Erythematous reflux esophagitis is an inflammatory process of the esophageal mucosa caused by prolonged or persistent negative effects of gastric contents on the mucosa.
Unlike the gastric mucosa, the esophagus is not protected from the aggressive effects of hydrochloric acid contained in gastric juice. With regular reflux of gastric juice into the esophagus, pathological changes occur in the cells of the organ mucosa and deeper tissue structures.
If the reflux of hydrochloric acid into the esophagus is short-lived, only inflammation and swelling are observed. With prolonged exposure, erosive foci are formed on the surface layer of the organ mucosa, occupying a large area and subsequently merging with each other, which is what the name of the pathology is associated with.
This disease is characterized by frequent bleeding and hemorrhage, and there is a risk of hemorrhagic effusion.
The disease is treated by adjusting the diet. Therapeutic therapy includes drug treatment; alternative medicine methods are considered effective for this pathology.
What is reflux - esophagitis?
The esophagus is located behind the trachea. The organ consists of several layers: the mucous membrane, the muscular layer and the outer membrane. The main function of the esophagus is to promote the bolus of food to the digestive organ. The evacuation function of the organ is carried out with the help of longitudinal folds, which are actively involved in the process of movement.
The esophagus has glands that produce mucous fluid. The fluid also participates in the process of movement, while simultaneously protecting the surface of the esophagus from damage.
The muscle layer that forms the upper and lower sphincters helps accelerate the movement of the food bolus along the length of the organ. The inferior pylorus is located between the stomach and esophagus, and is closed during meals. When you swallow food, the sphincter opens, allowing food into the stomach. When the sphincter is disrupted, a reflexive disease occurs.
When food enters the stomach, the process of processing it begins under the influence of hydrochloric acid, which is contained in gastric juice. Digestion is also facilitated by the peristalsis of the digestive organ, which helps the manifestation of 20 - 30 physiological refluxes that do not cause discomfort to a person. Reflux is a normal part of the digestive process. The pathological condition occurs when the protective mechanisms of the esophagus are disrupted.
The main protective barrier of the esophagus is the mucous membrane of the organ. It is this that protects the organ from mechanical injuries when moving a bolus of food, especially if the food is not chewed well, and from the effects of hydrochloric acid that enters the esophagus during physiological reflux.
The protective mechanisms also include the lower valve of the esophagus, which prevents frequent entry of gastric contents into the esophagus. Violation of the protective mechanisms of the esophagus can also be caused by a failure of the blood supply, which leads to the appearance of wounds and erosive formations on the surface of the mucosa and inhibits the wound healing process.
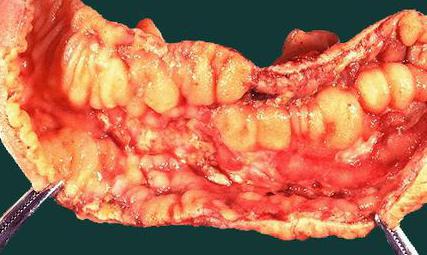
Erosive reflux esophagitis is a complicated course of the disease, detected by the reflux of stomach contents back into the esophagus. The disease in most cases is localized in the distal zone (lower esophagus). Specific to this pathology is the appearance of ulcers and erosions on the mucous membrane, which in the later stages merge into a single erythema.
Symptoms of the disease
Almost always, concomitant diseases with hyperemia are gastritis, stomach ulcers, and duodenitis. Less commonly, diseases that are not related to the gastrointestinal system are associated with hyperemia (overflow of blood in the vessels of the circulatory system of any organ or area of the body).

