like this. A covalent bond is formed between ubiquitin and the substrate protein, which occurs between the amine groups of the protein lysine residues and the carboxyl group of the terminal ubiquitin residue. The resulting conjugates, which contain more than one ubiquitin molecule, can be degraded by proteinases, mainly proteasomes. Recognition of proteins subject to proteolysis is carried out by the so-called ubiquitin complex, which is capable of interacting with waste or abnormal proteins. ATP is consumed both at the stage of formation and at the stage of degradation of ubiquitin-protein conjugates. There is reason to believe that ubiquitin causes significant conformational changes in the substrate protein, which makes this protein sensitive to proteolysis. The binding of a protein to ubiquitin serves as a signal for the “recognition” of this protein by proteinases, which provides a mechanism for the selective degradation of intracellular proteins.
Absorption in the small intestine
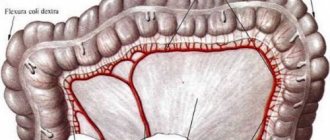
Next stop is the small intestine - the place where almost all nutrients are absorbed. This is largely due to its structure, since the organ is well adapted to the absorption function. Absorption of nutrients as a process depends on the size of the surface on which it occurs.
The internal surface of the intestine is about 0.65-0.70 m2, while villi 0.1-1.5 mm high increase its volume. One square centimeter contains 2,000-3,000 villi, due to which the actual area increases to 4-5 m2, two to three times the surface of the human body.
In addition, the villi have finger-like projections called microvilli. They also increase the absorption surface of the small intestine. Between the microvilli there is a significant amount of enzymes involved in parietal digestion.
This type of breakdown of nutrients is very effective for the body, especially for the course of absorption processes. This is explained by the following state of affairs. The intestines contain a significant number of microorganisms. If the processes of breakdown of nutrients were carried out only in the intestinal lumen, microorganisms would use most of the breakdown products, and less of them would be absorbed into the blood. Microorganisms, due to their size, are not able to get into the gap between the microvilli, to the site of enzyme action, where parietal digestion occurs.
Let's take a closer look at how nutrients are absorbed in the small intestine.
Movement of nutrients across the intestinal wall
There are two main ways in which nutrients cross the wall of the small intestine and enter the bloodstream: passive diffusion and active transport.
Passive diffusion does not require direct energy input. Experts compare the process of diffusion to passing liquid through gauze, where nutrients move from an area of high concentration (the intestinal cavity) to an area of low concentration (the bloodstream). Facilitated diffusion is also distinguished - here the movement is carried out with the help of a carrier protein - a molecule that is embedded in the membrane, penetrates it and forms channels.
Active transport means that a nutrient needs a helper or carrier molecule to get through the intestinal wall into the bloodstream. In addition, transfer occurs not along the concentration gradient of a substance (the gradient characterizes the direction of change in the concentration of a substance in the medium), but against it (from an area of low concentration to a high one), requiring the free energy of the body.
Feeling tired or lacking energy after eating a large meal is partly because the body has to work to absorb nutrients. The amount of energy required to transport nutrients depends on the nutrient and its size.
- Active transport is needed for the following nutritional components: glucose, galactose, amino acids, calcium, iron, ascorbic acid, thiamine, folacin, cholic acids and partially sodium.
- The diffusion method is used by most nutrients.
Characteristics of transportation of a number of food components:
- Glucose is absorbed in the mid-small intestine via the sodium-dependent glucose transporter SGLT1 (S = sodium, GL = glucose, T = transport) together with sodium only. Galactose is absorbed by the same mechanism.
- The absorption of fructose depends on the amount of the GLUT5 transport protein in the small intestinal wall. Healthy people can absorb up to 50 grams of fructose at a time, but it is low in GLUT-5—only 0 to 20 grams.
- Amino acids are absorbed in the small intestine via amino acid and sodium transporters by the same mechanism as glucose.
- Sodium is absorbed in the small and large intestine through various mechanisms, such as cotransport with glucose or amino acids. The transport of chlorine is mainly accompanied by the transport of sodium.
- Iron from animal products - heme - is absorbed better than non-heme iron from plant sources. Absorption of the mineral increases when its reserves in the body are low (for example, after bleeding or menstruation) and decreases when they are high.
