What does FGD of the stomach show? FGDS stands for “fibrogastroduodenoscopy”. This procedure is a diagnosis of the organs of the digestive system. To carry it out, a medical device is used - a gastroendoscope. This modern device provides specialists with a reliable, high-quality image of organs located inside the abdominal cavity. Thanks to fibrogastroduodenoscopy, doctors can make an absolutely accurate diagnosis and select appropriate therapy.
Gastroenterologist Mikhail Vasilyevich:
“It is known that for the treatment of the gastrointestinal tract (ulcers, gastritis, etc.) there are special drugs that are prescribed by doctors. But we will not talk about them, but about those medicines that you can use yourself and at home...” Read more >>>
Detailed explanation of the term FGDS
When undergoing FGDS as prescribed, patients often simply call the procedure “gastroscopy.” If it involves examining the esophagus, experts call this procedure “fibroesophagogastroduodenoscopy.” Let us consider in detail how each word of this complex term is deciphered:
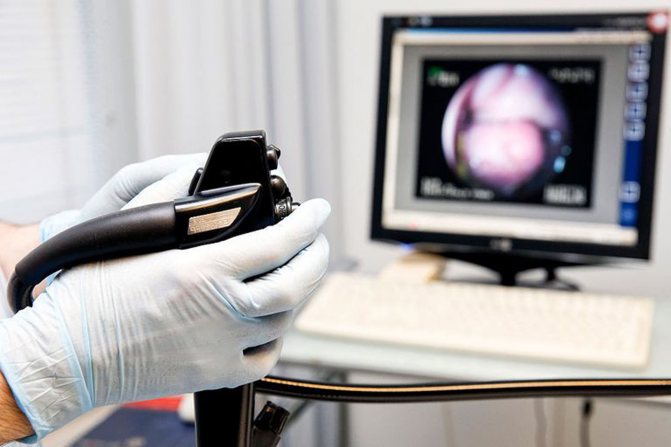
- "Fibro". This word reveals the characteristics of the probe that is used in diagnostics. This probe is made of optical fiber. During diagnosis, a videoscope is also used, the main function of which is to display a video image of the digestive tract organs on the monitor.
- "Gastro". From Greek gastēr, b. n. gastrós - stomach. This part of the word indicates the fact that the procedure is intended to examine the stomach.
- "Duodeno." This part of the word indicates that the duodenum is being examined.
- "Copy". This ending means that the specialist is using a probe to examine the organs located inside the abdominal cavity.
FGDS: what is it?
The abbreviation FGDS stands for fibrogastroduodenoscopy. FGDS is an endoscopic method for examining the condition of the mucous membranes of the esophagus, stomach and duodenum. The examination is carried out by an endoscopist.
A frequently asked question is: is there a difference between FGDS (fibrogastroduodenoscopy) and EGDS (esophagogastroduodenoscopy)? If you follow the terminology, then EGDS includes an additional examination of the esophagus, in contrast to FGDS. However, in reality, if the doctor is qualified and competent in his field, in both cases he will carefully examine all parts of the gastrointestinal tract accessible to inspection. Therefore, there is no difference between FGDS and EGDS for the patient.
What is the purpose of FGDS?
To enlarge the picture, click on it.
Typically, gastroenterologists prescribe fmbrogastroduodenoscopy if necessary to thoroughly examine the mucous membrane of such organs as:
- stomach;
- duodenum;
- esophagus.
This procedure allows specialists to conduct a reliable diagnosis of gastrointestinal diseases. It is prescribed in the presence/suspected presence of the following pathologies:
- peptic ulcer of the stomach, duodenum;
- esophagitis;
- inflammation of the duodenum;
- reflux esophagitis;
- inflammation of the gastric mucosa;
- gastritis (acute, chronic);
- intestinal tumor process.
In addition, this procedure is carried out on the recommendation of specialists for preventive purposes. As a preventive examination, it is necessary for the following categories of the population:
- Having undergone gastric surgery.
- Population over 40 years of age (even without any complaints).
- People who have complaints about problems with the stomach, manifested in the form of nausea, heartburn, flatulence, etc.
- Patients with aggravated analysis, which implies the presence of any cancer in relatives, consumption of spicy food, alcohol, harmful factors at work.
- Having gastroesophageal reflux disease.
- Constantly taking non-steroidal anti-inflammatory drugs, glucocorticosteroids.
* desirable to have
**Patients with diabetes should also not eat food before FGDS. *** Whether or not to take regularly taken medications (for ischemic heart disease, high blood pressure, but not arthritis, osteochondrosis, gastritis... ) before FGDS without harming your health should be agreed with your doctor! As a rule, patients with coronary artery disease and high blood pressure (to prevent exacerbation) are recommended to take medications regularly, and, therefore, before FGDS examination. Warn the endoscopist about the medications you take on the day of FGDS!
