Causes
Chronic acalculous cholecystitis (CAC) most often develops as a result of infection entering the gallbladder through the blood and lymph flow (in case of chronic tonsillitis, inflammation of the lungs, uterine appendages, appendix) or from the intestines (in case of development of dysbacteriosis, chronic pancreatitis, colitis, enteritis) . Most often, cholecystitis without stones is provoked by staphylococci, streptococci, enterococci, Escherichia coli, Pseudomonas aeruginosa, and Proteus.
However, an intense inflammatory process begins only if, in addition to the presence of pathogens, there is stagnation of bile in the bladder. Impaired bile outflow, in turn, may be caused by:
- congenital or acquired deformities of the gallbladder;
- prolapse of the abdominal organs;
- pregnancy (the walls of the gallbladder and other abdominal organs are compressed by the uterus);
- surgical interventions;
- endocrine diseases;
- the presence of parasites in the body (ascaris, lamblia and others);
- weak peristalsis of the gastrointestinal tract (GIT).
Factors contributing to the development of chronic acalculous cholecystitis can be a sedentary lifestyle and poor diet, when periods of dieting or fasting alternate with heavy meals.
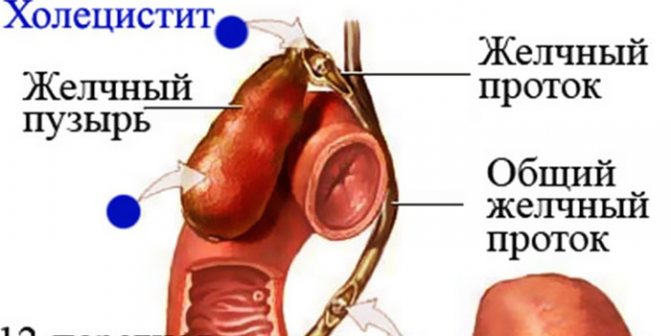
Stagnation of bile in the bladder, changes in its viscosity and qualitative composition create a favorable environment for the development of infectious microorganisms that have penetrated inside. As a result, bacterial inflammation develops, which, as it worsens, causes deformation of the gallbladder and thickening of its walls, thinning of the mucous membrane, and scarring.
According to statistics, chronic acalculous cholecystitis is 4 times more often diagnosed in women than in men
Main reasons
Most often, pathology develops if an infection enters the organ. This usually happens if there is an inflammatory process in the intestines. Then infection of the gallbladder occurs through lymph or blood.
The disease is caused by pathogenic microorganisms such as staphylococci, Proteus, Escherichia coli, enterococci, streptococci.
The disease in adults can occur against the background of other digestive ailments, such as:
- pancreatitis;
- duodenitis;
- bile duct dyskinesia;
- gastritis;
- peptic ulcer;
- hepatitis.
There are other reasons for the development of the pathological condition, due to which bile stagnates in the organ and ducts.
- wall deformations;
- organ prolapse;
- decreased tone;
- impaired outflow of bile.
If the patient has an acute form of the disease, then in the presence of inflammation in the organs of the digestive system, chronic non-calculous cholecystitis begins to develop.
The following factors are identified that provoke the occurrence of a pathological condition:
- period of bearing a child;
- sedentary lifestyle;
- disrupted diet;
- alcohol abuse;
- binge eating;
- excessive body weight;
- use of oral contraceptives;
- taking certain medications;
- presence of parasitic infestations;
- frequent consumption of junk food;
- prolonged fasting;
- improper functioning of the digestive system.
Diabetes mellitus can provoke the development of pathology. An experienced gastroenterologist will help determine the exact cause.
Symptoms
The disease can develop independently or after an attack of acute cholecystitis, and is characterized by a long course with alternating periods of exacerbation and remission.
The main symptoms of chronic acalculous cholecystitis:
- a dull aching pain in the right hypochondrium that occurs after eating (especially when eating fatty or spicy foods, egg dishes, alcohol, carbonated drinks) and persists for several hours or even days;
- spread of pain to the neck, right shoulder or lumbar region;
- heartburn;
- belching;
- bitter or metallic taste in the mouth;
- nausea (appears mainly after eating);
- vomiting (possibly mixed with bile).

