The pancreas (lat. pancreas) is an endocrine organ of mixed secretion that performs digestive and sugar-regulating functions in the human body. Phylogenetically, this is one of the most ancient glands. For the first time, its rudiments appear in lampreys; in amphibians, a multilobed pancreas can be found. The organ is represented as a separate formation in birds and reptiles. In humans, this is an isolated organ, which has a clear division into lobules. The structure of the human pancreas differs from that of animals.
Anatomical structure
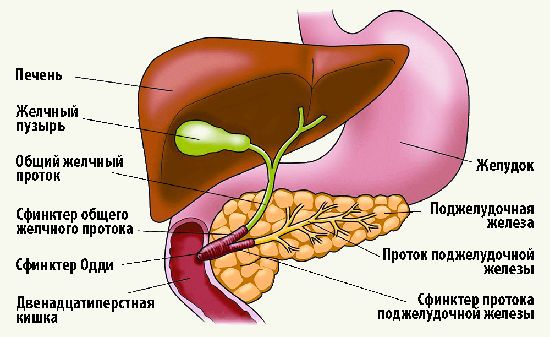
The pancreas consists of three sections: head, body, tail. There are no clear boundaries between the departments; division occurs based on the location of neighboring formations relative to the organ itself. Each section consists of 3-4 lobes, which in turn are divided into lobules. Each lobule has its own excretory duct, which flows into the interlobular ones. The latter are combined into shares. Uniting, the lobes form the common pancreatic duct.
Opening of the common duct is variant:
- Along the way, the common duct unites with the common bile duct, forming the common bile duct, which opens with one hole at the apex of the duodenal papilla. This is the most common option.
- If the duct does not unite with the common bile duct, then it opens with a separate opening at the top of the duodenal papilla.
- The lobar ducts may not be united into one common one from birth; their structure is different from each other. In this case, one of them unites with the common bile duct, and the second opens with an independent opening, called the accessory duct of the pancreas.
Position and projection onto the body surface
The organ is located retroperitoneally, in the upper part of the retroperitoneal space. The pancreas is reliably protected from injury and other damage, since in front it is covered by the anterior abdominal wall and abdominal organs. And at the back - the bony base of the spinal column and the powerful muscles of the back and lower back.
The pancreas is projected onto the anterior abdominal wall as follows:
- Head – in the left hypochondrium;
- Body – in the epigastric region;
- The tail is in the right hypochondrium.
To determine where the pancreas is located, it is enough to measure the distance between the navel and the end of the sternum. Its bulk is located in the middle of this distance. The lower edge is located 5-6 cm above the navel, the upper edge is 9-10 cm even higher.
Knowledge of the projection areas helps the patient determine where the pancreas hurts. When it is inflamed, the pain is localized mainly in the epigastric region, but can radiate to both the right and left hypochondrium. In severe cases, pain affects the entire upper floor of the anterior abdominal wall.
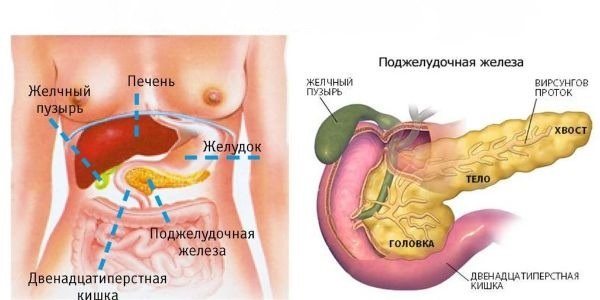
Location and macroscopic structure of the pancreas
Pancreas The pancreas
is located in the upper part of the abdominal cavity. Its boundaries are projected onto the abdominal wall in the umbilical region and the left hypochondrium (Fig. 1). This is where pain in gland diseases is localized. The length of the pancreas in an adult is 15–20 cm, width – 6–9 cm, thickness – 2–3 cm. The mass of the gland reaches 80–100 g. The shape of the gland resembles a triangular prism, elongated from the duodenum on the right to the spleen on the left.
The pancreas gets its name from its location under the stomach when the human body is lying down. In a standing person, the pancreas is located behind the stomach.
Few people know what the pancreas looks like; many have no idea where it is located. This organ is the most protected of all others in the abdominal cavity, as it is located deep. In front it is covered by the stomach, between them there is a fatty layer - the omentum. The head of the gland is wrapped, as it were, in the duodenum, and behind it is protected by the spine and spinal muscles.
The pancreas is located horizontally, it is extended throughout the entire peritoneal space in its upper part. Its largest part, the head, is located at the level of the 1st and 2nd lumbar vertebrae on the left side. The bulk of the pancreas is located midway between the navel and the lower part of the sternum. And her tail reaches the left hypochondrium.

