Intestinal organs
An adult human has a small intestine about 7 meters long. The diameter of the small intestine is approximately 2.5 to 3 cm.
Its anatomy begins with the duodenum, and it, in turn, begins with the bulb. The bulb precedes the peritoneal cavity. The peritoneum is a thin membranous cavity that covers the organs in the abdominal area, with some exceptions.
After the duodenum ends, there remains another 40% of the organ called the jejunum. The remaining 60% is the ileum. It ends where the large intestine begins.
The jejunum occupies the left upper abdomen, while the ileum is displaced to the right side and the upper part of the pelvis. The inner walls of the small intestine have folds of mucous membrane. They are completely absent in the ileum.
Absorption in the small intestine occurs through the main type of epithelial layer. Goblet cells, located throughout the epithelial layer, hide mucus that helps protect it from digestion.
Collections of lymphatic follicles are scattered throughout the small intestine. But the greatest concentration lies within the ileum. Pods are present (to a greater extent) in children and infants. This is the correct anatomy of the human intestine.
Environment in the small and large intestines
The environment in the duodenum, as well as in the large intestine, plays one of the main roles in the body.
As soon as it decreases, the number of bifido-lacto- and propionobacteria decreases. This adversely affects the level of acidic metabolites, which are produced by bacterial agents to create an acidic environment in the small intestine. This property is used by harmful microbes. In addition, pathogenic flora leads to the production of alkaline metabolites, as a result of which the pH of the environment increases. Then alkalization of intestinal contents is observed.
Metabolites that are produced by harmful microbes lead to changes in pH in the large intestine. Against this background, dysbiosis develops.
This indicator is usually understood as the amount of potential hydrogen, which expresses acidity.
The environment in the large intestine is divided into 3 types.
- If the pH is in the range of 1-6.9, then it is customary to talk about an acidic environment.
- At a value of 7, a neutral environment is observed.
- Ranges from 7.1 to 14 indicate an alkaline environment.
The lower the pH factor, the higher the acidity and vice versa.
Since the human body is 60-70% water, this factor has a huge impact on chemical processes. An unbalanced pH factor is usually understood as an environment that is too acidic or alkaline for a long time. In fact, this is important to know, because the body has the functions of independently controlling the alkaline balance in each cell. The release of hormones or metabolic processes are aimed at balancing it. If this does not happen, then the cells poison themselves with toxins.
The colonic environment should always be level. It is she who is responsible for regulating the acidity of the blood, urine, vagina, sperm and skin.
The chemical environment of the small intestine is considered complex. Acid gastric juice, together with the food bolus, enters the duodenum from the stomach. Most often the environment there is in the range of 5.6-8. It all depends on which part of the digestive tract is considered.
In the duodenal bulb, the pH is 5.6-7.9. In the area of the jejunum and ileum, a neutral or slightly alkaline environment is observed. Its value is in the range of 7-8. The acidity of the juice in the small intestine decreases to 7.2-7.5. With an increase in secretory function, the level reaches 8.6. In the duodenal glands, a normal pH of 7 to 8 is diagnosed.
If this indicator increases or decreases, it means that an alkaline environment is being formed in the intestines. This adversely affects the condition of the mucous membrane of the internal organs. Against this background, erosive or ulcerative lesions often develop.
Acidity in the large intestine is in the range of 5.8-6.5 pH. Considered acidic. If such indicators are observed, then everything is normal in the organ and beneficial microflora is populated.
Bacterial agents in the form of bifidobacteria, lactobacilli and propionobacteria help neutralize alkaline products and remove acidic metabolites. Thanks to this factor, organic acids are produced and the environment is reduced to normal levels. But as soon as unfavorable factors affect the body, pathogenic flora will begin to multiply.
Harmful microbes cannot live in an acidic environment, so they specifically produce alkaline metabolic products, which are aimed at alkalizing the intestinal contents.
Small intestine and its functions
The intestine has three sections:
- Duodenum.
- Jejunum.
- Ileum.
Food that is in the stomach passes into the duodenum using muscles known as the pylorus. There are 2 main functions of this human organ: digestion and absorption of food.
Digestion. Chemical digestion of food occurs in different parts of the small intestine. Digestive enzymes that work in the small intestine are secreted by the pancreas. Then they move through the pancreatic duct.
Nutrients in this organ cause the secretion of the hormone cholecystokinin. It provokes the production of digestive enzymes. The small intestine retains enzymes. The hormone secretin promotes the release of various bicarbonates, which then move to the small intestine.