- Calcium absorption in the small intestine is dependent on vitamin D and is stimulated by parathyroid hormone (PTH), which increases when blood calcium levels fall. Calcium absorption is also stimulated by pregnancy, growth hormone and insulin, and suppressed by thyroxine and cortisol. In general, only about 30% of calcium is absorbed from the diet.
Interesting fact: When nutrients are absorbed in the human intestine, some nutrients are absorbed more easily than others. This depends on the type of food supplied and the relative need for this nutrient. The smaller the amount in the body, the easier it is absorbed.
Don't worry too much about consuming too many nutrients. The body constantly strives for homeostasis - self-regulation aimed at maintaining balance. When there is a deficiency, it absorbs more than is required. Once balance is achieved, absorption is reduced to maintain the appropriate level.
The small intestine has several sections:
- initial - called the duodenum;
- middle – jejunum;
- lower – ileum.
Nutrients that can be absorbed in the duodenum:
- Monosaccharides (glucose, fructose, galactose), to a lesser extent - amino acids and fatty acids.
- Minerals: copper, magnesium, phosphorus, selenium, calcium.
- Vitamins: retinol, thiamine, riboflavin, B3, B7, B9, D, E and K.
After surgical removal of the duodenum, malabsorption (lack of absorption) of iron and calcium may develop.
Nutrients that can be absorbed in the jejunum:
- Lipids (fats, cholesterol).
- Monosaccharides: fructose, glucose, galactose.
- Amino acids and short peptides.
- Vitamins A, B1 (thiamine), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid), B6 (pyridoxine), B7 (biotin), B9 (folate), D, E and K.
- Minerals: calcium, chromium, iron, magnesium, manganese, molybdenum, phosphorus, potassium, zinc.
About 90% of nutrients are absorbed in the first 100-150 centimeters of the jejunum - this is the answer to the question - where the absorption of nutrients mainly occurs. If it is affected by severe disease or surgical removal is performed, while the ileum remains intact, malabsorption does not develop.
Nutrients that can be absorbed in the ileum:
- This is where the bulk of water is absorbed.
- Vitamins: B9, B12, C, calciferol, K.
- Minerals: magnesium, potassium.
Digestible macronutrients are completely absorbed in the small intestine, so in a person in good health, none of them should appear in the stool.
Every day, about 10 liters of water penetrate the small intestine: about 2 liters from the diet, and the rest from saliva, bile, pancreatic and intestinal juices. Of this, 9 liters are absorbed in the small intestine and only about 1 liter moves to the large intestine, where part is absorbed and about 150 ml is excreted in the stool.
Keep in mind!
A huge number of microorganisms live in the human intestine. Most of the “population” consists of beneficial microbes, they are called beneficial microflora. It protects the intestines from dangerous (pathogenic) and not very dangerous (conditionally pathogenic) microbes. Beneficial microflora is involved in the formation of immunity, the production of B vitamins, vitamin K and many essential amino acids, maintains metabolic processes at the proper level, and partially breaks down proteins, fats, and carbohydrates.
If the normal composition of the microflora changes and there are fewer beneficial microbes, your health worsens. Skin problems appear, the functioning of the stomach and intestines is disrupted, and viral diseases become more frequent. Doctors call this complex of symptoms dysbiosis. Poor nutrition, certain diseases, stress, and the use of antibiotics can be the impetus for its development.
There are two ways to cope with dysbiosis: “throw” beneficial microbes into the intestines or create comfortable conditions for the growth of your own microorganisms. For this purpose, probiotics and prebiotics are used. The first are beneficial bacteria, similar to those that inhabit our intestines. The second are dietary fibers, which are food for beneficial microorganisms.
You can get these substances from food. Thus, probiotics are found in “live” kefir and yogurt, and there is a lot of dietary fiber in bran, vegetables and fruits, herbs, and whole grains. However, this is often not enough, and you need to support the body with drugs or dietary supplements.
Absorption in the colon
The following nutrients can be absorbed in the lower intestine:
- Water.
- Minerals: calcium, sodium, chloride, potassium.
- Short-chain fatty acids (acetate, propionate and butyrate), which are formed during the fermentation of indigestible carbohydrates (fiber) and some amino acids by beneficial intestinal bacteria.
- Vitamins produced by symbiotic bacteria: vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B7 (biotin), vitamin B9 (folate), vitamin K.
Soluble dietary fibers (pectin, gum, lignin), polyols (sorbitol, xylitol, etc.) are fermented by intestinal bacteria, and their breakdown products are absorbed in the colon.
