With pancreatitis, the inflammatory process causes irreversible degenerative and destructive changes in the structure of the organ, which provoke recurrent pain syndrome and/or a progressive decrease in the functions of the pancreas (digestion suffers the most). The main reason for the development of the disease is alcohol consumption and smoking.
There is also a connection between chronic pancreatitis and pathologies of the biliary tract, stomach and duodenum. Of great importance in the development of chronic pancreatitis is malnutrition (in particular overeating), lack of antioxidants in food, lack of protein and vitamins in the diet, the use of various drugs and chemicals that damage the pancreas (estrogens, thiazide diuretics, azathioprine).
The clinical picture of chronic pancreatitis includes pain and/or indigestion syndrome. The pain usually does not have a specific localization; it occurs in the upper and middle abdomen on the left or in the center and often radiates to the back, sometimes becoming girdling. Most patients experience pain of high intensity and persist for a long period of time.
Typically, the pain intensifies half an hour after eating, although in some patients the pain is not associated with eating. It is impossible to determine pancreatitis by symptoms, since all signs are nonspecific. The diagnosis is made based on the results of laboratory and instrumental examinations.
With the development of pancreatic insufficiency, diarrhea, steatorrhea (fatty feces), flatulence, nausea, belching, loss of appetite, and weight loss occur. At the initial stage (up to 10 years of illness), periods of exacerbation alternate with remission, and the patient is mainly concerned about abdominal syndrome and dyspepsia.
Approximately 10 years after the onset of the disease, exocrine insufficiency occurs. During this period, the pain becomes less intense or disappears completely, and malabsorption syndrome comes to the fore (develops as a result of impaired absorption function because there are not enough enzymes).
To prevent the development of exocrine insufficiency, not only therapy in a hospital during an exacerbation is necessary, but pancreatitis must also be treated at home during remission. Doctors advise adhering to a diet, maintaining moderation in physical activity, and preventing diseases of the stomach, hepatobiliary system, and duodenum.
After an exacerbation, for a long period it is necessary to take medications that relieve the load on the gland and improve digestion. Medicinal herbs that have anti-inflammatory, antiseptic, and analgesic effects can also restore the functions of the pancreas; therefore, alternative medicine treatment methods can also be used as part of complex therapy.
What does the pancreas do?
It has two main functions:
- regulates sugar levels due to the release of insulin;
- participates in the food processing system in the duodenum.
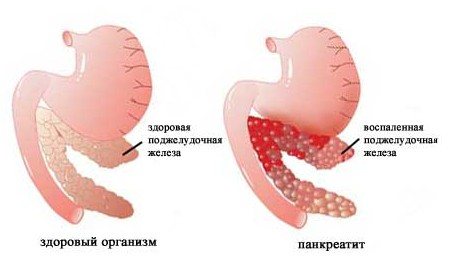
Pancreatitis involves a failure of the digestive system due to disruption of the pancreas, resulting in an excessive accumulation of enzymes in the duct. In this situation, the iron secretes juice, which destroys tissue and impairs its functionality. The connective tissue begins to replenish the damaged cells, but this process only recreates the volume, but does not restore the ability to produce hormones. New cells cannot perform the functions of their dead predecessors. And as a result, digestion loads the remaining cells, causing acute inflammation of the pancreas.
Pancreatitis can occur in acute or chronic form. Like other diseases, the first stages are characterized by attacks. And only in the absence of treatment can they become chronic.
Acute form of pancreatitis
Already during the manifestation of the first acute sign of inflammation, the pancreas begins to digest its own tissues, which is why it can no longer fully perform its original functions.
The acute course of pancreatitis has several degrees of severity, on which the intensity of the symptoms of such a disorder and the general condition of the person will depend.
Pancreatitis
Subject to timely seeking help from specialists and early diagnosis, they speak of a mild form of acute course, during which a small area of the pancreas is observed to be involved in the pathological process. In such cases, the disease can be treated with conservative therapy - prescribing medications and following a diet, which will quickly relieve the patient from the manifestation of external signs of the disease.
Drug therapy includes taking:
- antispasmodics and painkillers aimed at eliminating the main symptom of the disease - pain;
- antibacterial and anti-Helicobacter substances - to eliminate pathological bacteria;
- antipyretics, antiemetics and other drugs.
In moderate pancreatitis, the secretory function of the pancreas is disrupted, and ultrasound examination reveals thickening of the pancreatic tissue.
Severe pancreatitis is characterized by wider damage to the pancreas and often causes the development of severe complications, such as: pancreatic necrosis (death of pancreatic tissue), the formation of cystic neoplasms or abscesses, diabetes mellitus, secondary duodenal ulcers, nephropathy. Such changes are irreversible and lead to the replacement of gland tissue with other structures, which further disrupts the functioning of the organ.
The development of complications leaves virtually no chance of a favorable prognosis and the ability to cure pancreatitis forever.
From the above it follows that a complete recovery from pancreatitis is possible only if this disease is detected early by specialists. However, in cases of ignoring symptoms, unfair therapy and identification of complications, it is completely impossible to cure acute pancreatitis, since it becomes advanced, i.e. chronic.
Causes of pancreatitis
Like most diseases, this ailment can be caused by several reasons, one of them or 2-3 in combination. Here is a list of the most common:
- excessive drinking or alcohol poisoning;
- cholelithiasis;
- metabolic failure;
- drug intoxication;
- abdominal injuries or surgery;
- vascular disease;
- parasite infection;
- infections.
Wormwood
To prepare the medicine, take the above-ground part of the wormwood that blooms. It is used to make aromatic bitterness. In folk medicine, such bitterness stimulates the functioning of the digestive glands, affecting the secretion of pancreatic juice. Infusions of wormwood improve appetite and also have a beneficial effect on the digestion process.
To prepare the tincture, you will need a tablespoon of wormwood, which is poured with a glass of boiling water and then boiled for a few more minutes. The liquid is infused for about 45 minutes, and you can take it after straining in the amount of one tablespoon three times a day. The decoction is taken 20 minutes before meals.