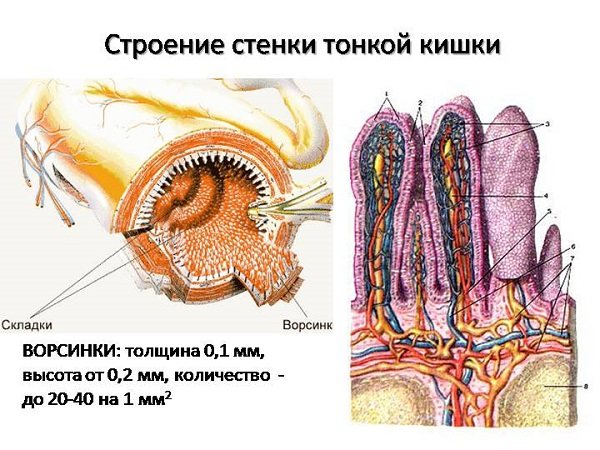
Villi of the small intestine to absorb nutrients
There are three types of nutrients that undergo digestion:
- proteins;
- lipids or fats;
- carbohydrates.
Fats or lipids are broken down into glycerol and fatty acids. Pancreatic lipase uses salts secreted by the gallbladder and liver to emulsify triglycerides and then break them down into free fatty acids.
Triglycerides are broken down into small units that enter the villi for absorption. Some carbohydrates are broken down into monosaccharides, or simple sugars, in the upper small intestine. While pancreatic amylase breaks down some other carbohydrates into oligosaccharides.
Absorption. Most nutrients from digested food are absorbed in the small intestine. The absorption of products necessary for the body occurs through the diffusion of nutrients. All tissues and structures of the organ are used to absorb the necessary elements.
Nutrients are absorbed and passed on to other organs to form complex products such as proteins. Undigested food passes to where the large intestine is located.
Mixed forms of intestinal disease
There are diseases that appear in adulthood and are characterized by ambiguous symptoms. A person may not suspect the presence of pathology for a long time, associating rare pain with recovery from an illness, but by the age of 30-35, signs of the disease begin to actively manifest themselves, leaving the person no choice but to go to the doctor.
Often, after a visit to a gastroenterologist, a person becomes unsure. He begins to wonder where such a disease as, for example, dysbiosis came from, if there were no symptoms before. If the patient had been able to look back, he would have noticed that symptoms such as pain in the small intestine, flatulence or obstruction did not arise out of nowhere. They usually develop against the background of minor diseases that have been ignored for a long time.
Dysbacteriosis
Typically, the first symptoms of this disease appear after 20 years. Since they are nonspecific by nature, dysbiosis is often confused with acute poisoning. According to doctors, dysbiosis is not a disease, but a complex syndrome. A few months of unstable intestinal function are enough for the development of favorable conditions for the development of other diseases. The following signs indicate possible dysbiosis:
- bad taste in the mouth;
- diarrhea;
- pain in the colon area;
- lack of appetite;
- irritability;
- migraine;
- restless sleep;
- depression.
After the doctor determines the causes of dysbiosis, he will prescribe drug therapy to relieve symptoms and improve the functioning of the gastrointestinal tract. Treatment is necessarily accompanied by an individual diet.
Irritable bowel syndrome (IBS)

This is a functional intestinal disorder in which there is a pronounced disorder of colon motility with characteristic clinical signs. At the first stage, this disease is difficult to recognize, since its symptoms are similar to typical poisoning or indigestion. In the first weeks of the disease, disturbances in the functioning of the muscles of the small intestine occur, but patients often ignore the primary signs. After a few months, IBS progresses and is accompanied by:
- sharp pain, especially after eating;
- loose stools alternating with constipation;
- gas formation and bloating.
In this case, there are no inflammatory or any other organic changes in the gastrointestinal tract.
Problems and their solutions
The small intestine is responsible for the normal functioning of the intestines. Intestinal diseases can be the following:
- Dysbiosis. The small intestine, like the entire gastrointestinal tract, usually contains bacteria. Dysbiosis is a condition that causes a large number of bacteria in the small intestine. Dysbiosis can be accompanied by a variety of symptoms, such as increased gas production. There may be diarrhea or, conversely, chronic constipation due to a failure in the absorption of nutrients. Sometimes weight loss may drop dramatically. Patients may also feel fatigue or pain throughout the body. If such symptoms occur, you should immediately consult a doctor. The small intestine will be examined with special instruments, because with this disease the large intestine can also be affected. Dysbiosis is usually treated with antibiotics.