Aching pain in the lower back may not indicate problems with the spine, but inflammation in the gallbladder
Sometimes chronic non-calculous cholecystitis occurs latently and is manifested by uncharacteristic syndromes:
Treatment of cholecystitis at home
- neurotic - manifested by suspiciousness, increased anxiety, unreasonable fear;
- vegetative-vascular - there are jumps in blood pressure and increased heart rate;
- cardiac - reflex angina occurs, manifested by dull pain in the heart (this condition occurs after a heavy meal, more often observed in overweight and obese people);
- allergic - develops mainly when the biliary tract is damaged by Giardia, accompanied by recurrent urticaria, which is difficult to treat;
- dyspeptic - there is flatulence, alternation of constipation and diarrhea (impaired fat metabolism, resulting from insufficient production of bile acids, provokes constipation, then a sharp release of bile occurs, causing severe diarrhea).
Acute acalculous cholecystitis is characterized by severe pain, increased nausea, vomiting, and jaundice. In addition to the listed symptoms, signs of intoxication of the body appear. The patient may experience headaches, fever, general weakness and malaise, arrhythmia - increased heart rate (not always). If inflammation spreads to nearby tissues, pericholecystitis develops, pain in the right hypochondrium is intense and constant.
In addition to errors in nutrition, increased physical activity or nervous strain can provoke an exacerbation.
Video
Cholecystitis, inflammation of the gallbladder. Symptoms, diagnosis, treatment.
Chronic cholecystitis is a long-term inflammatory disease of the gallbladder, which is based on a disruption of the process of formation and movement of bile through the ducts, infection of the sensitive mucosa. Treatment of chronic cholecystitis must be coordinated with the condition of neighboring organs, because most often patients have gastritis, duodenitis, pancreatitis or peptic ulcer.
Special restrictions are introduced if the cause of chronic cholecystitis is a previous viral hepatitis.
Treatment of chronic noncalculous cholecystitis differs in the stage of exacerbation and remission in the choice of medications and the nature of nutrition.
Diagnostics
The first diagnostic measures are examination and analysis of the patient's complaints, palpation (when pressing on the area of the gallbladder, acute pain occurs - Murphy's symptom).
To confirm the diagnosis, the patient is referred for a general and biochemical blood test. In the acute form and exacerbation of chronic acalculous cholecystitis, ESR and leukocyte content are increased, deviations from the norm in the quantitative ratio of different types of leukocytes are detected. Biochemical analysis determines changes in the activity of liver enzymes.

If acalculous cholecystitis is suspected, the patient is referred for an ultrasound scan
The main instrumental diagnostic method is ultrasound, which reveals an increase in the size of the gallbladder, thickening of its walls, bending, dyskinesia of the bile ducts with stagnation of bile.
If necessary, additional studies may be carried out:
- gastroduodenal intubation (detects impaired peristalsis of the gallbladder, the presence of infection, increased protein and bilirubin in the bile);
- oral or intravenous cholecystography (determines the size, shape and functional state of the organ);
- arteriography (allows you to study the condition of the cystic artery, determines the thickening of the walls of the organ).
Drug treatment
The choice of treatment regimen depends entirely on the form and course of the disease. If the patient is at the stage of exacerbation of the pathology, then drug therapy is used.
Antibiotics are mandatory to eliminate inflammation and infection in the gallbladder. The following drugs in this group can be used:
- Erythromycin;
- Cefazolin;
- Clarithrosin;
- Ampiox;
- Amoxiclav;
- Ampicillin.
Drug treatment also includes the use of drugs from the following pharmacological groups:
- Antispasmodics (Papaverine, Atropine, Platyfillin, Noshpa, Analgin). They effectively eliminate pain from cholecystitis.
- Enzymes (Festal, Creon, Mezim). These remedies are used to normalize the digestive process.
- Detoxification medications. If the need is expressed, Hemodeza is injected intravenously.
- Antioxidants. Promotes normal bile secretion.
- Anti-inflammatory drugs. Eliminate lesions in the digestive organ.
- Choleretic drugs (Ursohol, Lyobil, Allohol, Ursodez, Cholenzym, Hepatosan). These medications increase the production of bile salts and acid.
- Drugs with a choleretic effect (Holosas, Holagol, Urolesan, Peridol).
Medicines are used that also affect the underlying cause of the disease, for example, antiparasitic drugs are prescribed if necessary.
Complex treatment also includes taking vitamins B and C.
Treatment
Treatment of chronic non-calculous cholecystitis in the acute stage is carried out in a hospital setting, lasting on average 10–14 days. The patient is prescribed:
- broad-spectrum antibacterial drugs in the form of injections (Cefazolin, Cefotaxime) or tablets (Ciprofloxacin, Clarithromycin) - suppress the development of infection;
- Hemodez solution intravenous drip – eliminates symptoms of intoxication;
- antispasmodics (No-shpa, Drotaverine, Papaverine) – relieve spasms of the gallbladder and bile ducts, thereby relieving pain and improving the outflow of bile;
- antiemetics (Cerucal, Metoclopramide) – relieve nausea, suppress the gag reflex;
- choleretics (Allohol, Cholenzym, Cholestil, Flamin) – increase the production of bile by liver cells;
- cholekinetics (Xylitol, Sorbitol, Holosas) - improve the outflow of bile by increasing the tone of the gallbladder and simultaneous relaxation of the muscles of the biliary tract, prescribed to patients with reduced gallbladder function;
- enzyme preparations (Pancreatin, Mezim, Creon) - restore normal digestion.
Additionally, antiparasitic agents may be prescribed (if helminthic infestation is detected), vitamin complexes, and drugs to restore intestinal flora.

