Radiation proctitis is an inflammation of the rectum that occurs during radiation therapy for tumors of the pelvic organs. This condition is accompanied by pain in the rectum and anus, painful urge to defecate, diarrhea, and discharge of mucus and blood from the rectum.
The likelihood of radiation damage to the intestinal wall and the development of proctitis is directly related to the total focal dose received during RT. The optimal tolerated total focal dose in the pelvic area is 40-50 Gy. In this case, the probability of developing complications is about 3-5%. When the SOD increases to 65 Gy, radiation proctitis develops in half of the patients.
- Causes of intestinal inflammation after radiation therapy
- Phases of radiation damage
- Classification of radiation proctitis
- Symptoms of radiation proctitis
- How is radiation proctitis diagnosed?
- How is radiation proctitis treated?
- Forecast and prevention of radiation proctitis
Causes of intestinal inflammation after radiation therapy
The following mechanisms underlie radiation damage to the intestine:
- Damage to the intestinal epithelium that develops under the influence of ionizing radiation. This leads to its focal necrosis, desquamation (peeling) and atrophy.
- Development of nonspecific inflammation of the mucous membrane and submucosa. The tissues are infiltrated by neutrophils, hyperemia, swelling, and bleeding are observed.
- Due to trophic disorders (arterioles are damaged), the blood supply to the affected areas of the intestinal mucosa deteriorates, which further aggravates ischemia and necrosis. As a result, atrophic changes progress with the development of fibrosis of the submucosal layer.
- Against this background, pathogenic flora begins to join, which causes infectious complications, including sepsis.
The end result of long-term trophic disorders of the intestinal wall and necrosis is the formation of strictures (narrowing of the lumen), the formation of fistulous tracts, the formation of telangiectasias and the development of bleeding from them.
Diagnostics
The mucous membrane always has a hyperemic character. The color of the anus is red. An admixture with pus is noticeable in the intestinal lumen. The inflammation is very strong, making digital rectal diagnosis difficult.
For the study you need:
- cytological analysis of stool;
- anoscopy or sigmoidoscopy;
- biopsy of purulent areas;
- colonoscopy;
- coprogram or coprocytogram;
- bacterial culture of fecal contents;
- general analysis of stool, urine and blood;
- stool analysis for worm eggs.
For diagnosis, the rectoscopy method is often simply necessary, with the help of which you can clearly and in detail examine the intestinal walls, the presence of pathologies on the mucous membranes, the possible presence of tumors, and identify the root cause of the formation of purulent proctitis.
Phases of radiation damage
Depending on the timing of appearance, early and late radiation damage are distinguished. Early ones make themselves felt directly during radiation therapy, or within 100 days from the date of its completion. This period (100 days, or three months) is the deadline for epithelial recovery from sublethal damage. At this stage, the etiological factor is damage to the intestinal epithelium with the development of inflammatory reactions. If the radiation dose is small, the epithelium is restored quite quickly, and, accordingly, the mucous membrane returns to normal. On average, this takes about 2-4 weeks from the last radiation session.
Late radiation injuries develop 100 days after the end of radiation therapy. During this period, vascular disorders due to damage to the endothelium come first. Its cells become necrotic, and in order to restore them, the remaining endothelial cells begin to actively proliferate. This leads to obliteration of the lumen of blood vessels, the development of thrombosis, ischemia and trophic disorders. As a result, radiation vasculitis develops with bleeding, atrophic processes, fibrous changes, and the proliferation of scar tissue.
Classification of radiation proctitis
Depending on the severity, the following types of radiation proctitis are distinguished:
- Catarrhal proctitis. During the examination, a hyperemic, loose, edematous intestinal wall is discovered. There may be increased mucus production. This form of proctitis is considered mild.
- Erosive-desquamative proctitis. This form is manifested by foci of destruction of the epithelium with the formation of erosion - a tissue defect within the epithelial layer.
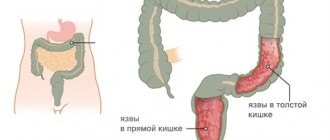
- Ulcerative proctitis - destruction spreads to deeper layers of tissue and involves the mucous membrane and submucosa in the process.
- Fistulous proctitis. A through perforation of the intestinal wall is formed with access to the pelvic cavity or with the involvement of nearby organs, for example, the bladder or vagina.
There is a classification of radiation proctitis based on the rectoscopic picture:
- There is local redness and friability of the intestinal mucosa, telangiectasias and dilated blood vessels are noted).
- Against the background of hyperemia and edematous intestinal mucosa, ulcers covered with a gray scab are found.
- Against the background of inflammatory lesions, strictures of the intestinal wall are detected.