Contraindications
The procedure is prescribed by a specialist who must know whether the patient has contraindications to FGDS. Among the contraindications to fibrogastroduodenoscopy, we note:
- vomiting, regurgitation;
- stroke;
- the patient has acute gastrointestinal bleeding;
- heart failure (grade 3);
- presence of signs of intestinal obstruction;
- detected clinical picture of intestinal perforation;
- detection of foreign bodies inside the upper intestines;
- the patient has a tumor in such organs (esophagus, duodenum, pancreas, stomach, biliary tract);
- malformations of the gastrointestinal tract.
Combined diagnostic methods
Testing for Helicobacter pylori
Infection with this microbe is often cited as the cause of peptic ulcers. The presence of Helicobacter pylori also causes gastritis and stomach cancer. The breeding ground for bacteria is the acidic environment of the stomach. Thanks to the gastroscopy technique, it became possible to perform HP testing with an overview of the gastrointestinal tract to select a suitable area for biopsy.
A unique method allows us to detect the fact of urease activity of a microbe that releases carbon dioxide during the breakdown of urea. A biopsy sample is taken during gastroscopy. By the color of the selected material placed in a special environment, the number of bacteria populating it is judged. The rapid test can give the following results:
- three pluses (first hour of the study) – signs of significant infection;
- two pluses (after 2-3 hours) – a sign of moderate infection;
- one plus after a day indicates a weak infection.
The method guarantees quick results without additional costs and special training of specialists. However, a minimal amount of bacteria in the biopsy specimen and gastric bleeding reduce the accuracy of the result.
GASTROSCOPY WITH INSPECTION OF BDS
FGS is often combined with examination of the major duodenal papilla (major duodenal papilla), the location of which is the descending portion of the duodenum. The main task of this small structure is to regulate the flow of bile and pancreatic fluid and prevent intestinal contents from entering the ducts. The use of modern devices guarantees high accuracy of research with the possibility of viewing an enlarged image on the monitor screen. Examination of the gastroscopy increases the time of gastroscopy by a couple of minutes; the manipulation is not painful, but very unpleasant.
Chromoscopy in endoscopy
The method is used to determine during FGDS areas with signs of degeneration of the epithelial layer of the mucosa, accompanied by ulcerations and the appearance of neoplasms. For diagnosis, the mucous membrane is irrigated with dyes that are safe for humans, which stain selected areas of the epithelium with a contrasting color. The study increases the efficiency of diagnosing oncological diseases of the digestive organs; the color test becomes an indispensable addition to the results of biopsy and histology, but increases the duration of the procedure.
SOURCES: https://proskopiyu.ru/gastroskopiya/fgds-nr-chto-eto.html
Proper preparation
To enlarge the picture, click on it.
Preparation for fibrogastroduodenoscopy is considered absolutely simple. The main condition that must be observed is the ban on eating food on the day of the procedure. Experts recommend eating your last meal 12 hours before FGDS. At the same time, dinner must be light. Most often it is porridge (buckwheat) with fish + any vegetable salad.
Before FGDS (2 days in advance), it is undesirable to drink coffee, chocolate, or alcohol. The ban on these products is established for the reason that they linger inside the stomach for a long time. On the day of the procedure, you are allowed to drink, but only 2 hours before the procedure; later it is not allowed.
It is also prohibited before performing FGDS:
- brush your teeth;
- smoking (nicotine can increase gastric secretion, constrict blood vessels, and this may affect the results of the study);
- perform ultrasound of the peritoneum;
- take medication;
- make an injection.
How to prepare for fibrogastroscopy?
The preparatory process for FGDS is not particularly complicated, but it does require careful implementation of all of the above points. Firstly, checking the mucous membranes of the organs should be carried out strictly on an empty stomach - even a small amount of food will cause a copious secretion of gastric juice. This will not only prevent you from getting informative results, but can also cause nausea and even vomiting.
Therefore, the patient needs to check in advance with the doctor or in the diagnostic office how long before the examination he should not eat or drink. As a rule, you need to abstain from food for at least 10–12 hours and from drinking liquids for at least 2 hours. Optimally, if FGS is scheduled for the morning, then the last meal should be no later than 18.00, and in the morning you can drink a glass of still water or weak tea. When preparing for FGS, you should not eat slowly digestible foods - nuts, seeds, chocolate

Dinner on the eve of a gastroscopic examination should be light and quickly digestible, and for 1-2 days before the scheduled examination, you should avoid foods that are slowly digested - chocolate, nuts, seeds. The second important point for a certain group of patients will be an absolute cessation of smoking at least 4–5 hours before FGDS. This is due to an increase in the secretory function of the gastric glands when smoking just one cigarette.