For severe inflammation, hospital therapy can last about a month
After relief of acute symptoms of acalculous cholecystitis, therapy is continued on an outpatient basis under the supervision of a gastroenterologist. Twice a year, preventive examinations are carried out, laboratory tests are taken to monitor the functions of the liver and gall bladder.
Treatment of acalculous cholecystitis during remission consists of weekly tubage using xylitol, sorbitol, magnesium sulfate (prescribed for decreased biliary tone). A full course includes an average of 6–8 procedures. Sanatorium-resort treatment with mineral waters is effective (Essentuki, Zheleznovodsk, Truskavets).
Treatment of chronic acalculous cholecystitis
As a rule, treatment of chronic acalculous cholecystitis is carried out using conservative methods. Dietary nutrition is recommended: frequent meals in fractional portions; fatty, fried, spicy foods, carbonated drinks and alcohol should be excluded from the diet.
DRUGS FOR PAIN. If abdominal pain occurs, antispasmodics (platiphylline, drotaverine, papaverine, etc.) are prescribed to treat the disease. During periods of exacerbation of the disease and its combination with cholangitis, the doctor prescribes antibacterial therapy with drugs that have a wide spectrum of action (cefazolin, amoxicillin, erythromycin, ampicillin, furazolidone, etc.), taking into account the microflora isolated from the bile.
DIGESTIVE DRUGS . To normalize digestion, it is recommended to take enzyme preparations (Pancreatin, Mezim-Forte, Festal). To enhance bile secretion, it may be necessary to take choleretics (cholenzyme, allochol, oxafenamide). In order to stimulate contraction of the gallbladder, cholecystokinetics (sorbitol, magnesium sulfate) are prescribed.
PHYTOTHERAPY . It is advisable to conduct courses of herbal medicine during periods of exacerbation and remission of the disease, for which it is recommended to take decoctions of mint, chamomile, rosehip, calendula flowers, licorice, etc. Outside of exacerbation, it is advisable to perform blind tubing, treatment with mineral waters, and exercise therapy.
OPERATION . Surgical treatment of chronic acalculous cholecystitis is recommended for persistent disease, severe deformation of the gallbladder, pericholecystitis, “disabled” gallbladder, associated cholangitis and pancreatitis, which cannot be treated. In such situations, cholecystectomy (open, laparoscopic or mini-access) is provided.
Diet
Successful treatment of chronic acalculous cholecystitis is possible only if you follow a diet. Necessary:
- eat at the same time, in small portions, often (4-6 times a day, the last time - 2 hours before bedtime), in small portions, do not overeat;
- eat food boiled, steamed, baked, heated (cold foods and drinks can cause spasm of the sphincter, which regulates the flow of bile);
- include in your daily diet protein omelettes, boiled or baked vegetables, cereal dishes, vegetable broth soups, compotes and jelly;
- exclude from the menu fatty, fried, spicy, nuts, baked goods, raw vegetables and fruits, dishes with eggs (yolk), carbonated drinks, alcohol;
- spend fasting days on fermented milk products.
Nutrition for chronic acalculous cholecystitis
After identifying chronic acalculous cholecystitis, it is necessary to adhere to certain rules in the diet and diet composition both during periods of exacerbations of the disease and outside of exacerbations.
- Nutrition for chronic acalculous cholecystitis should consist of frequent meals (4 to 6 times a day) and include fractional portions, so that the gallbladder will be emptied regularly.
- Spicy, fatty, fried foods, carbonated drinks, beer, wine, egg yolks, baked goods, nuts, cold dishes, raw fruits and vegetables, cream should be excluded from the diet.
- During periods of exacerbation, food should always be freshly prepared and warm. Dishes can be steamed, baked or boiled.
- Outside of exacerbations, it is recommended to include vegetables in the diet (carrots, beets, watermelon, melon, raisins, prunes, dried apricots), since they help restore gallbladder function and eliminate constipation.
- Fractional therapeutic nutrition should be observed by the patient for a long time, for years.
Folk remedies
Treatment of non-calculous cholecystitis with folk remedies involves the use of decoctions and infusions of medicinal herbs that help dilute bile and improve its outflow, reduce inflammatory processes and suppress infectious flora.

You can purchase a ready-made choleretic mixture at the pharmacy.
Most often, for non-calculous cholecystitis, infusions of yarrow, immortelle, corn silk, and tansy are used. The method of preparation is the same in all cases: pour a tablespoon of plant material into a glass of boiling water, leave, strain. Take ½ glass three times a day before meals. The treatment course is 20–30 days.
Treatment with folk remedies should be carried out only during remission.
Possible complications and prognosis
The outlook for the disease is mostly favorable. However, if the disease is advanced and treatment is ignored, complications may develop such as:
- hepatitis;
- cholelithiasis;
- cholangitis in chronic form;
- empyema.
Also, with frequent exacerbations, a bag filled with pus may form in the bladder. In the future, it can break through the wall of the organ (there will be a perforation), which will lead to more dangerous complications.
There are many causes of non-calculous cholecystitis. Treatment depends on the form of the disease and the severity. Proper nutrition in this case is both an obligatory part of therapy and a measure to prevent pathology.
Complications
The mild form of noncalculous cholecystitis responds well to conservative therapy. But if the disease is not treated, the inflammation worsens and the frequency of exacerbations increases. This can lead to the development of dangerous complications:
- reactive hepatitis;
- chronic cholangitis;
- stone formation;
- epiema (formation of a purulent sac in the cavity of the gallbladder);
- perforation (violation of integrity) of the walls of the gallbladder with the subsequent development of peritonitis;
- gangrene of the gallbladder.