- Against the background of ulcerative lesions, strictures and fistulas or intestinal perforation are detected.
Symptoms of radiation proctitis
Symptoms of acute radiation proctitis develop within 1-2 weeks after the start of radiation. It can be:
- Diarrhea.
- Pain in the rectal area or lower abdomen.
- Painful urge to defecate.
- Discharge of mucus from the anal canal or its admixture in the stool.
- Anal incontinence.
- Bleeding. In some patients, bleeding is profuse and leads to acute hemorrhagic anemia, which requires blood transfusion.
If there are no symptoms of acute radiation proctitis, this does not mean that long-term consequences will not occur. The frequency of late post-radiation proctitis is about 10% of the total number of cases. There is a latent period that lasts several months or even years. The clinical picture is characterized by the following symptoms:
- Pain in the right iliac region or rectum.
- Frequent stools, tenesmus.
- Presence of blood in the stool.
- When strictures form, constipation and partial intestinal obstruction may occur.
- When fistulas are forced, pathological cloudy vaginal discharge, pneumaturia (air in the urine), loose stools with impurities of undigested food are noted.
Depending on the severity of the disease, there are several degrees of the disease:
1st degree - mild proctitis. Accompanied by mild diarrhea, less than 5 times a day, there may be a discharge of small amounts of mucus and blood.
2nd degree - proctitis with a controlled course. Moderate diarrhea, more than 5 times a day. A large amount of mucus is released and there is bleeding.
3rd degree - proctitis with severe course. There are strictures and bleeding from the rectum requiring surgical intervention.
Grade 4 is a life-threatening course that requires immediate intervention. It is accompanied by intestinal obstruction, fistulas, and heavy bleeding.
Sample menu for the week
You can create a weekly menu yourself, choosing from the recommended dishes the one that suits your taste the most. Here is a list of a healthy diet with five meals a day for patients with proctitis in the recovery stage and a tendency to constipation.
| Day of the week | First breakfast | Lunch | Dinner | Afternoon snack | Dinner |
| Monday | semolina porridge without milk soft-boiled egg green tea with crackers | curd casserole prune jelly | chicken broth with dried loaf croutons boiled beef in a piece with vegetable puree dried apricot compote | stewed apple rosehip decoction cracker | boiled fish mashed potatoes kefir |
| Tuesday | cottage cheese with low-fat sour cream glass of cocoa with milk drying | oatmeal apricot compote | noodle soup with spider web vermicelli steamed cutlets with boiled potatoes rosehip decoction | baked apple green tea | stewed vegetables in meat broth with meatballs and yogurt |
| Wednesday | Rice porridge with water, oatmeal jelly with croutons | muesli with berries on kefir | fish soup dumplings with cottage cheese berry compote | pear with cottage cheese | lazy cabbage rolls green tea |
| Thursday | Hard boiled egg buckwheat porridge on water rosehip decoction with breadcrumbs | cottage cheese with raisins and a spoon of sour cream cocoa yesterday's bun | chicken soup with a piece of meat and carrots vegetable puree with quenelles dried fruits compote | banana | beef and rice meatballs kefir |
| Friday | oatmeal porridge without milk green tea with honey toasted white bread | decoction of prunes and figs with steamed fruit, crackers | meatball soup cottage cheese casserole rosehip decoction | decoction of dried apricots with honey white bread | oatmeal, sweetened with honey, yogurt |
| Saturday | piece of boiled chicken cottage cheese rosehip decoction | semolina porridge green tea | milk soup (diluted in half with water) with noodles meatballs with rice porridge prune decoction | oatmeal jelly with croutons | steamed fish with vegetable stew kefir |
| Sunday | buckwheat with stewed carrots, prune broth | steamed omelette dried fruit compote | vegetable soup chicken with buckwheat berry jelly | cocoa with dryings | boiled chicken with potatoes berry jelly |
It is recommended to drink additional fermented milk drinks before bed.
How is radiation proctitis diagnosed?
Diagnosing diseases is not difficult. The key point here is the presence of a history of radiation therapy and its effect on the pelvic organs, increased frequency of stool, and the presence of pathological impurities in it.
If the course is prolonged, it is recommended to examine the rectum using a rectoscope or endoscope. This will allow you to detect multiple erosions, scar deformation, atrophic changes and telangiectasias and decide on the need for endoscopic or surgical treatment.
Prevention
To prevent the occurrence of inflammation in the intestines and anus, to prevent the development of its relapses and again not to take antibiotics and ointments, it is necessary to use the following preventive measures against proctitis:
- promptly treat any gastrointestinal pathologies;
- eliminate inflammation in nearby organs as quickly as possible;
- eat right;
- forget about alcohol and smoking;
- carefully observe intimate hygiene;
- use condoms to exclude the possibility of transmission of infection through sexual contact.
