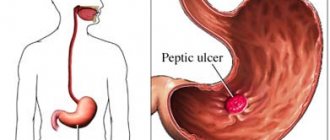
With pancreatitis, there may be blood in the stool
Pancreatitis is a serious disease caused by inflammation of the pancreas.
The disease is not local in nature, the whole body suffers from it. This cunning disease spares no one and often leads to serious complications, one of which is bleeding. Heavy bleeding in the acute form of the disease does not occur so often. But their appearance is evidence of a serious malfunction in the body, which can lead to death.
The cause of this phenomenon may be arrosion, or corrosion of the walls of blood vessels that are located in the pancreas area. Hemorrhage occurs in the space behind the peritoneum, in the lumen of the gastrointestinal tract or peritoneal cavity.
What kind of stool does an adult have with pancreatitis?
When a disease such as pancreatitis develops in a patient, the stool masses acquire a porridge-like consistency or liquid form. Feces are excreted in small portions, and they may contain fragments of undigested food, in particular meat and fiber. If fats are present in the feces, they acquire a foamy liquid consistency and can be released more than three times a day. This is due to the fact that the inflamed pancreas is not able to fully generate enzymes that take an active part in food processing processes.
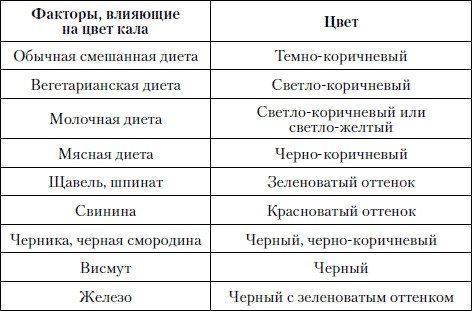
The color of stool during the development of pancreatitis may change depending on the severity of the pathology:
- As the disease worsens, feces acquire a dirty gray or pearlescent hue.
- If the patient adheres to a mixed diet, then his stool will have a brown tint.
- Yellow stool does not occur with pancreatitis. This color of feces is observed in babies who are breastfed.
- Greenish-colored stool masses are observed in the chronic form of the pathology.
- Feces can become very light in color, even white, due to the accumulation of large amounts of bile in the gland.
Each person can suspect the development of pancreatic pathological conditions based on the following signs:
- feces acquire a viscous consistency and begin to stick to the walls of the toilet;
- feces give off a fetid, putrid odor;
- the person has bloating;
- colic and belching appear;
- severe heartburn;
- constant nausea appears;
- vomiting begins;
- there is constant flatulence.
What can stool analysis show?

After a person notices changes in feces and the manifestation of symptoms characteristic of pancreatitis, he should go to a hospital for consultation. The specialist will examine him and collect an anamnesis of the pathology. But to confirm the preliminary diagnosis, the patient will have to undergo tests, in particular feces.
The following changes will indicate malfunctions of the pancreas:
- Smell . It becomes more smelly and intense. This is caused by putrefactive processes occurring in the intestinal lumen.
- Consistency . With pathological processes in the pancreas, stool acquires a more liquid structure. Their consistency resembles gruel with grains. Feces become lighter and can be easily flushed from the toilet. The composition contains undigested food fragments.
- Colors . If a person has the initial stage of development of pancreatitis, then his stool masses will become grayish or olive-colored.
- Frequency of bowel movements . Patients begin to defecate more often, but at the same time the portions of feces will become smaller in volume.
Pancreatic cancer
Pancreatic cancer (carcinoma) can cause blood to appear in pancreatitis. It is very difficult to detect it, so it is necessary to undergo the necessary diagnostics at the slightest hint of the disease. This form of cancer is very aggressive and acting quickly can save lives.
The development of pancreatic cancer is caused by:
- smoking;
- alcohol;
- food poor in fresh fruits and vegetables;
- hereditary predisposition;
- chronic pancreatitis;
- diabetes.
Symptoms of pancreatic carcinoma include: constipation, weakness, general fatigue. In 90% of patients, the disease manifests itself as pain and jaundice. The pain is excruciating, localized either in the back or in the upper left corner of the abdomen.
Jaundice may be accompanied by dark urine, itching, and light-colored stool. Yellowness of the skin and whites of the eyes appears as a result of bile entering the blood. This happens because the tumor blocks the bile duct. This is also the cause of itching all over the body.
With cancer, a large amount of fatty acids enters the feces and is excreted from the patient's body. This leads to a sharp weight loss against the backdrop of a good appetite.
Since the tumor puts pressure on the stomach and duodenum, severe attacks of nausea and vomiting occur.
Treatment for pancreatic carcinoma
The problem is corrected surgically. This is the only way to save the patient. The clinic performs pancreatic resection and subsequent chemotherapy.
Other treatments may be aimed at relieving some symptoms. Pain is relieved by:
- painkillers;
- chemotherapy and radiotherapy.
Folk remedies
To choose the right non-drug treatment, you should take into account: the presence of metastases, the severity of the condition, the stage of development of the disease, etc. With this knowledge, you can begin to select decoctions and tinctures. Golden mustache, wormwood, potato flowers, calendula, beet juice, etc. have a beneficial effect.