On the day of the examination, in the morning, in addition to the above, you should not brush your teeth or chew gum, as these actions also lead to an increase in the secretion of gastric juice. If the person being examined is taking a course of vital medications, then you must first consult with a doctor about the possibility of stopping them for several hours.
If you have an allergic reaction to the anesthetic used, be sure to report it in advance so that the diagnostician can offer an alternative option. It is also worth warning about possible difficulties with swallowing the endoscope - in such cases, the procedure is carried out under anesthesia.
Features of FGDS
Carrying out fibrogastroduodenoscopy consists of several stages, which we will describe in turn:
- Treatment of the oral cavity with an anesthetic (usually lidocaine is used to irrigate the cavity).
- The patient needs to lie down on the couch (on his left side).
- The patient is given a mouthpiece, which he clamps with his teeth. This precaution prevents damage to the endoscope.
- Insertion of the endoscope. This point is considered the most unpleasant, because at this moment patients often experience gag reflexes and belching.
- Stomach examination. This stage lasts only 5 – 7 minutes.
- Carrying out a biopsy. Material is collected from different places of the epithelium. This biopsy will be needed for histological examination.
In modern clinics, a modification of FGDS can be used. Thanks to the new product, the endoscope is inserted into the stomach through the nasal cavity. This diagnostic method is called transnasal; it has several advantages:
- The level of negative effects on tissue is reduced.
- Gives the patient the opportunity to speak.
- It is convenient to use when diagnosing older people.
- Provides an opportunity to examine the condition of the nasopharynx.
For the convenience of examining organs during a routine FGDS, they are slightly inflated with air. For this reason, during the procedure, after its completion, the patient may experience involuntary belching.
Although the procedure is painless, it still causes discomfort. To reduce the feeling of discomfort to nothing, you need to breathe calmly and evenly. When a piece of tissue is taken from the stomach, duodenum, or esophagus, no pain is felt. This explains the absence of sensory nerve endings inside these organs.
Decoding FGDS
Share information with your Facebook friends
VK
Question:
Hello, Andrey Viktorovich, help me decipher the biopsy.
- Two fragments were taken from the mucous membrane of the antrum of the stomach: the mucous membrane is moderately thinned, the architectonics of the location of the glands is disrupted, and focal hyperproliferation of the integumentary-pit structures is noted. In the lamina propria there is a moderate diffuse focal infiltration of lymphocytes and plasma cells, the stroma is diffusely fibrotic, expanding the glands of the lamina propria with a slight decrease in their number. Groups of glands are identified in which cylindrical cells alternate with a large number of goblet cells.
- Two fragments from the mucous membrane of the body of the stomach: the pit structures are hyperplastic, excessively tortuous, and randomly located. Stroma with pronounced fibrosis and diffuse focal lymphoid infiltration. The glands of the lamina propria are separated by strands of connective tissue, some of them are cystically dilated. Groups of glands are identified in which cylindrical cells alternate with a large number of goblet cells.
Conclusion: 1. The morphological picture corresponds to moderate chronic minimally atrophic diffuse reactive gastritis with foci of intestinal metaplasia of the glandular epithelium. 2. Moderate chronic diffuse inactive gastritis. Hyperplastic polyp with signs of chronic inflammation, with foci of intestinal metaplasia of the glandular epithelium. Helicobacter pylori was not detected. No treatment prescribed. They recommended doing an FGDS in six months. Please tell me what does this mean?
Answer:
Greetings! 1. “The architecture of the location of the glands is disrupted, focal hyperproliferation of integumentary-pit structures is noted” - these are signs of long-term chronic inflammation and tissue irritation either by chemical agents or active substances of neutrophils and lymphocytes. Accumulating in tissue during inflammation. 2. “The stroma is diffusely fibrotic, pushing apart the glands of the lamina propria with a slight decrease in their number” - the effect of inflammation leads not to true atrophy, but to apparent atrophy, due to the spreading of tissues in different directions. 3. “Goblet cells” are signs of small intestinal metaplasia; this may occur in the antrum, but does not cause significant concern. 4. “The glands of the lamina propria are separated by strands of connective tissue, some of them are cystically dilated” - apparently, on this basis they made the conclusion about a hyperplastic polyp, which is not entirely true. In the body, such a picture will most likely correspond to a polyp of the fundic glands. Histology alone is not enough for me. We need a description of the protocol, photos and video materials. But based on the data that exists, I don’t see anything terrible. Control after 3-5 years.
print version
TagsHealth Intestinal polyps FGDS