The pancreas is located behind the stomach
The pancreas is in close contact with many organs and large vessels. In addition to the stomach, it directly interacts with the duodenum, as well as with the bile ducts. On the other hand, it touches the left kidney and adrenal gland, and its end touches the spleen. The aorta, renal vessels and inferior vena cava are adjacent to the gland at the back, and the superior mesenteric artery is at the front. It also concerns a large nerve plexus.
If you know where this organ is located, you can recognize the onset of pancreatitis in time by the localization of pain. Typically, pain occurs in the epigastric region on the left. But it can spread throughout the peritoneum in its entire upper part.
The largest gland of the digestive system is located horizontally in the back of the abdominal cavity. The anatomical location of the pancreas is the level of the lumbar vertebrae (L1-L2) and the stomach. The organ of the digestive system has a lobular structure, consisting of small parts (lobules) surrounded by a common bag.
Pancreatic juice is excreted by tubules into the pancreas, the end of which is located in the wall of the duodenum. The digestive system also has a common bile duct, coming from the liver and gallbladder. Macroscopic structure of the pancreas:
- The head is located on the right side, adjacent to the duodenum.
- A body having a triangular shape.
- The tail is a conical or pear-shaped part.
Most of this elongated organ with an irregular cross-section is located on the left side of the midline of the body.

Structure of the pancreas
The functions of the pancreas depend on the characteristic features of the structure and location of organs in the abdominal cavity. The correct location of the organs contributes to high-quality threshing of food and normal secretion of the necessary enzymatic substances and other components involved in the digestive process.
The parts of the pancreas are conventionally divided into: head, body and tail.
structure of the pancreas
The head is located in the duodenal arch. Connects the liver and pancreas through the major papilla and various ducts, including the bile duct.
The organ plays an important role in the assimilation of food. Without it, it is impossible to transform food macromolecules into smaller segments that can be absorbed into the blood. Cleavage to monomers allows their absorption in the small intestine. Digestion itself is conventionally divided into mechanical and chemical. Pancreatic juice, together with gastric juice and bile, plays an important role in breaking down chyme (a semi-digested lump of food) into molecules.
The functions of the pancreas play the most important role in the human body. If there is a disruption in the activity of any part of the organ, the activity of the entire body is disrupted.
Histological and microscopic structure
If you look at the section under magnification, you will notice that the gland tissue (parenchyma) consists of two elements: cells and stroma (areas of connective tissue). The stroma contains blood vessels and excretory ducts. It communicates between the lobules and promotes the release of secretions.
As for cells, there are 2 types of them:
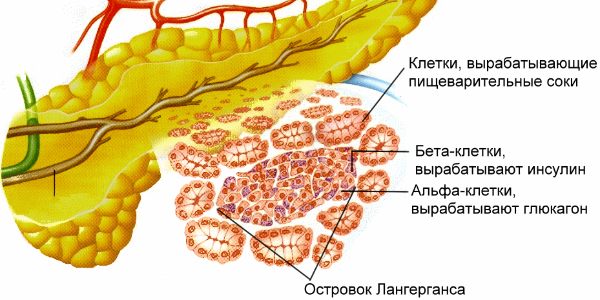
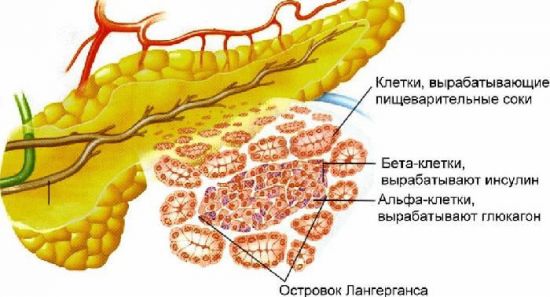
- Endocrine - secrete hormones directly into adjacent vessels, performing an intrasecretory function. The cells are united among themselves into several groups (islets of Langerhans). These pancreatic islets contain four types of cells, each of which synthesizes a different hormone.
- Exocrine (secretory) - synthesize and secrete digestive enzymes, thereby performing exocrine functions. Inside each cell there are granules filled with biologically active substances. The cells are collected in terminal acini, each of which has its own excretory duct. Their structure is such that they subsequently merge into one common duct, the end section of which opens at the apex of the duodenal papilla.
Pancreas histology: histological structure of the pancreas
- 1 Anatomy and functions of the gland
- 2 What is the structure of the liver
The pancreas consists of connective tissue and is enclosed in a dense capsule. It has many capillaries necessary for proper blood supply, so damage to it can lead to dangerous internal bleeding.
The pancreas is located in the abdominal cavity of the human torso. In front of it is the stomach, which is separated by a sebaceous bursa, and behind it is the spine. Lymph nodes, the celiac plexus and the abdominal aorta are located in the posterior part of the gland. It is with this arrangement of the organ that the load on it is distributed optimally.