Nutrition
Particular attention should be paid to the heat treatment of products. Food should be steamed, baked or boiled. Food should be chopped before serving to the patient.
Products allowed for consumption are only those that are easily absorbed by the body. Therefore, fatty foods are completely excluded.
The ideal dish would be puree soups. They have the right consistency and are easily digestible. They can include vegetables and saturate the body with useful vitamins and microelements.
The menu must include protein-rich lean meat, but only well-chopped in a blender. Low-fat fermented milk products in small quantities will also be useful.
Various cereals, but well boiled ones, will also support the body. They can also be added to soups.
Pancreatitis is one of those diseases that may not manifest itself for a long time, thereby complicating the process of subsequent treatment. However, there are a number of signs by which an attentive person can detect certain changes in his body and respond to them in time. One of these signs is stool.
Feces with pancreatitis change quite a lot, so it is important to pay attention to this and consult a doctor, even if there is nothing else to worry about. If you doubt whether the appearance of feces is normal, you can always find a photo on the Internet and compare. If the pancreas malfunctions, the stool becomes liquefied, does not come out immediately, but in small parts, and contains undigested food particles, which indicates a lack of enzymes.
There are quite a lot of options for the shape and consistency of stool with pancreatitis, but we can highlight those that are most common:
- Thin and long, resembling a ribbon. This option indicates problems with the sigmoid colon and tumor processes.
- The so-called "sheep's balls", indicating the presence of constipation and ulcers.
- Unshaped chair.
Changes in stool substance
The main sign of the development of a pathological process in the pancreas is the appearance of pain in the hypochondrium, 50-60 minutes after eating fatty, salty, sweet, spicy or fried foods. After which, the development of the following symptoms may be observed:
- the contents of the intestines begin to ferment;
- gas accumulation occurs, which causes intoxication;
- bloating appears in the abdominal area;
- diarrhea occurs.
If no measures are taken to eliminate the pathology, then structural changes in the pancreas can lead to death. Laboratory researchers pay special attention to the color of stool during pancreatitis, changes in its consistency and substance.
With the development of pancreatitis, stool takes on a mushy appearance with a liquid state. Bowel movements occur in small portions. The stool may contain fats, meat fibers and other components of undigested food, which is evidence that there is a deficiency of enzymes that facilitate the absorption and digestion of ingested food products. The presence of undigested fats in stool can cause frequent stools, as well as their transformation into a liquid and foamy state. The urge to defecate may occur up to 3-4 times a day. The stool substance may have the following states:
- a ribbon-like appearance, indicating a pathological change in the sigmoid intestine, the development of a tumor and the appearance of spasms in the sphincter;
- a small spherical appearance resembling sheep feces indicates the development of constipation or ulcerative lesions;
- cylindrical appearance, indicates the normal volume of plant and animal foods in the intestinal cavity;
- shapeless excrement indicates a vegetarian diet; feces contain a large amount of fiber.
The optimal state of the norm of fecal substance should contain the following ratios:
- dense fractions – 20%;
- water – up to 80%;
- The frequency of stool can be up to two times a day, but not less than once in 48 hours.
Normally, during bowel movements there should be a feeling of relief, without unnecessary discomfort and pain. No more than 400 grams should be consumed per day. feces, but when eating plant foods, the amount of stool may increase, and when eating fatty foods, the volume of stool decreases. A light state of feces is considered normal, ensuring a smooth sinking to the bottom in the water.
Healthy human feces
Whatever lifestyle a person leads, in medicine there are standards regarding his waste products:
- ratio of dense particles and water 20/80%;
- stool frequency at least once every two days;
- bowel movements should occur easily, without causing discomfort;
- the average stool volume of a healthy person is 150–400 grams per day;
- the feces should be cylindrical in shape and light, contrary to the popular joke that the feces of a healthy person sink, slowly sinking to the bottom.

A healthy lifestyle is the key to good health. Active people who play sports rarely experience bowel problems
How is pathology diagnosed?
Specific symptoms that may indicate dangerous changes were discussed above.
After examining the patient's stool, the doctor sends him for additional tests. Instrumental research is also carried out.
Primary analysis
The development of the disease and the appearance of possible complications is indicated by the patient’s stool. Therefore, gastroenterologists carefully monitor how it changes. Anyone can do a stool test at home for pancreatitis. Attention should be paid not only to the shade and shape of feces, but also to their smell.
The main symptom of pancreatitis is foul-smelling stool.
The smell is very unpleasant and pungent. This is due to the decomposition and putrefaction of protein residues.
When the color and consistency of feces changes, we may be talking about a relapse. In this case, the person requires urgent medical attention. The most dangerous symptom is the discharge of black feces - in case of relapse, we are almost always talking about hemorrhage. In this case, there is a risk of death.
The most favorable sign is considered to be the release of a cylindrical substance. This indicates that the disease is “dormant” and the food taken has been completely digested.
Carrying out a coprogram
One of the accurate modern research methods is coprogram, which is carried out for all forms of pancreatitis.

Coprogram
It helps determine the degree of functioning of the pancreas and other important organs.
Important! Before taking the test, you need to avoid taking antibiotics.