Complications of acalculous cholecystitis are more dangerous than the disease itself and can lead to the need for urgent surgical intervention
Acute cholecystitis

This disease is characterized by acute inflammation of the gallbladder. In this condition, damage to the wall of the gallbladder occurs and a change in the normal properties of bile.
Causes of acute cholecystitis
The formation of acute cholecystitis results from a sudden disruption or cessation of bile outflow. This condition appears when the gallbladder duct is blocked (obstructed) by a calculus, a clot of mucus, or a spasm of the sphincter of the duct itself.
In 90–95% of cases, acute cholecystitis develops as a complication of cholelithiasis (GSD).
Mechanism of inflammation development
When bile stagnation occurs, its composition changes. In the cavity of the gallbladder, the intensive development of the infectious process begins with the participation of bacteria, sometimes viruses or protozoa. Infectious agents usually penetrate into the gallbladder from the duodenum, less often from the liver, through the blood or lymph.
As a result of increased bile pressure in the gallbladder, the vessels of its walls are compressed, which leads to impaired circulation and the development of acute purulent inflammation up to necrosis (cell death).
Classification
Acute cholecystitis due to its occurrence is divided into:
- Acute calculous cholecystitis, resulting from obstruction by a calculus in cholelithiasis (from the Latin calculus - calculus, stone).
- Acute non-calculous cholecystitis (calculous).
- Acute cholecystitis has three stages of development. In the absence of treatment, a transition to a more severe stage occurs.
- Acute catarrhal cholecystitis. Only the mucous and submucous membranes of the gallbladder are affected.
- Phlegmonous cholecystitis. There is purulent damage to all the walls of the gallbladder.
- Gangrenous cholecystitis. Foci of necrosis of the gallbladder wall appear. This stage is dangerous due to a serious complication - perforation (the appearance of a through defect) of the gallbladder wall. In this case, infected bile leaks into the abdominal cavity and peritonitis (inflammation of the peritoneum) occurs, which is a life-threatening condition.
Symptoms

Acute cholecystitis is characterized by fairly pronounced manifestations, the intensity of which depends on the degree of damage to the gallbladder.
Catarrhal acute cholecystitis
The main sign of acute cholecystitis is the appearance of pain in the right hypochondrium. Often the pain spreads to the lower back, right shoulder blade, shoulder, and neck. It is immediately paroxysmal and later becomes permanent.
Nausea and vomiting occur, which does not bring relief. Body temperature is slightly elevated. Increased heart rate - tachycardia - may occur.
Phlegmonous acute cholecystitis
With further progression of the disease and its transition to the phlegmonous form, the severity of pain increases noticeably. It intensifies when changing the location of the body, breathing, or coughing. Vomiting becomes repeated. Body temperature increases even more.
Gangrenous acute cholecystitis
If the disease progresses to the stage of gangrenous cholecystitis, a picture of severe intoxication and local peritonitis appears. And with perforation of the gallbladder, which is a common complication at this stage, signs of diffuse peritonitis appear.
The condition noticeably worsens, the intensity of pain increases. It takes on a diffuse character. Sometimes, when pain receptors are damaged, pain may disappear - an “imaginary” improvement. Body temperature is high. Breathing is frequent and shallow. Tachycardia increases. The abdomen is swollen and does not participate in the act of breathing. Positive symptoms of peritoneal irritation are revealed.
Gangrenous cholecystitis often occurs in older people. However, their manifestations of the disease are usually erased, which makes it difficult to identify.
Diagnostics

Palpation of the abdomen reveals sharp pain in the right hypochondrium. Sometimes, especially in patients of thin build, an enlarged and painful gallbladder is palpable. A general blood test reveals an increase in the number of leukocytes (leukocytosis) and ESR.
The severity of the changes is determined by the degree of damage to the gallbladder.
Biochemical blood tests often reveal signs of cholestasis.
To clarify the diagnosis, ultrasound, CT and MRI, endoscopic methods, radiography and others are used. In particularly severe or doubtful cases, laparoscopy is performed.
Prevention
It is not always possible to prevent the development of the disease, but by following preventive measures you can achieve stable remission, avoid exacerbations and the development of complications. For this it is important:
- control and, if necessary, normalize weight;
- follow a diet and nutrition regimen;
- drink at least 2 liters of liquid daily;
- give up a sedentary lifestyle, ensure daily physical activity, but do not overexert yourself;
- consult a doctor in a timely manner and treat the acute stage of the disease, as well as other gastrointestinal pathologies, infections, helminthic infestations;
- undergo regular preventive examinations for chronic pathology.
Non-calculous cholecystitis is a serious disease, dangerous for its complications. The initial stages of the disease are easy to treat. It is much more difficult to treat advanced forms of the inflammatory process. Only a timely visit to a doctor and competently administered therapy, a healthy lifestyle and strict adherence to medical recommendations during periods of remission will help to avoid the development of serious consequences.
What it is?