The shape of the organ is elongated, outwardly reminiscent of a comma. Conventionally, it is divided into parts:
- The head (up to 35 millimeters in length) is located near the duodenum and is tightly adjacent to it.
- Body (up to 25 millimeters) - localized in the region of the first lumbar vertebra.
- Tail (up to 30 millimeters).
Thus, the length of the adult organ itself is, as a rule, no more than 230 millimeters.
The anatomy of the organ is complex. The pancreas is one of the organs of the endocrine system. Its tissues according to the type of structure and structure are divided into two types: exocrine and endocrine.
The exocrine part of the gland forms and secretes enzymes required for digestion in the duodenum. They help digest the main nutritional components in food. The endocrine part produces hormones and carries out metabolism.
Despite the fact that the pancreas is a solid organ, its anatomy and histology are significantly different from others.
What is the structure of the liver
The entire liver is covered with a special membrane made of fibrous tissue. Internally, the liver consists of hepatic lobes, which are the unit of measurement of the organ itself. The structure of the lobules consists of special cells, much smaller in size, called hepatocytes.
In the world, there are only two ideas about the general structure of the liver, since it is not possible to fully evaluate it even with the help of modern instruments.
If we talk about the first idea, then it belongs to the old classical one and belongs to the generally accepted idea. In scientific circles it is more common and states that the entire circulatory system that passes through the liver can be divided into several basic categories:
- the system in which blood flows to liver cells;
- a system that ensures blood circulation within the liver itself;
- a system that ensures the outflow of blood from an organ.
When blood leaves the liver, it is through a single vein and a single artery that help keep this system functioning properly. Circulation directly inside the liver occurs due to a numerous network of capillaries, which are multiple thin vessels.
Typically, the number of lobules inside the liver can reach a million. However, basically this amount varies from 500 thousand, it all depends on the individual characteristics of the human body.
In addition to capillaries, the liver contains lymphatic vessels and nerve fibers, which provide the liver with special sensitivity to changes in the internal environment of the body. That is, with the help of them it can identify any harmful bacteria.
Penetrating into the human body.
Also inside the liver there are peculiar layers, which are called hepatic plates. Their thickness is equal to one liver cell, and at the very edges of the organ, the lobules are able to independently merge into similar plates. In the space between such plates there are capillaries.
However, recently scientists are beginning to talk about such a concept as histofunctional cells, which are also found in the liver. And in this case we can already talk about liver histology. The portal hepatic lobule includes segments of three adjacent classical lobules that surround the triad.
The acini in the liver is formed from several adjacent segments. These are classic type cells that have a diamond shape. In the area of the acute angle there are veins, and at the obtuse angle there is a triad that sends its branches into the very center of the acini.
Also in the liver there are bile ducts that remove excess bile accumulated in the body from the body. Directly from the liver itself, all excess bile is periodically transported to the duodenum. The transport routes are further divided into several routes, which are located inside the liver, as well as outside it.
There are also interlobular bile ducts in the structure of the liver, located in the interlobular connective tissue, which is located in the interlobular space. At the same time, smaller ducts, whose function is to collect bile, are enveloped in a cubic type of epithelium. They merge with the large prismatic epithelium.
The bile ducts, which are located outside the liver, are divided into several types:
- bile flows related to lobar;
- hepatic flow, classified as general;
- a flow called vesicular;
- general bile flow.
A detailed examination of the histology of the liver, as well as other organs, for example, the pancreas, occurs with the help of a histological preparation of the liver or pancreas, which is pieces of tissue of a particular organ that are stained with a special substance.
The mucous membrane, which is located inside the liver, is represented by only one layer of transparent epithelium. The plates that make up this shell have rather loose connective tissue. Which contains many sections of mucous glands.
The liver also contains a membrane called the muscularis lining. Which consists of smooth muscle tissue. They are oriented, as a rule, indirectly or circularly. There is also a membrane inside the organ, which is formed from a connective tissue.
The gallbladder has three membranes on its walls:
- mucosa, which is represented by single-layer and prismatic epithelium;
- the bladder also has a layer that is loose connective tissue;
- The last is the fibromuscular membrane, which is the largest in size and covers most of the internal space of the gallbladder.
The pancreas is a mixed gland, as it consists of several parts:
- exocrine part;
- endocrine part.
The histology of the pancreas begins with its development. The rudiment of pancreatic development begins to appear at the end of the first month of pregnancy. From the already formed elements, blood vessels and nerves gradually begin to appear.
The exocrine system, more broadly speaking, is represented by pancreatic acini and intercalary and bilobed ducts. If we talk about the structural and functional part, then the unit in the pancreas is the pancreatic acinus. It contains several additional threads that perform a full secretory function.
In their shape, they are quite reminiscent of cones, and very elongated at the top of the head. In addition, the pancreas contains zymogen granules, which also contain the necessary enzymes. They have a unique color and method of dyeing.