This is due to the fact that the use of these drugs can distort the picture. If the result is incorrect, then at best the doctor will ask you to take the test again, and at worst, the wrong treatment will be prescribed.
If a person cannot stop taking medications, he should consult a doctor about this.
Before a coprogram you need to undergo mandatory training. It looks like this:
- Freshness is the most important criterion. You need to collect material in the morning, on the day of the study. You cannot activate the release of feces - you should not give an enema, much less take appropriate medications (even herbal ones).
- The biological material collected for research should not contain any impurities. The presence of menstrual flow and urine in the stool is not allowed. If impurities get into the stool, there is no need to bring “everything you have” to the doctor. It is recommended to wait until the next “portion” is released.
- Feces are brought in a special container. A special container is best suited for this. It is sold in all pharmacies. The container is filled with the substance by 30%.
During the study, special attention is paid to both the feces themselves and the “finds” found there - blood, mucus or pus. They are of the greatest value in terms of information content.
The coprogram helps diagnose not only pancreatitis. It detects disturbances in the functioning of the liver, stomach and intestines.
Changes in stool depending on the form of pancreatitis
Stool with pancreatitis directly depends on the stage of the disease and concomitant diseases. The most obvious violations occur during the period of exacerbation, the feces acquire a gray color with a pearlescent tint. This disease is complicated by constipation, indicating an inflammatory process in the digestive tract.
After the transition of acute pancreatitis to chronic pancreatitis, diarrhea overtakes a person. Loose stools can be explained by several reasons:
- in the case of pancreatitis of alcoholic origin, the digestive tract, weakened by toxins, cannot cope with its functions;
- Disturbance of microflora entails the appearance of dysbacteriosis;
- there is an acute shortage of enzymes necessary for complete digestion of food;
- intestinal motility is disrupted.
Causes of stool color change
Painful discomfort under the ribs an hour after eating fatty foods, salty, fried, spicy foods indicates clear signs of illness. The main symptom is accompanied by other symptoms that appear:
- itching;
- increased formation of gases;
- intoxication;
- fermentation in the intestines;
- flatulence.
flatulence
The acute type in patients with pancreatitis is often characterized by the presence of constipation. This indicates the development of pathology observed in the pancreas.
When constipation changes into liquid feces, this indicates the formation of a chronic course of the disease.
Reasons for the development of prolonged diarrhea in chronic pancreatitis.
- As a result of pancreatitis of alcoholic origin, the digestive system is weakened by toxins and is unable to cope with its purpose.
- Changes in intestinal microflora lead to the development of dysbiosis.
- There is an acute deficiency of enzymes that are required for food to be fully digested.
- The intestinal lining is disrupted.
The color of stool during pancreatitis will indicate what is happening to the body.
Features of diarrhea with pancreatitis
Digestive dysfunction is the main symptom of diseases associated with inflammation of the pancreas.

The stool takes on a mushy consistency, and the urge to have a bowel movement appears after every meal.
There are a number of features of stool with pancreatitis:
- During antibacterial therapy, stool becomes yellow and resembles plasticine in consistency.
- With pancreatitis, the color of stool changes to gray or very light, and undigested fats add shine to it;
- Feces have a foul odor and become very viscous (it is difficult to wash off clothes and is difficult to wash off surfaces).
Lack of medical care or untimely initiation of treatment can lead to very unpleasant consequences, the basis of which is dehydration:
- weight loss;
- inflammation of the mucous membranes;
- anemia;
- acute lack of vitamins and minerals;
- insomnia;
- apathy against the background of permanent neurosis.
One of the most alarming symptoms of pancreatitis is black diarrhea. Any doctor, hearing such a complaint, will be seriously concerned about the patient’s condition, since this indirectly indicates internal bleeding. It is blood that can color stool black.
Sometimes black stool is the result of eating foods that contain dye. Activated carbon has the same effect.
Feces for pancreatitis: modifications and interpretation of tests
The pancreas is an important organ of the gastrointestinal tract, playing a significant role in the process of digesting food. Most patients are aware that the pancreas produces insulin, which is necessary for the processing and absorption of sugar. The gland produces the so-called pancreatic juice - reminiscent of gastric juice, necessary for normal and efficient digestion.
With an exacerbation of pancreatitis, with chronic inflammation of the pancreas, the production of pancreatic juice is disrupted, and the outflow is difficult due to edema and inflammation of the ducts. The destruction of the gland begins due to stagnation, at the same time negatively affecting digestion. A sign of inflammation will be stool, changes in which patients note. Stool analysis for pancreatitis clarifies the diagnosis.
Normal stool and its disturbances in pancreatitis
A healthy person's stool consists of approximately 80% water and 20% solids. Color and consistency vary depending on diet. A large amount of plant foods makes the stool abundant, less dense, and shapeless. Consuming a lot of water is semi-liquid, and not enough is dry, like sheep's balls. The color changes depending on the type of food:
- with a mixed diet (vegetable and meat) – dark brown;
- with predominantly meat - very dark;
- with a vegetarian diet or predominantly plant foods – light brown.
Some medications and foods containing intense plant dyes (spinach, blueberries, beets, black currants and others) change the color of stool. Such changes, in the absence of complaints about the functioning of the gastrointestinal tract and pain, are considered normal variants and do not require outside intervention.