Before using this drug, you should consult your doctor and determine the duration of this course of treatment. Long-term use of wormwood decoction contributes to disorders such as hallucinations, seizures or other mental disorders. Such treatment is prohibited during pregnancy.
Treatment methods
There are several ways to get rid of this disease. It all depends on the symptoms, severity of manifestation and current diseases. Surgery is rarely resorted to, only if purulent adhesions are found in the glands. If you do not promptly intervene in such a situation, the person will die from blood poisoning. There are many ways to prevent or treat the disease. In such a matter as the treatment of pancreatitis, drugs play a major role. But don’t forget about traditional medicine. Doctors at leading clinics believe that fast and effective treatment of pancreatitis in any form is abstinence from food. Hunger greatly reduces the production of enzymes, thereby minimizing the toxic effect on the pancreas.
Strategy 2. Anti-inflammatory diet
The goal is to put as little stress on the pancreas as possible. A vegetarian menu with minimal fat and salt content is best suited for this (3). Perhaps the same mechanisms are at work here, thanks to which a vegetarian diet helps cope with intestinal dysbiosis.
It is recommended to make the basis of the menu vegetables and fruits rich in biologically active substances:
- White cabbage and cauliflower are rich in antioxidants (4);
- apples give us antioxidants and pectins;
- citrus fruits (lemon, lime) contain dietary fiber and somewhat “acidify” the food bolus;
- spices turmeric, cilantro, ginger, cinnamon, parsley and cardamom - their composition is rich in plant flavonoids and essential oils with an anti-inflammatory effect.
Most plants are best eaten raw, this primarily applies to broccoli and other types of cabbage: they should be added to salads, not cooked. Fruits, of course, should be eaten raw.
You can also include milk thistle in the menu. This medicinal plant is sold in finished form and is considered beneficial for the liver. But it also benefits the pancreas.
Attention should be paid to seafood: they are not fatty and nutritious. And they often contain zinc, a microelement whose level in pancreatitis drops far below normal (5). At the same time, the immune system suffers, creating conditions for smoldering inflammation. In addition to oysters, zinc is found in spinach, cheeses, and eggs.
Examinations and immediate measures for pancreatitis
The development of modern medicine has made the treatment of this disease quick and effective. Modern drugs make it possible to abandon surgical intervention and move on to step-by-step therapy. Before starting treatment, an examination, general tests, and ultrasound examination are prescribed.