Surgical removal of the lower intestine may only affect water absorption.
Suction mechanisms
How does the absorption process occur? Different substances are absorbed through different mechanisms.
- Laws of diffusion. Salts, small molecules of organic substances, and a certain amount of water enter the blood according to these laws. Diffusion involves the spontaneous movement of a substance in a solution, leading to equilibrium of its concentration in the volume.
- Filtration laws. Contraction of intestinal smooth muscles increases pressure, which triggers the penetration of certain substances into the blood according to the laws of filtration.
- Osmosis is the movement of molecules of a substance through a semi-permeable membrane that allows them to pass in only one direction. An increase in blood osmotic pressure accelerates water absorption.
- Large energy costs. Some nutrients require significant amounts of energy for the absorption process, including glucose, a number of amino acids, fatty acids, and sodium ions. During the experiments, with the help of special poisons, energy metabolism in the mucous membrane of the small intestine was disrupted or stopped, as a result, the process of absorption of sodium and glucose ions was interrupted.
Absorption of nutrients requires increased cellular respiration of the small intestinal mucosa. This indicates the need for normal functioning of intestinal epithelial cells.
Contractions of the villi also aid in absorption. The outside of each villi is covered by intestinal epithelium; inside it there are nerves, lymphatic and blood vessels. Smooth muscles inside the walls of the villi, contracting, push the contents of the capillary and lymph vessels of the villi into larger arteries. During the period of muscle relaxation, small vessels of the villi take the solution from the cavity of the small intestine. Thus, the villus functions as a kind of pump.
During the day, approximately 10 liters of liquid are absorbed, of which approximately 8 liters are digestive juices. Absorption of nutrients is carried out mainly by intestinal epithelial cells.
Biological role and structure of proteins.
Proteins are high-molecular nitrogen-containing organic substances, the molecules of which are built from amino acid residues.
All natural proteins consist of a small number of relatively simple structural blocks, represented by monomeric molecules - amino acids, linked to each other in polypeptide chains.
Functions of proteins: 1) Structural:
Please take part in surveys to assess the quality of the site. Every vote matters!
How is nutrient absorption regulated?
A fascinating feature of the digestive system is that it has its own regulators.
Hormonal regulation
The main hormones that control the functions of the gastrointestinal tract are produced and released by the cells of the mucous membrane of the stomach and small intestine.
- Gastrin causes the stomach to produce hydrochloric acid to digest certain foods. It is also necessary for the normal growth of the gastric and intestinal mucosa.
- Secretin stimulates the pancreas to produce digestive juice rich in bicarbonate; liver - synthesize bile; stomach - produces pepsin, an enzyme that digests protein.
- Cholecystokinin promotes the growth of the pancreas and encourages it to produce pancreatic juice enzymes, which leads to the release of the contents of the gallbladder.
Nervous regulation
2 types of neurotransmitters help control the digestive system. The external influence on the gastrointestinal tract is exerted by the brain or spinal cord. The chemicals acetylcholine and adrenaline are synthesized.
- Acetylcholine causes the digestive muscles to contract with greater force and move food through the gastrointestinal tract. In addition, it encourages the stomach and pancreas to produce more digestive juices.
- Adrenaline relaxes the muscles of organs and reduces blood flow to them.
However, more important are the internal nerves that form a dense network in the walls of the esophagus, stomach, and intestines. They are activated when the walls of organs are stretched by food. The internal nerves produce many different substances that speed up or slow down the movement of food and the production of juices by the digestive organs.
Humoral regulation is also involved: vitamin A enhances the absorption of fats, vitamin B – carbohydrates. Hydrochloric acid, amino acids, bile acids intensify the movement of villi, excess carbonic acid slows it down.
Process of absorption of carbohydrates
On average, an adult consumes 200-300 grams of carbohydrates daily. Some of the most common foods contain mainly this nutrient:
- bread;
- potato;
- bakery;
- candies;
- rice;
- pasta;
- fruits and vegetables.
Many of them contain starch, which is digested by the body, and ballast substances (fiber), which are only partially broken down, and the remains are excreted from the body.
Enzymes in saliva, pancreatic juice and small intestinal juices separate digestible carbohydrates into simple components - monosaccharides, which are absorbed into the blood (fructose, glucose, and during lactation - galactose).