When digestive functions are impaired, feces change. A sign of pancreatitis in the absence of pain is a noticeable change in the stool. Calculous (“stone”) pancreatitis, affecting the head of the gland, leads to intractable constipation. When all parts of the gland are affected, on the contrary, bloating and loose stools appear.
Soon after eating, the stomach begins to “boil,” gases form, bloating occurs, and diarrhea occurs. Pancreatic diarrhea begins - foul-smelling, mushy liquid feces with a greasy sheen that is difficult to wash off.
The color of the stool changes: the stool looks light, gray or pearlescent in color, interspersed with undigested food particles, primarily meat.
If at the beginning of the disease constipation occurs more often, and during exacerbations - diarrhea, people with chronic pancreatitis develop changeable stools: constipation is replaced by diarrhea, and vice versa. A noticeable sign of pancreatitis is considered to be an unpleasant, fetid odor of feces associated with rotting proteins in the intestines.
Stool analysis of patients with pancreatitis
When the initial diagnosis of pancreatitis is made, the patient is prescribed to undergo various tests, including a stool test. The goal is to establish the degree of digestion of fats. The presence of these substances in the feces indicates problems with the functioning of the pancreas.
Fecal analysis for pancreatitis speaks primarily about the exocrine functions of the gland - the secretion of pancreatic juice into the gastrointestinal tract. When its amount decreases, feces contain large volumes of undigested fiber, fats, and fatty acids.
Subsequently, stool testing is rarely ordered. Patients are asked to observe their bowel movements and report changes or observations to the doctor. Patients with chronic pancreatitis should pay attention to their stool in order to respond to changes in time and prevent exacerbation.
What is a coprogram
At the onset of the disease, the doctor has the right to prescribe a coprogram - an analysis of the patient's stool for bowel movements. For research, feces excreted from a single bowel movement are collected and placed in a clean glass or plastic container. There is no need to change the diet before analysis, keeping the results unreliable.
First, the general appearance of the patient’s stool is assessed (macroscopic examination): consistency, color, quantity, smell, the presence of visible impurities (blood, mucus, pus), inclusions of foreign particles, undigested food debris or worms. Then a microscopic analysis is carried out, examining the composition of the stool.
Coprogram of patients with pancreatitis
As a result of coprogram with pancreatitis, a change in the amount of feces becomes noticeable. The weight of an adult’s stool at a time is 200 g, in patients with pancreatitis it is often higher.
The consistency also changes - the stool is liquid or mushy. Interspersed with undigested food residues are visible. The presence of an abundance of undigested fats is called steatorrhea, proteins - creatorrhoea.
The number of elements is indicated in the stool analysis or in the transcript of the hospital chart.
Undigested carbohydrates indicate the use of enzymes to digest starch, which is poorly processed by the body during pancreatitis.
Is green really safe?
In the absence of any changes in the diet of a person suffering from inflammation of the pancreas, the stool should always be the same. If the stool suddenly turns green, this clearly indicates the presence of bile in it. In such cases, you should immediately inform your doctor, who will prescribe a therapeutic diet. In addition, the following measures should be taken:
- exclude fatty, fried, smoked, any types of canned food, sweets;
- completely avoid alcohol, coffee and carbonated drinks.

Only a doctor can definitely dispel doubts. In addition to diet, it is necessary to use medications that can only be prescribed by a specialist, based on test results.
How to normalize stool

Every patient who experiences pathological processes in the pancreas must first normalize their diet. To eliminate inflammation in the gland, it is necessary to adhere to a strict diet that excludes all foods that can provoke dyspeptic disorders.
It is worth noting that an exacerbation of the pathology, accompanied by a change in the color of feces, occurs when the diet is violated:
- The patient's diet contains a large amount of food containing starch.
- A person abuses protein foods, in particular meat and eggs.
- The patient consumes fatty foods in unlimited quantities, for example, fish, poultry, butter, and meat.
- The patient's menu includes fried and smoked foods, rich pastries, and baked goods.
To normalize the structure of stool and return it to its usual brown color, patients must adhere to the following rules:
- It is mandatory to undergo a course of drug therapy. Medicines prescribed by a specialist will help eliminate inflammation, as well as normalize the process of enzyme generation. In such situations, patients have to take antibacterial drugs, as well as probiotics.
- After the inflammation is relieved, the patient will have to take medications whose action is aimed at normalizing intestinal secretion and peristalsis, as well as restoring the process of bile generation.
In order to reduce fermentation and putrefactive processes in the intestines, thereby restoring the structure and color of stool, people need to stop eating the following products:
- baked goods;
- fatty, fried and spicy foods;
- jam, jam and bee honey;
- coffee;
- alcoholic beverages;
- confectionery products;
- black tea;
- soda;
- snacks;
- fast food;
- salted fish;
- smoked meats;
- canned food

The diet of a patient who has been diagnosed with pancreatitis should include the following foods:
- low-fat meats, poultry and fish;
- dairy products;
- dried bakery products baked from whole grain flour;
- vegetables;
- cereals;
- fruits;
- homemade jelly;
- unsweetened biscuits.