In Russian medical practice, non-calculous cholecystitis is understood as a chronic, slowly progressive inflammation of the gallbladder tissue, associated with a functional impairment of its motility and peristalsis, but not accompanied by the typical formation of stones.
The most common functional disorders associated with noncalculous cholecystitis are dyscholia and dyskinesia.
Treatment of the disease
In case of severe exacerbation of non-calculous cholecystitis, treatment is carried out in a hospital. The goal of therapy is to relieve exacerbations, prevent and treat complications. Conservative therapy is usually sufficient. Surgical interventions are performed in cases of frequent and severe exacerbations, severe deformation of the gallbladder and ineffective use of medications.
Our readers recommend!
For the prevention and treatment of diseases of the gastrointestinal tract, our readers advise
Monastic tea
. This is a unique product that includes 9 medicinal herbs useful for digestion, which not only complement, but also enhance each other’s actions. Monastery tea will not only eliminate all symptoms of gastrointestinal and digestive diseases, but will also permanently eliminate the cause of its occurrence.
Readers' opinions..."
Diet food
Therapeutic diet is one of the main components of the treatment of chronic acalculous cholecystitis. To regulate the secretion of bile from the bladder, food should be taken in small portions 4-6 times a day. The following foods are completely excluded from the diet during an exacerbation:
TREAT THE CAUSE, NOT THE EFFECT!
Nutricomplex,
a product made from natural ingredients, restores proper metabolism in 1 month. Read the article>>...
- fatty, spicy, fried foods;
- beer, wine and other alcoholic drinks;
- egg yolks;
- baked goods;
- nuts;
- raw vegetables and fruits;
- sparkling water.
Food should be warm, as cold dishes can lead to spasm of the sphincter of Oddi, which is responsible for the secretion of bile. Dishes should be steamed, baked, stewed or boiled. The menu includes steamed egg white omelettes, stewed and baked vegetables, cereal soups in vegetable broth, jelly, and compotes. During the remission phase of non-calculous cholecystitis, the diet can be expanded, but the basic principles of nutrition should be followed for a long time, sometimes for years. More information about nutrition for this disease can be obtained from the article: List of permitted and healthiest foods for cholecystitis.
Medicines
Drug treatment of chronic acalculous cholecystitis is aimed at solving the following problems:
- elimination of pain syndrome;
- restoration of motility and tone of the biliary tract;
- suppression of the inflammatory and infectious process in the gallbladder;
- normalization of impaired digestion.
Usually, for non-calculous cholecystitis, antispasmodics, antibiotics, and agents that normalize the motility of the gallbladder and intestines are used. In case of severe intoxication, infusion therapy is carried out. If cholelithiasis is excluded during the examination, it is possible to use choleretic agents based on ursodeoxycholic acid.
IMPORTANT!
How to remove bags and wrinkles around the eyes at 50 years old? Read the article>>...
Enzyme preparations are indicated to normalize the digestion process. For exacerbations of acalculous cholecystitis, treatment takes about 2 weeks, but with the development of complications it can be longer. After eliminating acute phenomena, the doctor may prescribe physiotherapy that will improve the contractile activity of the gallbladder.
Phytotherapy
To maintain remission of chronic non-calculous cholecystitis, treatment with herbal remedies is useful.
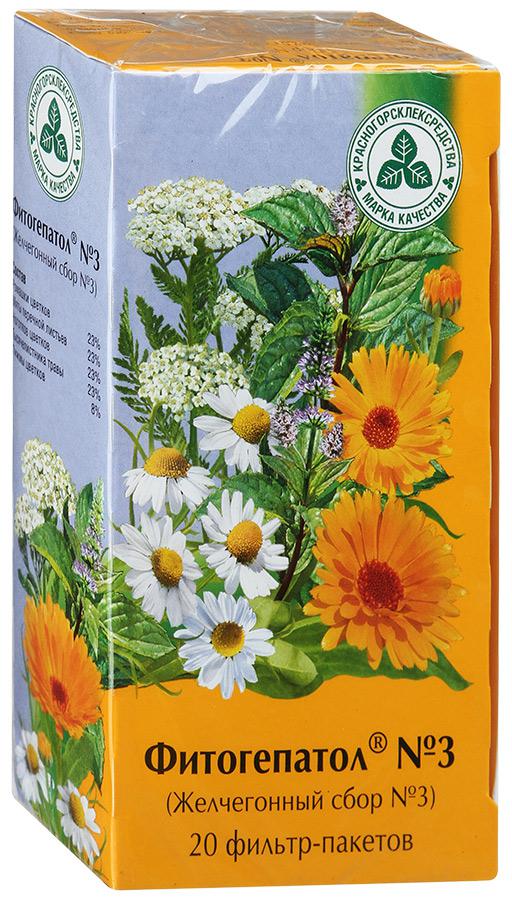
Pharmacies sell ready-made choleretic preparations, which are very convenient to use.
To improve bile secretion and reduce the inflammatory process, decoctions of tansy, yarrow, licorice, buckthorn and other medicinal plants are used.
Important: before using any of the presented treatment methods, you should consult your doctor.
Several traditional medicine recipes for the treatment of acalculous cholecystitis:
But perhaps it would be more correct to treat not the effect, but the cause?
We recommend reading the story of Olga Kirovtseva, how she cured her stomach... Read the article >>
Article rating:
(votes:
, average rating:
out of 5)
All materials on the website ozhivote.ru are presented for informational purposes only, contraindications are possible, consultation with a doctor is MANDATORY! Do not engage in self-diagnosis and self-medication!
This diagnosis is made when inflammation of the walls of the gallbladder is detected, but stones do not form in it (unlike calculous cholecystitis). Young people and even children are not immune from this disease. Moreover, acalculous cholecystitis affects women four times more often than men. The disease requires serious and long-term treatment.
Why does acalculous cholecystitis develop?
Carrying out statistical analyses, doctors note that in most cases, the non-calculous type of disease is the result of infection of the gallbladder. Pathogenic bacteria, along with blood or lymph, enter it mainly through the intestines. For example, if a person suffers from periodontal disease, tonsillitis or colitis. However, bile has powerful bactericidal properties. The infection causes inflammation when the secretions stagnate. This occurs when the motor function of the organ is impaired, since the outflow of bile is hampered.
The risk group causing non-calculous cholecystitis includes people with the following bad habits, conditions or pathologies:
- deformation of the gallbladder;
- prolapse of organs located in the abdominal cavity;
- last trimester of pregnancy;
- physical passivity, immobility;
- diets for weight loss;
- alcoholism;
- hormonal drugs;
- endocrine diseases.
As the non-calculous type of inflammation of the bile producing bladder progresses, the organ becomes deformed. Sometimes to such an extent that it forms adhesions with nearby intestines. In most cases, this disease is accompanied by other inflammations of the digestive tract. As a result, the acute non-calculous process becomes chronic. With a protracted course of the pathology, doctors classify the non-calculous type of disease as either typical or atypical. In the second case, intestinal, esophageal and cardiac forms of the disease may occur.