How is radiation proctitis treated?
If symptoms of radiation proctitis develop during radiation therapy, a revision of the radiation regimen is required. For mild damage, it is enough to increase the intervals between sessions. In more severe cases, the question arises of reducing the total focal dose or even canceling radiation therapy. In addition, treatment is required, which includes several areas:
- Diet food. An important part of the treatment of post-radiation proctitis is dietary nutrition. Food should contain an increased amount of protein, a sufficient amount of macro and micronutrients. It should also be chemically and physically gentle, i.e. you should avoid spicy, pickled, and canned foods. In addition, coarse plant fiber should be avoided so that it does not injure the already damaged intestinal wall.
- Conservative methods include drug therapy, therapeutic enemas, suppositories, etc. As part of independent treatment, it is used only for mild and moderate pathology; in other cases, it is used as part of complex treatment together with other treatment methods.
- Endoscopic methods - radiofrequency ablation, argon plasma coagulation, etc. Currently, these methods are the gold standard for the treatment of chronic forms of the disease and are mainly used to eliminate bleeding.
- Surgical methods include removal of the rectum with a stoma or coloanal anastomosis. They are used in severe cases when there is a threat to the patient's life. Surgical operations are used to eliminate strictures, fistulas and perforations of the intestinal wall.
Drug therapy for radiation proctitis
The following groups of drugs are used for drug therapy:
- Glucocorticosteroids are the main group of drugs used for moderate and severe proctitis. GCS have a powerful anti-inflammatory effect.
- Analgesics. Different groups of drugs are used, including narcotic drugs.
- 5-aminosalicylic acid (mesalazine) - has an anti-inflammatory and protective effect, thereby protecting the affected mucosa and stimulating its recovery.
- Antidiarrheal drugs. Enveloping and astringent agents and antispasmodics are used.
- Antibacterial drugs. They are prescribed for the treatment or prevention of bacterial complications of proctitis.
Given that the rectum is the terminal part of the digestive tract, many topical drugs are not effective enough when used in forms intended for oral administration. Therefore, preference is given to forms for local use - suppositories, enemas, powders, etc. They act directly on the intestinal wall and have an effect in the shortest possible time.
Surgical treatment of radiation proctitis and radiation injuries of the rectum
Surgical treatment is aimed at eliminating specific symptoms or complications of post-radiation proctitis. This may include continuous bleeding, fistulas and perforations of the intestinal wall, or strictures. Very rarely, surgery is used to relieve uncontrollable pain.
Before planning an operation, it is important to take into account that radiation damage reduces the regenerative capabilities of the tissue, so there is a high risk of complications, including bleeding, poor wound healing, infection and its generalization, as well as long-term negative effects such as severe scarring or anal sphincter failure.
Thus, classical surgical interventions in the acute period are risky, they do not allow complete control of bleeding and can lead to severe, life-threatening complications. Therefore, they are mainly used to eliminate the long-term consequences of radiation proctitis.
Endoscopic treatment methods
Endoscopic treatment methods are safer. They are based on the destruction of the affected part of the intestinal mucosa, followed by necrosis and replacement by healthy epithelium. For this purpose, radiofrequency ablation is used in particular. The method is based on local controlled heating of tissue to produce a thermal burn. The energy source here is radio frequency waves.
During the procedure, a special catheter is inserted into the patient's rectum, which will emit waves and heat the tissue. The standard depth of necrosis is several tenths of a millimeter, so 1-3 pulses are needed to treat one area of the mucosa. The energy intensity is adjusted automatically based on the current temperature of the tissue being treated. This allows you to avoid “overheating” and deep burns.
The advantage of endoscopic treatment is its bloodlessness, a high degree of control during the intervention, and quick results. It is most effective for bleeding. With just one procedure, you can coagulate all pathological blood vessels and stop even heavy bleeding. As a rule, for maximum results, the procedure is carried out 2-3 times at intervals of several months.
Traditional medicine recipes
To eliminate the symptoms of the disease, you can use various folk remedies. They will help get rid of itching and burning, relieve pain and stop rectal bleeding. Among the most common means are:
- Homemade candles made from badger fat, butter, bee products or raw potatoes.
- Ointments based on olive oil or Vaseline.
- Lotions made from decoctions of medicinal herbs - chamomile, oak bark, calendula, etc.
- Decoctions of medicinal herbs for oral administration.
It is important to remember that natural ingredients may cause individual reactions. Therefore, treatment of symptoms of rectal inflammation with folk remedies is possible only after consultation with your doctor. Special hygiene measures are also recommended - microenemas with a decoction of chamomile and other medicines.