To restore digestive processes, patients should take probiotics and prebiotics.
The use of enzyme-containing medications, for example, tablets, is also indicated:
To restore pancreatic functionality, patients must take medications with an enveloping effect, for example, Phosphalugel, Almagel. Patients are prescribed calcium supplements and vitamin-mineral complexes. If there are serious changes in the gland, hormone-containing medications are prescribed.
Feces with pancreatitis change characteristics due to a deficiency of pancreatic enzymes, which is visible even to the naked eye. If you notice an uncharacteristic odor or color in your stool, especially if you notice that it doesn’t flush well or sticks to the walls of the toilet, consult a doctor and get examined.

Blood in stool
The most dangerous symptom of pancreatitis, causing anxiety among doctors and fear among patients, is the presence of fresh blood in the stool. There may be several reasons for its appearance:
- tumor processes in the gastrointestinal tract;
- cracks and ruptures of the colon;
- acute inflammatory processes.
At the first detection of blood during a bowel movement, you should immediately consult a doctor, as this may indicate acute pancreatitis.

For diagnosis, the smallest details are very important: the thickness of the clots, their color, the presence of other symptoms
There are symptoms that, in the presence of bloody stool, should prompt you to immediately go to a medical facility:
- painful bowel movements;
- nausea, vomiting, dizziness;
- significant decrease in blood pressure;
- temperature increase.
Diagnosis of pancreatitis
One of the very first and most reliable tests prescribed for the diagnosis of pancreatitis is a coprogram.

At the initial stages, in laboratory conditions, they find out whether there are traces of undigested food in the stool, the presence of which indicates a lack of enzymes
There are rules for collecting material for analysis, because only if the necessary techniques are followed will the result be reliable. Basic recommendations:
- before collection, try to avoid taking medications as much as possible;
- follow a therapeutic diet;
- collect feces in a sterile container;
- the material must be fresh (overnight storage in the refrigerator is possible);
- women undergoing analysis during menstruation must use a tampon, having previously carried out hygienic procedures.
How to get tested
To obtain reliable data, 4 days before the test you need to switch to a special diet consisting of mashed potatoes, a small amount of other pureed vegetables, cereals, dairy products and fruits. You should not eat heavy foods (meat, fish, eggs), or those containing large amounts of plant fiber - tomatoes, beets and all types of green vegetables.
The daily amount of calories, which must be divided into 5 doses, should not exceed 2250. During this period, you cannot take enzyme preparations. If a colonoscopy or examination of the digestive system using barium was performed, stool sampling can be done after 2 days.
The day before stool collection, you should not do the following:
- enema;
- take laxatives and medications containing bismuth;
- introduce suppositories.
Women should not have stool tested during menstruation.
Before collection, it is necessary to wash the genitals and anus, urinate - there should be no urine in the stool. It is better to defecate in a special vessel and immediately take a sample from it for analysis - approximately 30 g of feces. The material is collected in a dry and clean container, filling it 30%, closed and submitted to the laboratory as quickly as possible, since after cooling the characteristics of the feces begin to change.
Stool analysis can be done in any clinic where there is a laboratory. The results will be ready on the same day.
Coprogram
Feces are the final product of food processing, which undergoes mechanical, chemical and enzymatic processing in the body.

In case of diseases of the digestive organs, one can judge the problem and its location based on the results of the coprogram. This is a stool analysis, including the following studies:
- general - quantity, smell, color, consistency, impurities;
- microscopic - the presence of biological fibers, tissues, salt crystals.
Treatment of pancreatic diarrhea
Diarrhea, no matter what disease it is caused by, requires an immediate response, because it instantly leads to dehydration of the body and causes serious complications. For pancreatitis, a comprehensive approach is taken to solving this problem:
- prescribe medications;
- recommend strict adherence to a therapeutic diet;
- The use of traditional methods is allowed (with prior consultation with a specialist).
Medications
The treatment strategy for diarrhea always depends on the form of pancreatitis and the presence of concomitant diseases. Traditionally there are 2 ways:
- Oral. It consists of prescribing enzyme-containing drugs that facilitate the functioning of the pancreas (Creon, Pancreatin, Bifidumbacterin, etc.).
- Intravenous. Used in acute periods when immediate response is required. It is carried out in a hospital. Solutions of electrolyte salts are prescribed (Disol, Trisol, etc.)

When taking any medications, you should always strictly follow the instructions and prescription of the doctor.
Folk remedies
If the situation is not critical, and the doctor has approved the proposed method of treatment, you can try folk remedies. Traditionally, they consist of consuming decoctions of medicinal herbs.
A decoction of corn silks and other medicinal plants:
- take equal parts of corn silk, chamomile and calendula inflorescences;
- pour boiling water at the rate of 1 tbsp. herbal mixture per 1 glass of water;
- leave for 1 hour;
- consume half an hour before meals.
- take mint, elecampane and string in equal parts;
- pour boiling water at the rate of 3 tbsp. spoons of prepared herbal mixture per 0.5 liters of water;
- Seal tightly and leave for at least 1 hour.