Signs of cholecystitis without stone formation
The non-calculous type of disease has very characteristic symptoms. Often these signs are pronounced. With non-calculous cholecystitis, a person feels that every time in the depths of the right hypochondrium he has a dull pain after eating. Especially after fatty foods. Moreover, pain with cholecystitis radiates either to the neck, then to the shoulder or back. The second typical symptom that distinguishes a non-calculous inflammatory process in the gallbladder is belching, heartburn, and an unpleasant taste of bitterness. The third classic symptom is nausea after eating.
Other diagnostically no less important symptoms of cholecystitis, characteristic of atypical forms of the disease:
- flatulence;
- stool instability (either diarrhea or constipation);
- vomiting, often with bitter masses due to bile;
- rise in temperature;
- heart pain, tachycardia.
Non-calculous cholecystitis is finally diagnosed after laboratory tests and instrumental examination. An ultrasound helps determine whether there are stones in the gallbladder. The cholegraphy method, performed using x-rays, allows you to determine whether a non-calculous inflammatory process is developing. However, this type of examination is not prescribed during periods of pregnancy or exacerbation of the disease. Blood and stool tests are required.

How to treat cholecystitis
First of all, the patient must be provided with bed rest. Acute and chronic acalculous cholecystitis should be treated by strictly following the instructions of the gastroenterologist. It is necessary to comprehensively solve the following problems:
- Alleviate the patient's condition by eliminating painful colic.
- Eliminate stagnation of bile.
- Extinguish the non-calculous inflammatory process in the bladder.
These goals can be achieved using the following therapeutic methods:
- therapeutic diet;
- drug therapy;
- physiotherapeutic procedures;
- herbal medicine;
- hydrotherapy.
How is exacerbation of cholecystitis treated?
If the patient's chronic illness history is replete with frequent episodes when a non-calculous type of illness is activated, hospitalization is necessary. Strict bed rest and refusal to eat for several days are prescribed. Drinking should be moderate, in small portions, so as not to provoke vomiting. The patient is given a complex of medications (tablets, injections). Later, when non-calculous, chronic cholecystitis passes the acute phase, electrophoresis and mud applications are used. In case of suppuration or blockage of the bile duct, the organ is urgently removed.

Medicines
Drug therapy is complex. For non-calculous cholecystitis, drugs from the following groups are used to eliminate pathology:
- analgesics that eliminate painful colic - Ketonal, Baralgin, Sedalgin;
- antibiotics – Ampicillin, Rifampicin, Erythromycin;
- antispasmodics, relaxing bile ducts - No-shpa, Papaverine, Platiphylline, Atropine;
- antiemetics - Cerucal, Ondansetron, Motilium;
- choleretic drugs for cholecystitis - Hologon, Cholenzym, Nikodin, Tsikvalon;
- enzymes that activate the motility of the digestive tract - Mezim Forte, Festal, Creon, Panzinorm;
- probiotics that restore beneficial intestinal microorganisms - Linex, Bifiform, Bifidumbacterin, Enterol, BioFlora.
Diet
Therapeutic nutrition is the most important condition for getting rid of this disease. Acute non-calculous inflammatory process requires a gentle diet. Warm liquid soups, cereals, and jellies are prescribed. Gradually pureed meat, fish, dairy, vegetable and fruit dishes are included in the diet. If a patient develops a non-calculous type of inflammation of the gallbladder, it is necessary to eat food often, but in small portions.
Should be permanently excluded:
- fatty, fried foods;
- spicy seasonings;
- egg yolks;
- nuts;
- raw vegetables and fruits;
- baked goods;
- any alcoholic and carbonated drinks.