One part of the cells inside the pancreas is colored oxyphilic, and the other, which is basal and more expanded, is colored basophilic.
This part looks homogeneous in its composition and has selector tubules that are located between the cells, in the lumen of the acinus.
In fact, all these elements, in addition to their direct functions, also perform a protective function. However, the pancreas, due to its special value for the body, also has another protective mechanism. It is expressed, as a rule, in the production of special pancreatic enzymes that do not allow harmful bacteria into the pancreas.
Inside the pancreas there are also centroacinous cells, which are stellate in shape, small and flattened. They present a light-colored cytoplasm with a denser structure. Merging at the exit, these cells form a single duct.
Today it is known that this is how separated cells are transformed into a single whole, which is called the initial section.
The initial section is pushed inside the pancreas, thereby ensuring close contact with the internal and external environment.
The pancreas includes a system of excretory ducts, which are divided into several types:
- actually, the intercalary duct itself;
- ducts located inside the lobules;
- ducts that are located in the space between the lobules;
- the common duct, which acts as an excretory duct.
The intralobular ducts are lined internally with cubic epithelium. The interlobular ducts, in turn, are lined with a mucous membrane, which protects the walls and gives a signal of irritation if a foreign body has penetrated inside. Also in these interlobular ducts there are connective tissues that ensure the integrity of the system inside the pancreas.
Also inside the pancreas are the vagus and sympathetic nerves. The functions of the nerves are aimed at detecting the smallest changes in the internal environment of the pancreas. In addition, age-related changes occur in the gland, which are expressed in a change in the ratio between the endocrine and exogenous parts.
Histology is a scientific branch of biology that studies the structure and functions of the body’s components, tissues and organs. The pancreas is the only organ in the body that forms and secretes both internal and external secretions. Therefore, the histological structure of the pancreas has a rather complex structure.
In order to conduct complete and detailed tissue studies, histological preparations are used. They are pieces of tissue stained with special compounds for examination under a microscope.
Exocrine tissue
The exocrine tissues of the pancreas consist of acini, which form digestive enzymes, and ducts, which remove them. The acini are tightly packed together and connected by a thin layer of loose tissue containing blood vessels. The cells of the exocrine region of the gland are triangular in shape. The cell nucleus is round.
The acini themselves are divided into two parts: basal and apical. The basal membrane contains the membranes of the granular network. When using a histological preparation, the staining of this part will be fairly uniform. The apical one, in turn, takes on sour shades. Using a histological specimen, well-developed mitochondria and the Golgi complex can also be seen.
Source: https://skazz.ru/podzheludochnaya-zheleza-gistologiya-preparat/
Anatomy and functions of the gland
The pancreas consists of connective tissue and is enclosed in a dense capsule. It has many capillaries necessary for proper blood supply, so damage to it can lead to dangerous internal bleeding.
The pancreas is located in the abdominal cavity of the human torso. In front of it is the stomach, which is separated by a sebaceous bursa, and behind it is the spine. Lymph nodes, the celiac plexus and the abdominal aorta are located in the posterior part of the gland. It is with this arrangement of the organ that the load on it is distributed optimally.
The shape of the organ is elongated, outwardly reminiscent of a comma. Conventionally, it is divided into parts:
- The head (up to 35 millimeters in length) is located near the duodenum and is tightly adjacent to it.
- Body (up to 25 millimeters) - localized in the region of the first lumbar vertebra.
- Tail (up to 30 millimeters).
Thus, the length of the adult organ itself is, as a rule, no more than 230 millimeters.
The anatomy of the organ is complex. The pancreas is one of the organs of the endocrine system. Its tissues according to the type of structure and structure are divided into two types: exocrine and endocrine.
The exocrine part of the gland forms and secretes enzymes required for digestion in the duodenum. They help digest the main nutritional components in food. The endocrine part produces hormones and carries out metabolism.
Despite the fact that the pancreas is a solid organ, its anatomy and histology are significantly different from others.
Histological structure of the pancreas
Histology is a scientific branch of biology that studies the structure and functions of the body’s components, tissues and organs.
The pancreas is the only organ in the body that forms and secretes both internal and external secretions. Therefore, the histological structure of the pancreas has a rather complex structure. In order to conduct complete and detailed tissue studies, histological preparations are used. They are pieces of tissue stained with special compounds for examination under a microscope.
Endocrine tissue
This part of the pancreas is formed from the so-called islets of Langerhans, consisting of a collection of cells that have a round and oval shape. This tissue is well supplied with blood due to numerous capillary networks. Its cells stain poorly when using a histological specimen.
As a rule, the following types are distinguished:
- A - produced in the periphery and is considered an insulin antagonist. They can be fixed with alcohol and dissolved in water. Produce glucagon.