Abnormal bowel movements during pancreatitis are common, but it is important to respond to it in time and consult a specialist. With timely treatment, you can get rid of this unpleasant symptom. In diseases associated with digestive dysfunction, one of the most important conditions for positive dynamics is the patient’s attentive attitude to changes in his body.
Today, a person of any age is diagnosed with pancreatitis. A factor in this is poor nutrition and an unhealthy lifestyle. To reliably diagnose pancreatitis, the patient needs to undergo a series of examinations. Particular attention is paid to the study of excrement. Feces with pancreatitis have a mushy type. When the patient has a bowel movement, stool due to pancreatitis does not come out completely. In the structure of feces, fatty acids, muscle fibers, connective tissue, and starchy grains are observed, this indicates a lack of enzymes that produce normal digestion. Undigested fats in stool during pancreatitis lead to frequent visits to the bathroom. Often the consistency of stool is liquid or foamy. The number of trips to the bathroom per day is 4 times.
What diseases cause discolored stool?
Our readers successfully use Monastic Tea to treat gastritis and ulcers. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The pigment that gives stool its color is mainly bilirubin. Together with bile acids, it breaks down proteins that contain hemoglobin and other hemes.
Bilirubin is brown, so it colors feces. There is no pure bilirubin in feces, since in the intestines it turns into another brown pigment - stercobilin.
If little bile enters the intestines, the stool is not colored. Food remains are excreted undigested and uncolored, that is, the feces become acholic.
Young children (up to two months of age) fed only formula or breast milk may produce light yellow or whitish stool due to insufficient enzyme production.
This should not alarm parents, since discolored feces at this age are considered a physiological norm.
Acholic stools are not always associated with a lack of bilirubin. Diet can affect the color of stool.
Discolored feces appear after consuming homemade sour cream, butter, and animal fats.
Due to their high fat content, such products cannot be completely digested and enter the large intestine unchanged, partially discoloring the feces.
This phenomenon is not dangerous to health. After a few days, the color of the discolored feces will be restored. The person does not experience any unpleasant symptoms and feels completely healthy.
To determine what exactly made the feces discolored in an adult - diseases of the gastrointestinal tract or dietary features, you need to monitor whether there is a connection between the color of feces and nutrition and how often discolored feces appear.
Isolated cases of discolored stool in an adult are more likely to indicate an excess of fatty foods, chocolate or alcohol in the diet than to health problems.
In order for stool to stop being discolored, it is enough to adjust your eating habits. It is useful to exclude alcohol and dishes prepared by frying from the menu - this will facilitate the work of the liver and pancreas, and the production of bile will be restored.
Some medications can cause discolored stool.
These include:
- non-steroidal anti-inflammatory drugs;
- oral contraceptives;
- aspirin;
- antifungal tablets;
- drugs to get rid of tuberculosis.
The listed groups of medications do not directly discolor stool - they affect the functioning of the liver.
If, during treatment with the above drugs, discolored feces appear, then you must inform your doctor about this. You may need to immediately check the condition of your liver and adjust your treatment.
Diseases of the digestive organs
A common cause of discolored stool is inflammation of the pancreas (pancreatitis).
Feces with pancreatitis are liquid, mushy, they contain a large amount of unprocessed fats, since the body does not have enough enzymes to process them.
The color of stool can be described as pearlescent or dirty gray. Simultaneously with the change in the color of the stool, the temperature rises, pain in the hypochondrium, dizziness, and vomiting begin.
The pain may be tingling in nature. Taking painkillers does not improve the condition.
Acute pancreatitis is a serious illness with the possibility of death. The chronic form is less severe.
Feces in chronic pancreatitis have a characteristic odor and gray color and are difficult to flush down the toilet. A dull pain appears in the hypochondrium, and the temperature may rise.
Another reason why stool may become discolored is cholecystitis. This is the name for inflammation of the gallbladder, an organ in which bile produced in the liver accumulates before being released into the intestines.
With cholecystitis, a large amount of fat and nitrogenous products are found in the stool, leading to a change in its color to light, sometimes whitish.
Symptoms of gallbladder inflammation:
- stool discoloration;
- pain in the right hypochondrium that occurs after eating spicy or fatty foods or drinking alcohol;
- constant nausea;
- bitter or metallic taste in the mouth;
- irritability, insomnia;
- white coating on the tongue, dry mouth.
Cholecystitis can occur in acute and chronic forms - the color of stool changes in both cases. In case of acute cholecystitis, the patient needs urgent surgery. The chronic form is treated conservatively: with medications and diet.
Discoloration of stool due to cholelithiasis
Another common gallbladder disease, cholelithiasis, can lead to the appearance of discolored stool.
With this disease, undigested fat is found in the coprogram, which gives the feces a light yellow color.
Light-colored stool means that due to a blockage in the bile duct, bile does not flow into the intestines in sufficient quantities.
A typical symptom of gallstone disease is biliary colic. The patient (usually in the evening or at night) has a slight rise in temperature, the skin and mucous membranes turn yellow, and diarrhea and vomiting begin.
After an injection of an antispasmodic, the spasm ends and the state of health improves. With a mild form of cholelithiasis, attacks of biliary colic are observed 1–5 times a year, with a moderate form - once a month. In severe cases, the stomach hurts constantly, the stool is liquid and discolored.