Traditional treatment
Medicinal plant preparations are gentle and have minimal side effects. Infusions and herbal decoctions are good for treating non-calculous types of bladder damage. Folk remedies dilute stagnant bile and activate its outflow. In addition, they suppress the development of infection and relieve non-calculous inflammatory process. However, such drugs can be used only after cholecystitis has passed the acute stage. They should not be used during pregnancy or given to a small child.
Warm herbal infusions are often taken. Brew 8-10 g of dry raw material with a glass of boiling water and drink half a glass three times a day before meals for 3-4 weeks. Particularly popular:
- corn silk;
- parsley herb;
- immortelle flowers.
Complications
With delayed or inadequate treatment of this disease, the following may develop:
- hepatitis;
- cholelithiasis;
- cholangitis;
- empyema (suppuration), perforation (rupture), gangrene of the gallbladder.
Video
A favorable prognosis for this disease is possible only if the patient is treated adequately and in a timely manner. As a result of complex therapy, the patient completely restores his ability to work. The maximum danger with cholecystitis is complications, sometimes leading to rupture of the gallbladder.
What is chronic cholecystitis
The calculous form of the disease is an inflammation in the area of the gallbladder, which occurs due to the deposition of stones in it. Dense masses consist of impurities of calcium, cholesterol, and bile dyes. Gallbladder stones cause problems with the outflow of bile and impair blood supply to the walls of the organ, as a result of which numerous substances begin to leak out of it, triggering the inflammatory process. Over time, this pathological process is complemented by the proliferation of bacteria.
Chronic calculous cholecystitis periodically worsens, and the patient experiences jaundice and colic. Unlike this form of pathology, non-calculous is not associated with stone formation, but can also be chronic or acute. Inflammation of the gallbladder can be caused by bacteria, viruses, or parasites. Calculous cholecystitis is characterized by a chronic course, which periodically alternates with exacerbations and remissions. Experts take into account the number of alternations of these periods per year for a particular patient and determine the severity of the pathology:
- severe cholecystitis;
- moderate calculous cholecystitis;
- mild form of cholecystitis.
Why does calculous cholecystitis develop?
The main reason for the development of inflammation of the gallbladder is the formation of stones in the lumen of the organ. Stones occur as a result of changes in bile levels, as a result of which cholesterol crystallizes and causes stagnation of secretions. Stones with a high degree of probability can be formed due to a violation of the outflow of bile (stagnation of this substance): this leads to the fact that the walls of the gallbladder begin to become inflamed. Stones in the organ occur due to:
- excess consumption of carbohydrates, fats;
- vitamin deficiency;
- long-term adherence to strict diets;
- passive lifestyle;
- acute viral hepatitis;
- helminthiases;
- pancreatitis;
- Crohn's disease;
- chronic gastritis;
- cholecystopancreatitis;
- liver cirrhosis;
- biliary dyskinesia;
- endocrine disorders, which are facilitated by diabetes mellitus, treatment with hormonal drugs, obesity, menopause, etc.;
- hereditary predisposition.

Signs
With a calm course of chronic calculous disease, the symptoms are mild. Patients with cholecystitis usually complain of:
- Aching pain in the peritoneal area. The symptom is localized in the area of the right hypochondrium, and it can be permanent or occur 1-3 hours after eating fatty, fried foods.
- Pain syndrome in the upper body. Patients feel pain near the right shoulder blade, neck, right shoulder. Sometimes sharp pain may occur, as during an attack of biliary colic, but this symptom quickly passes.
- Nausea, insomnia, irritability.
To confirm the diagnosis, the doctor performs an ultrasound, which is the main method of examining patients with suspected inflammation of the bile duct. Echo signs:
- reduction/increase of bubble;
- thickening of the organ walls by more than 3 mm;
- deformation of the external and/or internal contours of the gallbladder;
- the presence of heterogeneous fixed or free-floating inclusions;
- three-layer wall (characteristic of a pronounced exacerbation of chronic calculous cholecystitis).

Exacerbation
During the exacerbation phase of calculous disease, the patient experiences additional symptoms. Signs of this are:
- dizziness;
- acute pain near the liver, radiating to the sternum, shoulder or shoulder blade;
- weakness;
- slight increase in body temperature;
- vomiting, severe nausea;
- abdominal spasms;
- bloating;
- constipation or intestinal disorders.