- Enteritis. Symptoms of enteritis:
- Severe diarrhea, including bloody diarrhea.
- Vomit.
- Fever.
- Loss of appetite.
- Nutrient deficiency.
Abdominal pain and discomfort after eating.
In general, clinical symptoms will depend on the extent of damage to the small intestine. Here is a list of some diseases that may affect them:
- giardiasis;
- ascariasis;
- tapeworm;
- helminthic infestation;
- bacterial infections;
- enterotoxigenic Escherichia coli
- campylobacter;
- salmonella;
- pseudomembranous colitis;
- mycobacteria, for example the common Mycobacterium tuberculosis;
- typhoid fever;
- Echinocereus bacillus;
- viral infections;
- rotavirus;
- neoplasms or cancer.
Excessive belching, acute pain similar to gastritis, can indicate that there is inflammation in the lower part of this organ.
On the other hand, if the signs change after a bowel movement, it may indicate minor lesions in the ileum. The small intestine requires a careful diagnostic examination so that all affected sections can be thoroughly examined. After this, the doctor will be able to prescribe adequate treatment.
Flatulence – Symptoms – Website of gastroenterologist Bredikhina
Flatulence (from the Greek word meaning rising, bloating) is an excessive formation, accumulation of gases in the lumen of the digestive tract.
A healthy person's gastrointestinal tract contains about 200 ml of gases. The gases include a mixture of hydrogen, methane, nitrogen, sulfur, and carbon monoxide. Bloating is a common and unpleasant symptom that sometimes causes a person to suffer more than abdominal pain. Bloating is a subjective sensation of excess gas in the gastrointestinal tract; it is included in the medical concept of flatulence syndrome.
Aerophagia
Normally, when eating food and liquid, or swallowing saliva, a small amount of air enters the stomach. But often there is increased swallowing and swallowing more air:
- when eating in a hurry (fast food),
- when talking while eating,
- smoking,
- drinking carbonated drinks,
- drinking through a straw,
- using chewing gum
- with poorly fitting dentures,
- some mental states (anxiety, hysterical psychoses).
Lack of enzymes in the gastrointestinal tract
The lack of enzymes leads to the fact that a large amount of undigested food debris ends up in the lower parts of the digestive tract. The processes of rotting and fermentation are activated there.
During fermentation processes, sudden gas formation , bloating, rumbling, transfusion, and increased release of gases (carbon dioxide and methane) are observed.
This is most often observed after eating plant foods, milk, and rye bread.
Putrefactive processes ( dyspepsia ) develop with excessive consumption of food proteins due to enhanced enzymatic digestion of them. Flatulence is less pronounced, but the gases released are more smelly due to hydrogen sulfide and ammonia.
In the formation of carbon dioxide, the level of hydrochloric acid in the stomach and the activity of pancreatic secretions, enzymatic deficiency (intolerance to lactose, fructose, wheat) are important.
A larger amount of gases is represented by intestinal gases (up to 75%). They are formed during the enzymatic activity of intestinal bacteria during the digestion of food components.
In the small intestine, small gas bubbles mix with food. Only 20% of gases are of bacterial origin.
In the colon, gases are 100% formed by bacteria, and due to the high density of the contents in the intestine, the processes of penetration of gases into the blood are disrupted. This creates conditions for the accumulation of large amounts of gases.
A healthy person can release from 0.5 to 1.5 liters of gases per day. The “food” for colon bacteria is digestible fiber - cellulose, hemicellulose, pectins, dietary fiber.
Under normal conditions, large amounts of gases are absorbed by bacteria (aerobes), which also live in the large intestine.
A violation of the ratio of bacteria that produce gas and bacteria that absorb it causes flatulence.
Gases produced by microflora are involved in the regulation of intestinal function, for example, methane helps slow down peristalsis and causes constipation, and carbon dioxide regulates the peristalsis of the colon, increasing peristalsis.
Malabsorption of food components
Bloating can be observed with increased gas formation in diseases in which the absorption of food components is impaired, in violation of the microbiome of the small and large intestines, gluten intolerance and lactase deficiency, and in the consumption of problematic foods that cause increased gas formation.
Impaired colon motility, constipation and increased sensitivity to stretching of the intestinal wall (visceral sensitivity in IBS and functional diseases) can interfere with the passage of gases and their retention in the intestinal lumen.