Patients are admitted to the dispensary mainly with acute manifestations of the disease. The first step when prescribing therapy is to begin treatment with antibacterial and anti-inflammatory drugs. If a purulent formation has been identified, in addition to the main therapy, minimally invasive intervention and antimicrobial sanitation of purulent formations are performed.
A quick positive effect is achieved by suppressing the breakdown of enzymes and removing toxins from the blood that inhibit the patient’s recovery.
Is pancreatitis completely curable with medications?

In the acute phase (the first 1-3 days), the patient is prohibited from eating, he needs to drink alkaline water, and apply cold to the epigastric area. The following groups of drugs are also used:
- To reduce the stimulating effect of hydrochloric acid on the pancreas: antacids - Almagel, Gastal; anticholinergic – Gastrocepin, Atropine; histamine receptor blockers – Ranitidine, Cimetidine.
- To reduce the activity of pancreatic enzymes (trypsin, lipase), anti-enzyme drugs are taken - Trasylol, Gordox.
- To eliminate severe pain: antispasmodics – No-shpa, Papaverine; analgesics – Baralgin.
- To correct water and salt metabolism in the body, use: Reopoliglucin, calcium and potassium preparations; Trisol, sodium chloride solution; hemodesis.
- To correct secretory insufficiency, multienzyme drugs are needed - Digestal, Pancreatin, Creon.
With a rational (without abuse) approach, pumpkin seeds are very useful. They are rich in various amino acids, microelements, and vitamins. But they should only be consumed raw. You can dry it in the sun, but frying is completely excluded.
There is a good recipe that will help cure pancreatitis using honey and pumpkin seeds. You need to take 100 grams of seeds, grind them, add 5 tablespoons of honey, mix thoroughly. Eat half a teaspoon 15-20 minutes before meals.
Use of medications
Treatment of pancreatitis with drugs consists of the use of the following drugs:
- painkillers - “Papaverine”, “No-shpa”, “Ketarol”, “Analgin”;
- antacid drugs - “Phosphalugel”, “Almagel”, “Ranitidine”;
- enzymatic agents - “Creon”, “Pancreatin”, “Omez”.
Proper treatment of pancreatitis, drugs for which only a doctor can prescribe, is impossible without antacids and histamine blockers. Such medications are taken to protect the walls of the gastric tract from the destructive effects of the contents of the pancreas.
It is very important to begin timely treatment of pancreatitis. The drugs most often prescribed for it are the same: Omeprazole and Ranitidine. These drugs reduce acidity and are considered more effective compared to other drugs. But with excessive use of drugs, the rate of juice secretion and the process of breaking down food in the stomach are disrupted.

In certain situations, when treating pancreatitis, drugs from a different group are taken. They serve as substitutes for natural enzymes - “Pancreatin”, “Creon 800”, “Creon 25000”. Medicines reduce the production of pancreatic juice, which destroys tissue.
Strategy 4: Pain Relief
Pain syndrome in chronic pancreatitis serves as a signal that something is wrong with the pancreas, it is beginning to be overloaded. Therefore, by reducing pain using natural methods, we simultaneously have a beneficial effect on the gland.
One option for a pain-relieving (anti-inflammatory) protocol that can be implemented at home is micronutrient supplementation. There are specific observations regarding antioxidants with methyl and thiol groups. As an example, glutathione has been studied (8). It is synthesized in the body and to increase the level of this antioxidant, you need to eat more foods containing sulfur:
- garlic;
- eggs, good - quail;
- natural cottage cheese;
- spinach;
- beet.
In its native form, the content of glutathione in food is negligible. As an alternative, you can take nutritional supplements with glutathione - this will have a positive effect on the health of the pancreas.
Chronic pancreatitis: alternative treatment
If the disease has already left the acute stage, and treatment turned out to be ineffective, then you will face a long period of therapy. Chronic pancreatitis is a long-term inflammatory process in the pancreas. Middle-aged women suffer more from this disease.
Chronic pancreatitis can be a consequence of the following diseases:
- cholelithiasis;
- gastritis;
- enteritis;
- blockage of gland vessels;
- infections;
- worms;
- heavy metal poisoning.
At the first signs of the disease, it is necessary to sound the alarm, but before starting treatment for pancreatitis in adults, medications must be agreed with a doctor. When treating with herbs, it is recommended to carefully select recipes.