- Starch is digested in two stages: first, enzymes in saliva and pancreatic juice break it down (a polysaccharide) into maltose (a disaccharide); then an enzyme - maltase - in the lining of the small intestine breaks down maltose into glucose (a monosaccharide), which can be absorbed into the blood. Glucose travels through the bloodstream to the liver, where it is stored or used to provide energy to the body.
- Another disaccharide, sucrose, is separated by an enzyme in the small intestinal mucosa into glucose and fructose, which is absorbed from the intestinal cavity into the blood.
- Milk contains another type of carbohydrate - lactose, which is broken down by the enzyme lactase into galactose and glucose - absorbed from the intestinal cavity.
Different monosaccharides have different rates of absorption. Glucose and galactose have the highest speed, but their transport is slowed down or blocked if there are no sodium salts in the intestinal juice. They enhance this process, increasing the speed by more than 100 times. In addition, carbohydrate absorption is more intense in the upper intestine.
Carbohydrates are absorbed rather slowly in the colon. However, this possibility is used in medical practice during artificial nutrition of the patient (nutrient enemas).
Protein absorption process
Meat, eggs, seafood beans, tofu, etc. contain protein molecules that must be digested by enzymes before they can be used to create and repair body tissue.
Enzymes in the gastric juice begin the digestion process: pepsin helps break down proteins into peptides. The process is completed in the small intestine. Here, enzymes from pancreatic juice and the intestinal lining break down protein into amino acids, which are absorbed into the blood and transported to all parts of the body.
The process of protein absorption is carried out in the form of solutions of water and amino acids by the capillaries of the villi. 90% of the final products of this nutrient are absorbed in the small intestine and 10% in the large intestine.
Fat absorption process
Fat molecules are the main source of energy for the body. The first step in digesting fats such as oil is to dissolve it in the watery contents of the intestinal cavity through bile acids produced by the liver. They allow enzymes to break down fat into its components. Glycerin (1 component) during absorption easily passes through the epithelium of the intestinal mucosa.
Fatty acids (2 components) and cholesterol (3 components) are combined with cholic acids (bile), the latter helping them move into the cells of the mucous membrane. In them, the components create a whole again - fatty acids combine with glycerol, forming fat, which is characteristic of the human body. Most of these molecules move to the lymph vessels near the intestines. Through them, the converted fat is transferred to the blood vessels of the chest, and from there the blood moves it to different segments of the body.
The breakdown products of pork fat and butter, among other fats, are absorbed much more easily.
The process of absorption of water and salts
Absorption begins in the stomach, but is much more intense in the intestines.
The main volume of content absorbed from the cavity of the small intestine is water with salts dissolved in it. It comes from food, liquids and juices secreted by many glands of the digestive system. In a healthy adult, more than 4.5 liters of water, containing over 28 grams of salt, are absorbed from the intestines into the blood every 24 hours; 1 liter is absorbed in 25 minutes. The rate of absorption of mineral salts depends on their concentration in the solution. Water absorption occurs according to the laws of osmosis.
Diagnosis of the disease
To properly organize the treatment of the disease, instrumental and laboratory studies are required. When palpating the abdomen, pain is noted along the course of the colon, sometimes more pronounced in any of its segments, usually spasmodic and sharply painful.
After examination and history taking, the patient is prescribed laboratory tests:
- General blood analysis. Since colitis is characterized by an inflammatory process, a high erythrocyte sedimentation rate, a high platelet concentration, leukocytosis, and a reduced hemoglobulin level are recorded.
- Coprogram. Traces of blood, leukocytes and red blood cells may be observed in the stool. Culture for infectious and bacterial agents.
- PCR diagnostics. Aimed at identifying helminthiasis and viral intestinal infections. Examination for the presence of certain antibodies in the cytoplasm of neutrophil cells. The analysis makes it possible to determine the presence of genetic autoimmune diseases that negatively affect the functioning of the intestines.
- Examination for fecal calprotectin. Allows you to identify Crohn's disease, the secondary symptom of which may be colitis.
Modern medicine allows us to clarify the diagnosis using instrumental research. Conducted:
- Colonoscopy and sigmoidoscopy. Such examinations can detect catarrhal or atrophic changes in the intestinal mucosa.
- Radiography or irrigography. The procedures allow us to assess the degree of damage to the intestinal mucosa and the localization of the inflammatory process. The study makes it possible to determine dyskinesia.