- B – represent the most numerous group and are located in the very center of the islands. They are the source of insulin, which lowers blood sugar levels. They dissolve well in alcohol. Poor staining with the drug.
- D – they form and release the hormone somatostatin, which slows down the synthesis of cells A and B. They have an average level of density and size, located on the periphery.
- D-1 – produce a polypeptide and represent the smallest group of cells. They are responsible for reducing pressure by activating the secretion of the gland. They have high density.
- PP cells - synthesize polypeptide and enhance the production of pancreatic juice. They are also located in the peripheral area.
Hormones that are formed by the islets of Langerhans are sent directly into the blood because they do not have ducts. Moreover, the largest part of these areas is located in the “tail” of the pancreas. Their number usually changes over time. So, during the period of active growth of the body, it increases, and after twenty-five years it gradually begins to decrease.
Conclusion
For the study of the pancreas, histology plays an important role. This is necessary for research into common pathologies such as pancreatitis, as well as the development of new drugs, surgeries and procedures.
Source: https://pankreatsindrom.ru/podzheludochnaya/zheleze-gistologiya.html
Physiology
When food enters the stomach cavity and its subsequent evacuation into the cavity of the small intestine, the pancreas begins to actively secrete digestive enzymes. These metabolites are initially produced in an inactive form, as they are active metabolites that can digest their own tissues. Once they enter the intestinal lumen, they are activated, after which the cavity stage of food digestion begins.
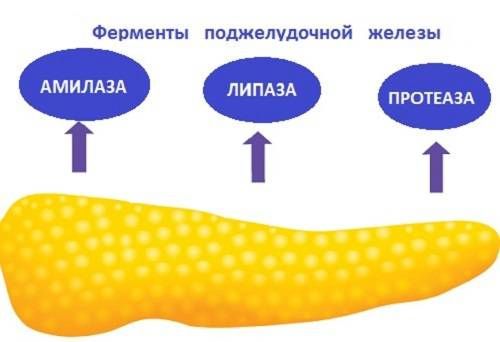
Enzymes that carry out intracavitary digestion of food:
- Trypsin.
- Chymotrypsin.
- Carboxypeptidase.
- Elastase.
- Lipase.
- Amylase.
After digestion is complete, the broken down nutrients are absorbed into the blood. Normally, in response to an increase in blood glucose, the pancreas will immediately respond by releasing the hormone insulin.
Insulin is the only glucose-lowering hormone in our body. This is a peptide whose structure is a chain of amino acids. Insulin is produced in an inactive form. Once in the bloodstream, insulin undergoes several biochemical reactions, after which it begins to actively perform its function: to utilize glucose and other simple sugars from the blood into tissue cells. With inflammation and other pathologies, insulin production decreases, a state of hyperglycemia occurs, and subsequently insulin-dependent diabetes mellitus.
Another hormone is glucagon. The rhythm of its secretion is monotonous throughout the entire day. Glucagon releases glucose from complex compounds, raising blood sugar.
Functions
In addition to enzymes, the pancreas produces hormones (insulin, glucagon, somatostatin). This endocrine (intrasecretory) function is performed by groups of cells called pancreatic islets (islets of Langerhans - after the name of the researcher who described them). There are from 1 to 2 million islets in the pancreas, although their total volume does not exceed 3% of the mass of the gland.
Among the cells of the pancreatic islets, alpha and beta cells are distinguished. The latter make up 60–80% of all cells. They are located in the central part of the islets and produce insulin. Along the periphery of the islets there are alpha cells (10–30% of the total cell mass) that produce glucagon. Another 10% of cells secrete somatostatin (Fig. 3).
Insulin and glucagon regulate blood glucose levels - an important source of energy for many tissues, and for the central nervous system, in fact, it is the only and irreplaceable one. Glucagon promotes the release of glucose from the liver and increases its level in the blood. Insulin, on the contrary, leads to the deposition of glucose in the form of glycogen in the liver, resulting in a decrease in the amount of sugar (glucose) in the blood. Somatostatin inhibits the release of insulin and glucagon.
Insulin is a unique hormone, the function of which is not duplicated by other biologically active substances. Its main effect is to increase cell permeability to glucose. Under the influence of insulin, the rate of glucose transfer into cells increases approximately 20 times. Insulin increases the transport of glucose through the membranes of muscle fibers, promotes the synthesis and accumulation of glycogen in them.
If the function of the pancreas is insufficient, developing as a result of its disease or partial removal, a serious disease can occur - diabetes mellitus.
The most important hormones secreted by the pancreas are insulin and glucagon. Together they regulate carbohydrate metabolism. Insulin increases the penetration of glucose into cells and accumulates its reserves, mainly in the muscles and liver, in the form of glycogen. These components are an energy reserve for the human body.