In the case of chronic pancreatitis, without natural herbs it would be impossible to eliminate the disease with tablets alone. There are traditional methods of treating pancreatitis that help restore the functioning of the pancreas:
- taking a decoction of medicinal herbs for bile;
- the use of an infusion that localizes the inflammatory process in the bile;
- eating healthy foods five times a day;
- strict adherence to the diet.
Traditional methods of treating pancreatitis recommend wisely selecting medicinal herbs. They are divided into the following categories:
- relieving spasm;
- normalizing digestion;
- enveloping and protecting the mucous membrane.
To reduce the amount of bile, immortelle, dandelion, chamomile, tansy, and knotweed roots are mixed in equal proportions and poured into a liter jar, poured with boiling water and left for one to two hours in a dark place. Drink one glass of the decoction half an hour after each meal.

To relieve the inflammatory process, plantain is used. It is rich in vitamins and natural hepatoprotectors. One spoon of freshly squeezed juice is taken before meals for 30 days. After a break of two to three months, the course is continued.
For pain relief, you need to take crushed leaves of dandelion, motherwort, cucumber, plantain and yarrow. Two tablespoons of the mixture are added to a thermos with boiling water and left for seven hours. It is advisable to drink the medicine at night to relieve pain and reduce bile production. In such a serious matter as the treatment of pancreatitis, medications prescribed by a doctor are not the only thing you can rely on. As you can see, herbs can also play a significant role.
Details about the diet
Diet is an integral part of the treatment of both acute and chronic pancreatitis. Its observance is mandatory both in the stage of remission and during exacerbation, since its further condition depends on what a person eats.

Diet is the main component of treatment for pancreatitis
As mentioned above, during an acute attack, a starvation diet is prescribed. It is recommended to adhere to it for several days. During this period, you are allowed to drink only water in small quantities and at regular intervals.
After the pain attack is relieved, nutrition is based on the principles of feeding a six-month-old child, but with the exception of milk. During this period you are allowed to consume:
- low-fat vegetable soups (they must be pureed),
- puree mixtures,
- freshly squeezed vegetable juices, only unconcentrated and in small quantities (you are allowed to drink no more than 1.5 glasses of vegetable juices per day).
During the rehabilitation period after an attack, it is allowed to eat only boiled or steamed foods without adding salt or other spices. They can be prepared from potatoes, rice, lentils, egg whites, etc. As the body recovers, meat and fish dishes, as well as low-fat dairy and fermented milk products are gradually added to the diet. A more detailed list of permitted foods after an exacerbation should be provided by your doctor.
The most important thing for every person suffering from pancreatitis is to know what foods he is strictly forbidden to eat in order to prevent the disease from progressing and prevent its exacerbations. These products are:
- all fatty meats and fish,
- fried and fatty foods,
- salo,
- canned food,
- smoked meats,
- pickles,
- sausages,
- semi-finished products
- rich pastries,
- dairy and fermented milk products high in fat.

Eating even small quantities of prohibited foods can lead to a painful attack.
If the patient gives up bad habits and constantly adheres to a therapeutic diet, he will be able to forget about exacerbations for a long time and maintain his health for many years!