- Contrast irrigoscopy. A contrast agent is injected into the patient's rectum, after which an x-ray is taken to assess the degree of functional impairment of the organ. The study makes it possible to exclude the proliferation of tumors and stenosis of the intestinal walls.
- Fibroileocolonoscopy. It is an endoscopic examination of the intestine. During the examination, the location of the pathological process, its nature and phase are recorded, and biological material is taken for examination to exclude oncology and the risk of tumor formation.
- Ultrasound, MRI. Ultrasound allows you to determine changes in the lumen of the intestine or the walls of an organ; ultrasound of the abdominal cavity makes it possible to detect inflammation of the liver, pancreas and gall bladder. Examination by palpation of the anus. Carry out to exclude the possibility of hemorrhoids or paraproctitis.
External factors affecting nutrient absorption
In addition to the body's nutritional status, there are other factors that influence the absorption of nutrients. Here are a few key variables.
Stress
Many people have digestive problems such as dyspepsia and heartburn, and this is largely due to stress. They are byproducts of the body's biochemical response to stress. Since this nervous system reaction does not promote digestion, it also negatively affects absorption. Many people take antacids to reduce symptoms, but these drugs can also reduce the absorption of some nutrients, so taking them may be counterproductive. The best plan is to change your attitude towards circumstances over which a person has no control. This can relieve indigestion and heartburn and thus restore normal absorption.
Stress also contributes to:
- imbalance of intestinal bacteria – growth of pathogenic ones;
- development of chronic inflammation;
- increase in pain syndrome.
Quite simple measures can help relieve stress:
- walks;
- yoga;
- meditation;
- herbal teas;
- warm bath;
- keeping a diary where you can express your emotions;
- sufficient sleep for the body, etc.
Medicines
Drug-nutrient interactions can work in both directions. For example, corticosteroids, often prescribed to reduce inflammation after sports injuries, reduce the absorption of calcium and vitamin D. On the other hand, grapefruit and grapefruit juice may increase the absorption of certain pharmaceutical drugs such as Tegretol (an antiepileptic drug) and Zocor (used to treat high blood pressure). cholesterol levels), which can lead to an overdose. Any drug can affect nutrient absorption.
It is important to study the instructions and interact correctly with doctors.
Alcohol
Even when nutrient intake approaches the recommended daily amount, drinking alcohol can cause deficiencies.
Alcohol damages the lining of the stomach and small intestine, altering or reducing the absorption of vitamins and minerals.
Also, according to a 1993 report from the National Institute on Alcohol Abuse and Alcoholism, alcohol interferes with the breakdown of nutrients by reducing the secretion of digestive enzymes.
The recommendation is to reduce alcohol consumption to a minimum.
Caffeine
You don't have to give up your morning coffee to ensure nutrients are absorbed, but wait at least an hour between consuming caffeine and eating food or supplements. Iron is one of the nutrients that is particularly affected by caffeine, which can reduce mineral absorption by up to 80%.
It is worth thinking about how to replace coffee and tea with analogues that do not contain this psychostimulant. You can also mitigate the effects of caffeine on absorption by simply adding a couple of tablespoons of milk or cream to your coffee or tea.
Exercise stress
Intense exercise promotes a healthy body and mind, but harsh and untimely training can affect the efficiency of nutrient absorption. In general, exercise improves intestinal motility, promoting bowel health. But with aggressive and untimely training, the body directs blood and nutrients to the working muscles, diverting attention from the process of digesting and absorbing food. For this reason, it is important to wait a couple of hours between eating and exercising. If the body is not given time to properly absorb nutrients, a person will not be able to get the expected benefits from training. Macro and micronutrients are used in metabolism to produce energy, and a deficiency in any of the nutrients results in lower energy levels.
Prevention
Prevention of colitis, like all other gastrointestinal pathologies, is based on diet. It is important to monitor your health; in case of repeated cases of diarrhea and stomach problems, in case of repeated digestive failures, you need to consult a specialist and undergo an examination. If you have chronic colitis, you should adhere to the rules of a healthy lifestyle. You need to eat right, limit stress and stress.

When a patient has a hereditary predisposition to colitis, he needs to undergo regular examinations, which will help to detect the disease in a timely manner and stop its progression. Preventative measures for colitis in children include preventing intestinal infections, maintaining hygiene, and making appropriate food choices and handling. Preventive vaccination is important for infants and older children.