Pancreatic hormones
Insulin deficiency leads to one of the most dangerous and at the same time common diseases - type 1 diabetes. If the pancreas does not produce enough of the hormone, a patient who does not take treatment is at risk of death. Glucagon has the opposite effect - it increases blood glucose levels and increases its availability in stressful situations, during physical or intellectual activities. This process causes glycogenolysis in the body, that is, the breakdown of glycogen.
Some pancreatic cells in the islet of Langerhans also produce hormones that are essential for human physiological development, such as somatostatin, which modulates the secretion of growth hormone.
The alveolar organ is isolated by parenchyma, consisting of septa. They are composed of connective tissue, nerve sinuses and blood vessels. This is the basis of the endocrine part of the pancreas. The second part is represented by the islets of Langerhans, which are cells regulating glucose levels. The total number of which is no more than one million, their number gradually decreases with age.
The endocrine functions of the pancreas are determined by the work of the islets of Langerhans, consisting of endocrinocytes and insulocytes. The following types are distinguished:
- α cells. The function is based on the production of glucagon. Only 10-30% of the total.
- B cells. Synthesize insulin. (60-80%).
- Δ cells produce somatostatin.3-7%.
- D1 cells inducing VIP (vasointestinal peptide).5-10%.
- PP cells form pancreatic polypeptide. 2-5%.
islets of Langerhans
There is also a separate type of cells in very minute quantities that contain thyrotropin-releasing hormone, gastrin and somatoliberin. What endocrine function does the pancreas perform?
The composition of pancreatic juice includes proenzymes:
- proteinases – trypsin, chymotrypsin, carboxypeptidase;
- amylase, maltase, lactase - for the breakdown of carbohydrates;
- lipase, which affects fats;
- for influencing nucleic acids – ribonuclease and deoxyribonuclease.
Proenzymes are an inert type of enzyme. After the chewed remains enter the stomach, the released hormones activate the reactions. These, in turn, lead to the activation of proenzymes and their conversion into enzymes. This complex mechanism is due to the fact that the gland has protected itself from the effects of its own enzymes on its own tissues.
The endocrine functions of the pancreas are directly related to the activity of hormones that are released into the blood in quantities that will be sufficient to digest certain types of food.
- Insulin controls optimal glucose levels in tissues and cells.
- Glucagon affects liver glycogen, fats and increases glucose in the bloodstream.
- Somatostatin reduces bile production and affects the reduction of certain hormones;
- VIP controls the entire food digestion system and increases bile formation.
The combined activity of insulin and glucagon controls the optimal quantitative percentage of glucose in the blood. What is the additional function of the pancreas? It carries out a humoral function, which is based on the distribution of nutrients throughout the body using fluids (blood, lymph). It is performed by pancreozymin and secretin. The activity is to control the secretion of pancreatic juice.
The secretory function is due to the presence of pancreatic juice, consisting of organic substances and enzymes:
- water by 98%;
- urea;
- protein (albumin, globulins);
- bicarbonates;
- microelements (calcium, sodium, phosphorus, chlorides);
- uric acid;
- glucose.
Salts create an alkaline environment.
The pancreas is an organ of mixed secretion. After all, it consists of different cells, each type of which produces certain hormones or enzymes. It is the pancreatic juice released by the gland that helps digest food normally. And the hormone insulin, responsible for the absorption of glucose, is also produced by this gland.
Therefore, the pancreas performs several functions:
- participates in digestion processes;
- produces basic enzymes for the breakdown of proteins, fats and carbohydrates;
- produces insulin and glucagon to regulate sugar levels.
In order for the gland to properly perform its functions, a combination of many factors is necessary. Her health depends on the normal functioning of the liver, gall bladder, duodenum, proper blood circulation and transmission of nerve impulses. All this affects its functions, mass and structure. The normal size of the pancreas in a healthy person should not exceed 23 cm. And its enlargement may indicate some kind of pathology.
The pancreas performs very important functions in the digestive processes
The pancreas produces pancreatic juice, which contains enzymes necessary to break down proteins, fats and carbohydrates from food. In just a day, approximately 600 ml of juice is produced, sometimes its amount can increase to 2000 ml. And the type and amount of enzymes depend on the nutritional characteristics of a person. After all, the pancreas can adapt and stimulate the production of exactly those enzymes that are needed at the moment.
The production of pancreatic juice begins after food enters the stomach. Although this process often begins at the sight of food or from inhaling its smell. At the same time, a signal is sent to the gland cells through the nerve fibers, and they begin to produce certain substances.
The enzymes that the pancreas produces are produced in an inactive form, as they are quite aggressive and can digest the tissues of the gland itself. They are activated only after entering the duodenum. The enzyme enterokinase is located there. It quickly activates trypsin, which is an activator for all other enzymes.