Abdominal bloating occurs occasionally in all people and is most often associated with dietary habits and the consumption of “problem” foods.
Foods that cause flatulence
Products that most often cause increased gas formation:
- legumes of all types (white, red, brown), lentils of all types,
- all types of cabbage (white cabbage, broccoli, Brussels sprouts, kohlrabi, cauliflower),
- salads of all kinds,
- dairy products,
- onion,
- celery, parsley,
- garlic,
- asparagus,
- beets, carrots,
- bananas,
- raisin,
- grapes, apricots, plum juice, apples, plums,
- yeast bread (black, bagels, fresh bread, especially wholemeal bread), wheat germ,
- beer,
- nuts (pistachios and sesame),
- soybeans and soy products (tofu, soy milk).
These foods contain a lot of fermentable fructo-oligosaccharides - these are sugars that, when they enter the large intestine, begin to be intensively digested and form gases - wheat products, fruits rich in fructose (eg.
apples, pears), vegetables containing fructans (e.g. onions, asparagus), products containing raffinose (e.g. legumes, beets), sorbitol (sugar-free chewing gum). Oats and potatoes can potentially cause flatulence because...
rich in carbohydrates (sugars, starch).
The microbial composition of the intestine and peristalsis depend on the amount of polysaccharides consumed. Depending on the nature of the intestinal flora and the clinical picture of the disease, gas formation in the intestines is distinguished as fermentative, putrefactive and mixed.
All of them cause psychological discomfort and reduce a person’s quality of life.
Flatulence - clinical manifestations
Flatulence occurs at any age, is one of the most common complaints of patients, and is observed in 85% of patients with diseases of the gastrointestinal tract. Bloating may be seen in older and older adults as a symptom of anxiety. These patients should be examined with oncological suspicion, to exclude colon and ovarian cancer.
Bloating is a subjective feeling of fullness and distension of the abdomen, the appearance of hardness and tension in the anterior abdominal wall, excessive formation and discharge of gases, rumbling, and frequent belching.
Objective manifestations of bloating are:
- increase in abdominal circumference (patients often say: “I want to unfasten the belt at my waist”),
- loud rumbling
- loud belching
- uncontrolled release of foul-smelling gases.
Excessive (loud) belching is a violation of the motility of the upper gastrointestinal tract; there is an odorless belch or belching with regurgitation (bitter or sour belching). Often found in GERD, peptic ulcers, diseases of the biliary tract and gallbladder.
Belching may not be associated with the gastrointestinal tract, but may be determined by improper eating behavior, habits and mental factors.
With functional disorders, swelling and stretching are not constant, and differ in circadian rhythm. For most people, bloating occurs after eating, increases at the end of the day, and goes away overnight.
Diagnoses with the symptom of flatulence
The diagnosis of any form of digestive disorder is clarified by conducting a scatological examination of stool, examining intestinal microflora, determining the acidity of gastric juice, and pancreatic enzymes. According to indications, a thorough laboratory and instrumental examination of the gastrointestinal tract is performed.
Principles of treatment
The treatment of flatulence is based on eliminating the cause of increased gas formation, treating the patient’s existing diseases of the digestive system, removing accumulated gases in the lumen of the gastrointestinal tract, and preventing their formation.
It is recommended to eat frequently in small portions, eat slowly to prevent swallowing air, and chew food thoroughly. You should not talk while eating.
You may need to reduce the amount of food you eat. When eating small portions of food, bloating is not observed, but large meals can cause bloating and distension of the abdomen.
It is advisable to exclude products that cause increased gas formation, carbonated drinks.
To establish the cause of flatulence for some time, it is advisable to keep a food diary, the nature of the sensations in the stomach from various foods.
Moderate physical activity improves gas transport and ensures bowel movements.
When studying individuals suffering from increased gas formation, fluctuations in the intestinal microflora and differences in the microbiome of healthy individuals and patients with bloating and the appearance of bacteroids are noted. Two probiotics have a positive effect - Bifidobacterium infantis and Lactobaccilus acidophilus. Research continues.
- normalizing peristalsis and promoting the removal of gases from the intestines. These can be infusions of dill, fennel, caraway and prokinetics, accelerating the movement of gases through the intestines and their release,
- The drug Trimedat, a universal regulator of gastrointestinal motility, is currently presented on the Russian market. The drug stimulates gastric emptying, normalizes intestinal motility (constipation and diarrhea) and gas movement, reduces visceral sensitivity, reduces the feeling of bloating and discomfort in the abdomen, and relieves abdominal pain. Trimedat is prescribed 200 mg (1 tablet) 3 times a day 30 minutes before meals for 30 days or more.