How to treat chronic cholecystitis
The doctor chooses treatment based on the form and severity of the pathology. Acute calculous cholecystitis requires hospital treatment, while self-medication at home is unacceptable and very dangerous. Conservative treatment includes taking certain types of medications: the patient simultaneously drinks antispasmodics, choleretic, detoxification, and antiemetic drugs. When the patient's condition has stabilized, cholecystectomy or laparoscopic surgery is prescribed (the doctor can remove only the stones or the entire gallbladder).
Is cholelithiasis treated with folk remedies?
It is impossible to cure chronic calculous cholecystitis, but traditional medicines can help reduce the intensity of symptoms. For this purpose, various herbs that have a choleretic effect are used. Decoctions and infusions are prepared from them, which help relieve inflammation from the gallbladder and eliminate the stagnant processes that occur in it. The following recipes for folk remedies are recommended to be used periodically to prevent exacerbation of chronic cholecystitis in order to avoid organ removal.
- Decoction of immortelle flowers. Pour boiling water (80 ml) over dried flowers (15 g), keep the liquid in a water bath for no longer than half an hour. When the decoction for chronic cholecystitis has cooled, take it twice a day before meals, 2 tbsp. l.
- Infusion of lingonberry leaves for calculous cholecystitis. Add 3 tbsp. l. raw materials into a thermos, fill with barely boiling water (1 liter) and wait 8-10 hours. Afterwards, you can start taking folk medicine, and it is recommended to drink the infusion during the day as tea, and prepare a fresh portion the next day.

How to treat chronic cholecystitis
Drug treatment helps to temporarily eliminate the symptoms of cholecystitis, and chronic pathology can be completely cured only in the surgery department by removing the gallbladder (for this purpose, a laser, chemical litholysis method, laparoscopy, abdominal surgery, etc. can be used). Conservative treatment involves taking the following medications:
- Antibiotics. If the patient experiences an increase in temperature and leukocytosis, the doctor prescribes a 7-10-day course of antibiotic therapy, while taking macrolides (Azithromycin), penicillins (Amoxicillin), cephalosporins and gentamicin (the last two are given intramuscularly in a hospital setting). In addition, in the presence of Giardia, Furazolidone or Metronidazole is used. If a patient with calculous type cholecystitis exhibits inflammatory symptoms, broad-spectrum tablets are prescribed.
- Choleretics. These drugs stimulate the formation of bile, the lack of which leads to disruption of the digestive process. Such drugs prevent the formation of stones, liquefy bile masses and are used, as a rule, during an exacerbation of calculous chronic cholecystitis, when the ducts of the bladder are clogged. The doctor can prescribe Odeston, Tsikvalon, Oxafenamide and other choleretics that have an antispasmodic effect to the patient.
- Antispasmodics. To relieve unpleasant symptoms (spasms, colic), drugs such as No-shpa, Platifillin, Atropine, Drotaverine, Duspatalin, etc. are prescribed. However, ordinary painkillers such as Ibuprofen or Aspirin for cholecystitis do not give the expected effect.
- Cholekinetics. Cleanses the gallbladder from accumulated excess bile. For this purpose, they take the drugs Lutkens, Oddi, vegetable oils, magnesium sulfate, synthetic hormones (Choleritin, Pituitrin, Cholecystokinin).
- Enzymes with bile. If a patient with cholecystitis has concomitant pancreatitis, the doctor prescribes Cholenzym or Festal to improve digestion.
- Drugs that help dissolve stones. During the period of subsiding inflammatory process, taking Litofalk, Urosan, Henofalk may be indicated.
- Vitamin complexes. For the treatment of chronic calculous cholecystitis, it is recommended to take vitamins B and C.

Diet during exacerbation
The main requirement of a therapeutic diet is fragmentation (the patient should eat 5-6 times a day, taking short breaks). Portions for calculous cholecystitis should be small, and the diet should be healthy and balanced. Evening meals are completely excluded. Protein, carbohydrate and fat-containing foods should be consumed in accordance with dietary requirements. Thus, the amount of animal fats in the menu is reduced (during exacerbations they are completely excluded), they are compensated by vegetable fats, which are better broken down by bile and improve cellular metabolism of the liver.
Thanks to vegetable fats, the volume of bile mass production increases and the risk of stone formation decreases. During a diet for chronic cholecystitis of the calculous type, it is recommended to include the following products in the diet:
- lean meat (poultry, except duck, rabbit, beef), fish;
- vegetables fruits;
- porridge (buckwheat and oatmeal are the healthiest);
- a large amount of liquid, including still mineral water, herbal decoctions, homemade compotes, jelly (the daily volume should be 2000 ml).
For calculous chronic cholecystitis, exclude the following foods:
- spices;
- spicy dishes;
- smoked;
- sausages;
- fried, fatty foods;
- canned food and products with preservatives (mayonnaise, ketchup, store-bought juices, pickles, etc.);
- nuts;
- meat/fish broths;
- baked goods, sweets;
- strong tea, any coffee;
- cold drinks, soda;
- egg yolk;
- liver, brains;
- lamb
Video
Chronic noncalculous cholecystitis can cause serious complications. For example, if treatment is not started in a timely manner, a person may develop hepatitis, cholelithiasis, or cholangitis in a chronic form. The most dangerous of all complications is considered to be perforation (rupture) of the membrane of the gallbladder and, as a result, entry of bile into the abdominal cavity. As a result, peritonitis develops, and pus accumulates in the bile reservoir. Among other things, the patient is not immune from gallbladder gangrene in the event of an advanced stage of acalculous cholecystitis.