The main enzymes produced by this gland break down proteins, fats and carbohydrates
This gland secretes various enzymes. Some of them are able to break down proteins, amino acids, nucleotides, others help in the digestion of fats and the absorption of carbohydrates:
- Nucleases - ribonuclease and deoxyribonuclease break down the DNA and RNA of foreign organisms that enter the digestive tract.
- Proteases are involved in protein breakdown. There are several of these enzymes: trypsin and chymotrypsin break down those proteins that have already been partially digested in the stomach, carboxypeptidase breaks down amino acids, and elastase and collagenase break down connective tissue proteins and dietary fiber.
- Enzymes that break down fats are very important. This is a lipase, which is also involved in the production of fat-soluble vitamins, and a phospholipase, which accelerates the absorption of phospholipids.
The pancreas secretes a lot of enzymes to break down carbohydrates. Amylase is involved in the absorption of glucose, breaks down complex carbohydrates, and lactase, sucrase and maltase release glucose from the corresponding substances.
Special cells located in the islets of Langerhans produce insulin and glucagon
Few people realize what the pancreas is for. Usually they find out about it when some pathologies appear. And the most common of them is diabetes mellitus. This disease is associated with impaired glucose absorption. This process is ensured by insulin, a hormone produced specifically by the pancreas. If its production is disrupted, the amount of glucose in the blood increases.
Functions performed and role in metabolism
The pancreas is an organ of the endocrine system that belongs to the mixed secretion glands. It performs exocrine functions (production of digestive enzymes into the cavity of the small intestine) and intrasecretory functions (synthesis of sugar-regulating hormones into the bloodstream). Playing an important role in our life, pancreas performs:
- Digestive function - participation in the digestion of food, the breakdown of nutrients into simple compounds.
- Enzymatic function - production and secretion of trypsin, chymotrypsin, carboxypeptidase, lipase, elastase, amylase.
- Hormonal function - continuous secretion of insulin and glucagon into the bloodstream.
The role of individual enzymes
Trypsin . It is initially released as a proenzyme. Activated in the cavity of the small intestine. Once activated, it begins to activate other digestive enzymes. Trypsin breaks down peptides into amino acids and stimulates the cavity digestion of food.
Lipase . Breaks down fats into fatty acid monomers. It is released as a proenzyme and is activated by the action of bile and bile acids. Participates in the absorption of fat-soluble vitamins. The level of lipase is determined during inflammation and other pathologies.
Inflammation of the pancreas (pancreatitis)
A common pathology among the adult population, in which inflammatory damage to the stroma and parenchyma of the pancreas occurs, accompanied by severe clinical symptoms, pain and disruption of the structure and functions of the organ.
How the pancreas hurts and other symptoms of inflammation characteristic of pancreatitis:
- Pain of a girdling nature, radiating to the right or left hypochondrium. Less commonly, the pain occupies the entire upper floor of the abdominal cavity. The girdling nature of the pain is due to the close location of the superior mesenteric nerve plexus. Due to its structure, irritation of one section of a nerve leads to the spread of a nerve impulse to all neighboring nerve fibers. The pain feels like a hoop squeezing the upper abdomen. Pain occurs after a heavy meal or after a fatty meal.
- Dyspeptic disorders: nausea, vomiting, loose stools (diarrhea) mixed with fat. There may be a decrease in appetite, bloating, and rumbling.
- Symptoms of intoxication: headache, weakness, dizziness. In an acute process, low-grade body temperature is observed. Febrile fever is not typical for pancreatitis.
These signs are characteristic of the edematous (initial) form of inflammation. As the disease progresses, inflammation affects deeper and deeper areas of the tissue, which ultimately leads to necrosis and necrosis of individual lobules, disruption of the structure and functions of the organ. The clinic for this condition is bright, the patient needs immediate medical attention. This is due to the fact that the pain is more pronounced, the patient rushes about and cannot find a comfortable position.

Channels
The main role of the pancreas in the human body is to ensure normal digestion. This is its exocrine function. Pancreatic juice produced inside the gland enters the digestive tract through a system of ducts. They arise from all the small lobules that make up each section of the gland.
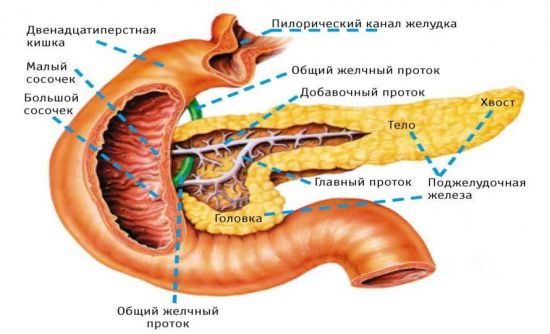
The main duct of the pancreas, connecting with the bile duct, exits into the duodenum
All pancreatic ducts unite into one common one, the so-called Wirsung duct. Its thickness is from 2 to 4 mm, it runs from the tail to the head of the gland approximately in the middle, gradually expanding. In the area of the head, it most often connects with the bile duct. Together they exit into the duodenum through the major duodenal papilla. The passage is closed by the sphincter of Oddi, which prevents the contents of the intestine from entering back.