- sorbents that absorb excess gases and remove them from the body. The most commonly used sorbents are activated carbon, polyphepane, polysorb.
Gases formed in the gastrointestinal tract are foam with multiple small bubbles surrounded by a layer of viscous mucus.
This mucous foam covers the surface of the intestinal lining in a thin layer.
Foam complicates parietal digestion, reduces the activity of enzymes, disrupts the absorption of nutrients and gases by the intestinal wall, and increases the movement of gases through the intestinal tract.
The action of defoamers is based on the release of gases from mucous bubbles. The deposition of foam reduces the volume, restores the absorption of gases through the intestinal wall, accelerates the movement of gases and their release.
It works quickly and effectively. It is an organosilicon compound that has defoaming properties and helps prevent the formation of gases and their destruction. The drug is not absorbed into the blood and is excreted unchanged in the feces.
Espumisan is not absorbed in the intestinal tract, does not affect liver function, does not disrupt the intestinal microflora, does not affect the metabolism of proteins, fats and carbohydrates, and does not interfere with the absorption of vitamins, minerals and trace elements.
The drug can be taken for a long time without adverse reactions, and is used in children, adults, pregnant and nursing mothers.
Espumisan is available in two forms: capsules and emulsions, does not contain sugar, is approved for diabetes, and is used for flatulence of any origin. Espumisan is taken 2 capsules up to 3-5 times a day or 2 ml of emulsion.
Syneticon is part of the enzymatic preparation Unienzyme. Unienzyme can be used when overeating or large amounts of food to improve digestion, prevent gas formation, and protect the mucous membrane (vitamin PP). The drug is taken after meals 2 times a day for 2 weeks, and then “on demand”.
The active component is a natural enzyme - alpha-galactosidase, which reduces gas formation in the gastrointestinal tract by breaking down oligosaccharides contained in problem foods into simple carbohydrates without the formation of gases.
The use of the enzyme alpha-galactosidase in nutrition provides enzymatic activity that is absent in the human body, limiting the entry of oligosaccharides into the large intestine in an undigested form. There they undergo bacterial breakdown with the formation of gases. Taking Orlix provides high efficiency in relieving gas formation.
The recommended dose of the drug is 2-3 tablets during meals with the first portions of food when consuming gas-forming products. Orlix acts instantly, flatulence does not occur when consuming problematic foods. The dosage depends on the amount of problem foods consumed. In the future, the drug is taken “on demand” and the patient himself determines the required dose.
Orlix is safe and can be used by healthy people for any disease of the gastrointestinal tract, functional or organic, in the presence of a symptom of increased gas formation.
Flatulence. Phytotherapy
In the complex treatment of patients with severe flatulence, plants with carminative, antiseptic, anti-inflammatory, and enveloping effects are indicated.
These include plants:
- caraway seeds,
- coriander,
- common fennel,
- pharmaceutical dill,
- garden dill,
- peppermint,
- pharmaceutical camomile,
- yarrow,
- bird cherry,
- Potentilla erecta,
- dandelion,
- chicory,
- alder,
- Oak bark,
- buckthorn,
- zhoster laxative,
- horse sorrel,
- rhubarb, etc.
Depending on the manifestations of intestinal function, plants with laxative or astringent properties are introduced.
Flatulence is better suppressed by plant collections, here are some of them:
- Peppermint, leaves - 2g, chamomile, flowers - 2g, caraway seeds - 2g, fennel, seeds - 2g per 250 ml of boiling water, leave for up to 2 hours. Take 1 tablespoon 20-30 minutes before meals. The collection is recommended for flatulence and constipation.
- Chamomile, flowers - 1g, yarrow, herb - 1g, dandelion, roots - 2g, caraway seeds, fruits - 2g, dill, fruits - 1g, wormwood, herb - 1g, laxative joster, fruits - 2g. Prepare a decoction with 250 ml of water. Take 2-3 tablespoons 15-20 minutes before meals. Collection for flatulence with a tendency to diarrhea.
- Cinquefoil erect, rhizome - 2 g, bird cherry fruits - 2 g, caraway seeds, fruits -2 g, yarrow herb -2 g, valerian officinalis, rhizome with roots 2 g per 250 ml of boiling water, leave for 2 hours. Take 1-2 tablespoons before meals 30 minutes.