To diagnose cholelithiasis, it is necessary to do a stool and blood test, perform an ultrasound examination or tomography of the liver and gall bladder. GSD is a disease in which it is very important to be able to prevent colic.
To prevent attacks, a special diet and medications are used to dissolve cholesterol stones.
It is very important for people with gallstones to monitor the color of their stool. If you notice discoloration of feces (usually this phenomenon is accompanied by soreness under the ribs on the right side), you should immediately go on a strict diet. Nutritionists recommend using diet No. 5 to prevent exacerbations of cholelithiasis.
Inflammatory liver diseases
Has your stool become discolored and your urine dark? Most likely, these are symptoms of hepatitis - a dangerous viral disease.
Depending on the type of virus, hepatitis A, B and C are distinguished. In recent years, other types of the virus have been identified.
Lightening of stool is observed with any type of viral hepatitis. Hepatitis A can be contracted through water and food. Hepatitis B is transmitted only through blood.
Its most dangerous complication is cirrhosis of the liver, which develops in 10% of patients. Hepatitis C proceeds in the same way as the previous form, but is much easier to tolerate.
How do stools change?
Stool with pancreatitis directly depends on the stage of development of pancreatitis, as well as adjacent pathologies. During an exacerbation of the pathology, the patient’s stool is dirty gray, pearlescent in color. Brown gamma stool indicates changes in diet, yellow substance is observed in childhood when children are breastfed.
However, during the course of treatment, yellow stool is also observed due to the use of antibacterial drugs. The feces themselves are similar in structure to soft plasticine. Such changes will cause the development of other pathologies.
When digestion is disrupted, stool becomes diluted. Due to intense interstitialization, feces acquire a mushy consistency, and fermentation leads to a foamy texture of feces.
Pancreatitis is considered a disease that affects the color and texture of stool.
The feces may become lighter in color, which is a warning sign that bile is accumulating in the gland. The feces become viscous, are not completely washed off and have an unpleasant odor.
When acute pancreatitis becomes chronic, a person develops loose stool.
Character of stool in chronic pancreatitis.
- Ribbon-shaped appearance - indicates a painful phenomenon in the sigmoid colon. This feature of feces indicates the appearance of a tumor formation or the presence of sphincter spasms.
- The shape of sheep stools resembles dark colored balls. Such stool is observed when a chronic form of constipation or ulcerative pathologies develops.
- The shape of the sausage shows that the person has consumed foods of plant and animal origin in normal quantities.
- Shapeless feces - appears in people who eat a vegetarian diet, which indicates the consumption of foods containing a large amount of plant fiber.
Type and features
To determine the type of substance, the Bristol scale is used. The main types are presented in the table.
| View | Description |
| Liquid | There are no solid particles at all. |
| Lumps | They are quite hard. Characterized by difficult passage. Shape: walnut. |
| "Flakes" | The specific difference is looseness. The ends are uneven. Another difference is the mushy quality. |
| "Sausages" | The surface is smooth, the consistency is quite soft. Small cracks may appear on the surface. |
| Lumps | They are distinguished by their softness. The ends are straight. Feces come out easily. |
Shape of feces
Feces may be:
- ribbon-shaped;
- formless;
- "sheep";
- cylindrical.
What does the presence of mucus indicate?
If mucus is contained in small quantities, this is not considered a pathology. Mucus is a necessary substance for transporting feces. When pancreatitis develops, the amount of mucus increases.
Important! An alarming signal is the presence of a large amount of mucus on the walls of the toilet.
This suggests that pancreatitis has strengthened its position and may be preparing to transform into a chronic form.
Sometimes excess mucus is due to the fact that in this way the body is trying to expel dangerous substances along with loose stools. He also tries to get rid of food processing residues.
What does the presence of blood indicate?
The appearance of blood in the stool is accompanied by the following symptoms:
- increased number of urges to urinate;
- weakness (combined with dizziness, headaches. Often a person feels tired even after a long rest. He always wants to lie down);
- nausea (sometimes turns into vomiting, which does not bring relief - the person still feels sick. The patient may vomit several times a day);
- pain during bowel movements (a person complains of abdominal pain. It can be either mild or quite sharp);
- a sharp drop in blood pressure.
Bloody impurities in the stool can signal the development of a dangerous complication - oncology.

Blood in stool
But in 70% of cases, not everything is so bad. Blood in feces is formed due to the presence of cracks in the walls of the colon.
If acute pancreatitis has already been diagnosed, this symptom may signal its exacerbation.
Color of feces with pancreatitis
Pancreatitis is a disease that leads to a change in the natural functioning of digestion. A lack of enzymes contributes to a negative effect on all organs, and the color of the excrement will allow you to determine the real violations.
After eating foods prohibited for consumption, the patient experiences indigestion, which is accompanied by a condition where a process of decay and fermentation develops. Fatty meats, fish, lard and other products lead to negative consequences, changing the color of stool in the pathology of pancreatitis.
Green stool with pancreatitis indicates an exacerbation of changes in exocrine function. This situation is characteristic of the chronic type. In addition, green stool will occur when stagnation of bile develops and the release of the substance into the stomach increases.