The physiology of the pancreas ensures high pressure in its common duct. Therefore, bile does not penetrate there, because the pressure in the bile ducts is lower. Only certain pathologies can lead to the penetration of bile into the pancreas. This is a violation of its functions when the secretion of pancreatic juice decreases, spasm of the sphincter of Oddi or blockage of the duct with a gallstone. Because of this, not only stagnation of pancreatic juice occurs in the gland, but also the reflux of bile into it.
This connection of the ducts of the pancreas and gall bladder also becomes the reason why obstructive jaundice is observed in adults during inflammatory processes of the gland. After all, part of the bile duct passes through her body and can be compressed due to swelling. This also often leads to the spread of infection from one organ to another.
Sometimes, due to congenital developmental anomalies, one of the ducts does not connect to the common one and independently enters the duodenum at the top of the head of the pancreas. The presence of such an accessory duct, which is called santorium, is observed in 30% of people; this is not a pathology. Although, if the main duct is blocked, it cannot cope with the outflow of pancreatic juice and is therefore useless.
How to detect inflammation of the pancreas
To identify a particular pathology of the pancreas, including inflammation, one symptom of pain is not enough. Laboratory and instrumental examination methods are prescribed.
Laboratory methods include:
- Clinical blood test to detect the presence of signs of inflammation and intoxication. Inflammation is supported by an acceleration of the erythrocyte sedimentation rate, an increase in the number of leukocytes, and qualitative changes in the leukocyte formula.
- Blood chemistry. Inflammation is indicated by an increase in total protein and qualitative changes in the protein composition of the blood. If a high content of amylase and other organ-specific enzymes is detected in the blood, then we can speak with complete confidence about damage and destruction of glandular cells.
- Biochemical urine analysis. Damage and inflammation of the gland is signaled by the appearance of diastase (amylase) in the urine.
- Functional tests that evaluate the functioning of the pancreas based on the level of secretion of hormones and enzymes.
- Stool analysis to detect the presence of undigested fats and soaps - steatorrhea. This is an indirect sign of inflammation and dysfunction of the pancreas.
Instrumental methods:
- Ultrasound examination of the abdominal organs. A visual examination method that allows you to evaluate the structure and structure of the pancreas. When inflammation occurs in the parenchyma of the gland, structural changes will occur, which a specialist can clearly see even with the naked eye.
- Magnetic resonance imaging is an x-ray examination method based on contrasting areas of lower density. MRI is performed before surgery to assess the extent of the lesion and the structure of the organ, and the extent of the surgical intervention.
- Fibrogastroduodenoscopy (FGDS). Allows you to assess the condition of the stomach, duodenum and the structure of the duodenal papilla. It is also carried out for differential diagnosis and a more accurate diagnosis.
If necessary, laparoscopy, ERCP, plain radiography of the abdominal cavity, and MSCT can be performed. These methods are necessary for differential diagnosis and more accurate establishment of the etiology and topical diagnosis of the disease.

general characteristics
Previously, the pancreas was considered just a muscle. Only in the 19th century was it discovered that it produces its own secretion, which regulates digestion. Research by scientist N. Pavlov revealed what important functions the pancreas performs in the human body.
In Latin this organ is called pancreas. Therefore, his main disease is pancreatitis. It is quite common, since the normal functioning of the pancreas is connected with all other organs of the gastrointestinal tract. After all, she interacts with many of them.
This gland is called the pancreas, although when a person is in an upright position, it is located behind the stomach. This is a fairly large organ - the normal size of the pancreas is from 16 to 22 cm. It has an elongated shape, slightly curved. Its width is no more than 7 cm, and its weight is 70-80 g. The formation of the pancreas occurs already in the 3rd month of intrauterine development, and by the birth of the child its dimensions are 5-6 mm. By the age of ten, it increases 2-3 times.
Endocrine role of the pancreas
The role of the gland is also important in diabetes mellitus. With this pathology, the level of insulin production decreases, and the level of glucose in the blood increases. This leads to the formation of glycated hemoglobin. Ultimately, all transport and metabolic processes in the body are disrupted, immunity and protective forces are reduced. This condition can be compensated by parenteral or enteral administration of exogenous insulin, which compensates for the lack of its own hormone.
Thus, pancreas, performing important functions in our body, contributes to normal digestion and digestion. Maintains blood sugar at a constant level and participates in metabolic processes. When it is damaged, serious disturbances in homeostasis occur, and the level of health and lifestyle decreases. Monitor the condition of the pancreas and do not let the course of possible diseases take their course in order to avoid unpleasant consequences.