How to improve nutrient absorption - additional recommendations
The human body can absorb from 10 to 90% of nutrients from food. Study the following tips and apply them if they apply to you.
Repair damaged digestive tract
Almost 90% of nutrients are absorbed in the small intestine. If a person suffers from irritable bowel syndrome or another type of gastrointestinal disorder, nutrients will be poorly absorbed. The solution is treatment + taking probiotics - live microorganisms and/or their metabolites that heal the digestive tract and heal the intestines. Probiotics can also improve almost every function in the body.
Other supplements for treating a damaged GI tract include collagen and digestive enzymes.
Juices
Unlike raw fruits and vegetables, fresh juice is already processed, making it easier to digest.
The right food combination
The body can only absorb some nutrients in combination with others, so they should be combined. For example, fat-soluble vitamins A, D, E and K should be combined with fatty foods.
Avocado oil and coconut oil have been shown to improve nutrient absorption.
Chewing
The process of digestion begins the moment a person begins to chew food. Saliva contains enzymes that help break down food, making it easier to digest. According to the researchers, this process improves absorption. If a person eats quickly, then most likely he is not chewing properly. Recommendations:
- Take small bites of food.
- Take your time and chew slowly.
- Chew until the food loses its texture.
- Do not put more food or liquid in your mouth until the previous portion has been swallowed.
Competition between nutrients during absorption
The truth is that some nutrients occupy a dominant position in the absorption process. For example, calcium interferes with the absorption of iron. Copper and zinc, zinc and iron can also compete. But don't get too hung up on nutrient interactions. Nature “packed” them together, does a person need to separate the nutrients? There are times when additional intake of a mineral or vitamin is required:
- for example, a doctor may recommend iron supplements to correct anemia;
- Female athletes and older adults often need extra calcium;
- Doctors recommend that women take folic acid when planning pregnancy.
However, taking high doses of individual vitamins or minerals without a medical reason leads to nutritional imbalances and increases the likelihood of nutrient competition. This is important to know in order to avoid cases of abuse.
Absorption of nutrients from dietary supplements
For the most part, vitamin-mineral complexes are absorbed in the body in the same way as regular food. However, it is worth paying attention to the following points.
- Bioavailability. The term refers to how efficiently a tablet or capsule is broken down in the body after administration. No matter how good a product it is, if it is not absorbed, the body will not be able to use it.
- Chelation is the wrapping of a nutrient with amino acids. This process increases the bioavailability of minerals. However, chelation must be done correctly to be effective, otherwise it reduces or even blocks nutrient absorption.
- Dosage. Typically, absorption efficiency decreases as the amount of a vitamin or mineral increases. Therefore, if high doses are prescribed, doctors recommend dividing them into parts throughout the day.
- Take dietary supplements with food. A number of experts claim that in some cases, the longer nutrients remain inside the body, the higher the rate of absorption.
Forecast
With timely and successful treatment of intestinal colitis and after full recovery, the acute form of the pathology ends with recovery. In the chronic form of colitis, following a special diet and following the doctor’s instructions ensures long-term remission. If a child has a stable remission, after 24 months he is removed from the register. Intestinal colitis can be treated completely if treatment is started in a timely manner and a special diet is followed. An advanced condition can provoke serious complications that are life-threatening.
Sources: zhkt.guru/kolit-2/vidy-4/diffuznyy-10 okeydoc.ru/kolit-simptomy-klassifikaciya-prichiny-vozniknoveniya-i-lechenie/ thewom.ru/health/kolit-kishechnika-simptomy-i-lechenie -pitanie-pri-kolite-kishechnika-narodnye-sredstva-pri-yazvennom-kolite-kishechnika/ https://vospaleniekishechnika.life/kolit/diffuznyj-kolit.html https://bolvkishkah.com/kolit/diffuznyj-kolit. html gastrot.ru/kishechnik/kolit ogkt.ru/kolit/kishechnika-vidy-i-formy-zabolevaniya-lechenie.html https://gastrosapiens.ru/kishechnik/lechenie-k/kolit-lechenie.html https:// www.ayzdorov.ru/lechenie_kolit_chto.php https://comp-doctor.ru/jkt/pancolitis.php This material is exclusively subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/19/2020