As a result of the abuse of fatty foods and alcohol, a painful phenomenon develops in the pancreas, and the stool becomes light-colored.
If, in addition, signs of painful discomfort and stool disorder are formed, then light-colored feces clearly indicate pancreatitis. Light color appears when taking medications or due to infectious manifestations.
If a patient has pancreatitis, doctors advise carefully monitoring the color of feces. A dangerous sign of pancreatic disease is black feces. It signals the formation of serious diseases. This often indicates the presence of internal bleeding. It happens that the cause of blackness is in taking certain medications - activated carbon. Dangerous impurities are observed in the stool, which is a reason to consult a doctor.
It is normal for there to be a small amount of mucus as it is necessary for the stool to move easily. When pancreatitis forms, the volume of mucus can increase. When obvious marks remain on the toilet, this is a reason to think about it.
Mucus in feces occurs when enzymes are too active. When a painful phenomenon occurs, the gastrointestinal tract attempts to stop it thanks to mucus, as a result of which it is excreted from the intestines along with excrement. This cleanses the body of toxins and prevents the organ from becoming inflamed. A large volume of mucus also indicates other diseases, which are taken into account.
The presence of blood in feces during pancreatitis is considered the most negative cause, which is characterized by the following situations:
- the presence of formations in the digestive tract;
- wounds and ruptures in the walls of the large intestine appear;
- the presence of inflammatory phenomena that have progressed to the acute stage;
- There are areas that bleed.
Due to the severity of the symptom, doctors, using laboratory stool analysis and blood tests during the development of pancreatitis, identify the true factor in the appearance of bloody bowel movements for subsequent therapy.
If a patient develops the following symptoms, doctors advise immediately going to the hospital.
- Symptoms of itching and burning, blood in excrement.
- Nausea.
- Weakness.
- Painful sensations during bowel movements.
- Rapid drop in pressure.
- Feces come out in large volumes.
- Temperature increases.
Until the cause of blood in the stool is determined, you should not eat foods that are difficult to digest. It is forbidden to include fatty, spicy, smoked foods in the diet for pancreatitis.
Stool color
Pancreatitis refers to diseases that inhibit the functioning of the digestive system. An insufficient amount of enzymes necessary for digestion negatively affects the functioning of all organs of the gastrointestinal tract, and some problems can be immediately identified by the color of the patient’s stool. In fact, by characterizing the patient’s condition, the color scheme of stool will help to accurately determine the condition of individual sections of the intestine, as well as find out the cause of malfunctions of the gastrointestinal tract.
During the development of the disease, experts advise paying attention to such points as:
- The stool changes in consistency. It becomes liquid, there are lumps in which fragments of undigested food can be seen.
- Change in stool color. Gray-green confirms doubts about the development of pancreatitis.
- A strong stench is nothing more than the presence of rotting processes in the intestines.
Green stool for pancreatitis
Failures in the synthesis of enzymes involved in the digestion process affect the consistency of stool and its color. Banal indigestion can be caused by improperly selected food products, which subsequently causes a reaction of rotting and fermentation. The same reason applies to the color of stool, for example, fatty meat, fish, lard and other products after consumption can become precisely the factor that modifies the consistency and color shade of stool. The main reason for the appearance of green stool in pancreatitis is an exacerbation of the situation with exocrine function, which usually develops in the chronic form of the disease. A concomitant factor that provokes the phenomenon may be stagnation of bile, or an increased release of a substance into the stomach.
For this type of manifestation, a special diet is prescribed:
- All sweets are excluded from the menu, including sweets, cakes and other similar products.
- Complete refusal of fatty foods (meat, lard, fish).
- Forget about carbonated and alcoholic drinks, chocolate and coffee.
- Fast food in the form of fast foods, sandwiches and similar foods should be completely excluded from the diet.
Since the problem needs to be changed for the better, in addition to a strict diet, experts advise restoring and normalizing the color of stool using medications in the following sequence:
- Localization of inflammatory processes.
- Restoring the normal functioning of intestinal secretions.
- Normalization of peristalsis.
- Improving the condition of the biliary tract.
Light feces
Light-colored stools most often indicate that there is a malfunction in the digestive system due to inflammation of the pancreas, which is provoked by fatty foods or the consequences caused by prolonged consumption of alcoholic beverages. The color itself may indicate the development of other diseases, but in combination with the main symptoms, stomach pain, diarrhea, in most cases the development of pancreatitis is expected. In order to accurately diagnose, experts advise carrying out a number of measures to help find out the cause of the manifestation.
With pancreatitis, light-colored stool may appear at the time of taking medications, or due to the development of infectious processes in the gastrointestinal tract. The listed reasons are the main ones, but to accurately characterize the manifestation, experts advise conducting additional research in the form of submitting stool for laboratory analysis.
Black chair
First of all, the patient himself should pay attention to changes in the color of stool; this will help to avoid or prevent a lot of negatively affecting consequences that are “rich” in diseases from the complex category. The appearance of black diarrhea is a dangerous harbinger, which can combine many suspicions regarding the patient’s condition. Most often, such feces indicate the presence of internal hemorrhages.
Also, the cause of black stool may occur due to the use of medication, such as activated carbon, but this factor is usually taken into account by the patient himself.