Source: https://bredihina.ru/simptomy/meteorizm/
Indications for ultrasound examination of the small intestine
Indications for the use of ultrasound diagnostics include:
- curvature of the rectum, which was shown by rectoscopy;
- constant constipation;
- fecal incontinence;
- the possibility of peritonitis, appendicitis, Crohn's disease;
- suspicion of colitis, intussusception;
- palpation made it possible to palpate an unknown neoplasm;
- rehabilitation period after surgery to control possible relapse;
- X-rays showed that there was a displacement of the organ;
- presence of fluid in the abdominal cavity;
- retrocervical endometriosis in a female patient (intestinal defects are possible);
- early detected cancer in the rectum;
- the presence of a malignant tumor in the prostate in a male patient to check whether it has spread to the intestines.
Return to contents
How is ultrasound performed for problems with the small intestine?
There are 3 methods by which ultrasound is performed on the small intestine:
- Irrigoscopy. A sterile saline solution in an amount of 2 liters is injected into the intestines.
- Transabdominal ultrasound. As with other types of ultrasound diagnostics, during an ultrasound of the intestines the patient lies on the couch on his back, undressed to the waist. A special conductive gel is applied to the desired area; it is non-stick and colorless. You need to take a napkin or towel with you to wipe your stomach after the ultrasound. The ultrasound specialist moves a special instrument over the area of study and looks at the results of the scan on the monitor.
- Endorectal ultrasound. The patient lies on his right side, undressed from the waist down. A special examination instrument is inserted through the anus.
Return to contents
Diseases of the large intestine and their symptoms
The large intestine has the function of absorbing certain substances, as well as removing the remains of processed food from the body.
Problems of this organ indicate discomfort in the lower abdomen. Symptoms of the problem are similar to common symptoms of bowel disease.
This:
- rumbling in the abdominal area,
- pain is felt in the anus, pain symptoms are often observed in the lateral parts of the organ;
- bloating,
- but when stool disorders occur, namely diarrhea, blood and mucus are observed in the discharge;
- there may be mucus discharge from the anus,
- a person experiences fecal incontinence.
The disease has general symptoms:
- exhaustion,
- lack of strength,
- sexual desire disorder.
Colon dyskinesia
A common disorder that indicates that the intestines are working with motility problems, which leads to various difficulties in moving food.
This may occur due to the following factors:
- psychogenic disorders,
- wrong diet
- endocrine diseases,
- functional disorders in the work of other digestive organs.
Symptoms are mostly characteristic of intestinal disease:
- rumbling,
- stool disorder,
- bloating,
- pain in the intestinal area.
Diverticular pathology
The disease is a process where sinuses appear on the intestines. Diverticula are protrusions on the surface of the large intestine. This is caused by the weakness of the walls and the willingness to form such protrusions.
The disease code according to ICD 10 is designated K57.
The symptoms coincide with the general signs of intestinal disease. It’s just that bowel dysfunction manifests itself in a tendency to constipation. With this disease, it is important to choose the right diet.
The disease can lead to complications:
- the appearance of an inflammatory tumor,
- perforation in places where the wall bulges can provoke peritonitis.
Chronic colitis
The inflammatory process of the intestinal mucosa is called chronic colitis. Pathology leads to various changes in the intestinal wall.
Symptoms:
- rumbling,
- flatulence,
- sharp cramps in the abdomen after eating,
- bowel dysfunction is inconsistent: there may be constipation, and then it is replaced by diarrhea;
- poor health,
- there is a bitterness in the mouth,
- loss of appetite.
Nonspecific ulcerative colitis
The disorder is caused by an immune malfunction. Why it appears, experts have not yet found an answer.
With this pathology, the intestinal walls are affected by an inflammatory process, which also has the characteristic of diffuse and ulcerative.
The disease manifests itself with symptoms:
- The stool is often loose, although there may be constipation,
- bleeding,
- general malaise,
- pain in the intestinal area.
Pathology causes consequences:
- perforation of the intestinal wall,
- bleeding,
- colon cancer,
- polyps.
Colon cancer
The tumor arises on the surface of the mucosa and spreads along the lining wall. The disease has a share of five percent in the total number of cancer diseases.
Pathology is often a consequence of neglected and untreated intestinal diseases. The onset of the disease is typical in old age and occurs more often in men.
Common signs of intestinal disease include:
- constipation,
- there is blood in the stool,
- emaciation,
- general malaise.
The tumor is treated by surgical removal, otherwise the prognosis is poor.