Thus, the following symptoms are characteristic of different forms of gastritis:
- Symptoms of hyperemia (overflow of blood in the vessels of the circulatory system of any organ or area of the body) (overflow of blood in the vessels of the circulatory system of any organ or area of the body) of the gastric mucosa. The gastric mucosa is focally hyperemic, there is a coating with whitish foamy mucus on the surfaces of the organ in “mucus lakes”, the folds are compacted and are not completely smoothed out with the help of air.
- As cells die, the surface becomes thinner and turns pale. In this case, the foci of the disease do not become hyperemic, and the vascular web is clearly visible.
- In the superficial form of gastritis, the mucous surface of the stomach (a hollow muscular organ, part of the digestive tract, lies between the esophagus and the duodenum) is hyperemic throughout or only in the body and antrum of the stomach. Sometimes hyperemia is focal in nature or can be diffuse.
- If there is fibrous gastritis, hyperemia is most pronounced, while it is focal and characterized by the presence of pus. This inflammation can be caused by measles or scarlet fever infection. The patient may vomit blood frequently.
- The phlegmonous form of the disease can be triggered by trauma to the stomach with sharp objects, such as fish bones. In such cases, this indicates possible hyperemic foci.
- Bulbit is characterized by swelling and redness, thickening of folds in the antrum. Among the reasons are Helicobacter pylori infection of the antrum of the stomach (a hollow muscular organ, part of the digestive tract, lying between the esophagus and the duodenum) and unhealthy diet.
- Renal dysfunction (various degrees of swelling).
- Depression and permanent stress also provoke hyperemia.
The main symptoms of gastropathy include:
- hyperemia of the mucous membrane;
- pain in the stomach;
- nausea, vomiting;
- heaviness, weakness;
- loss of appetite.
If such symptoms appear, patients should undergo an examination and consult a doctor - an endoscopist, who will prescribe antigastritis therapy based on the diagnostic results. If necessary, with severe manifestations of pathology in the stomach, endoscopic resection will be prescribed. The prognosis after the operation is quite favorable.
Types of disease
The classification of erosive reflux-esophagitis is carried out depending on the phase and nature of the course.
- Sharp look. This type is quite common and is detected by superficial or deep lesions of the mucous membrane. The disease occurs suddenly, the clinical picture is pronounced. With timely treatment, when the treatment tactics are chosen correctly, recovery occurs quickly and complications do not arise.
- Chronic appearance. Fixed in most cases, characterized by periods of exacerbation and remission. The chronic type of pathology occurs as a result of prolonged exposure to negative factors and therefore at this stage there is a risk of the formation of irreversible complications. The treatment course for erosive esophagitis is about 6 months.
- Ulcerative appearance. Erosive formations in this form affect the deeper layers of the mucous membrane of the esophagus. The ulcerative form requires long-term therapy.
- Peptic appearance. When the contents of the digestive organ penetrate the esophagus, swelling and inflammation of the mucous membrane of the organ develop, this is a prerequisite for this type of pathology.
- Catarrhal appearance. Damage to only the upper layers of the mucosa is observed. Characterized by redness and hyperemia of the mucous membrane.
The pathological process can affect different parts of the organ and, depending on the localization zone, the following are distinguished:
- Total. The entire esophagus is affected;
- Proximal. The upper parts of the esophagus are affected;
- Distal. The pathological process is localized in the lower part of the esophagus, as well as near its junction with the stomach. This type of lesion occurs in patients more often than others.
Erosive reflux esophagitis occurs in several phases:
- First phase. Single erosive formations appear on the mucosa, the size of which does not exceed 5 mm;
- Second phase. It is possible for erosive formations to merge with each other, which are located on the surface layer of the mucosa and do not penetrate into its deeper layers;
- Third phase. Characteristic of this stage is the spread of the inflammatory process to the entire mucous membrane. Small erosive foci merge to form ulcers;
- Fourth phase. The presence of chronic ulcers of the distal zone of the esophagus and narrowing of its lumen are observed.

More about the disease
The term “hyperemic gastropathy” can be found in the endoscopic report of the patient; it indicates that during the examination there is redness, bruising and swelling of the gastric mucosa. The result of this process is increased vulnerability of the gastric membranes, increased mucus secretion and hyperemia. In medicine, almost all diseases related to the gastrointestinal tract fit into the general name “gastropathy”.
We can say that this is the same superficial chronic gastritis, characterized by both minor and extensive inflammation of the gastrointestinal tract. Hyperemic gastropathy is not a disease, per se, but a complication accompanying gastritis, with typical symptoms.

Causes
The main reason for the development of reflux disease is impaired functionality of the lower esophageal sphincter as a result of a decrease in its muscle tone. When the inferior pylorus remains open or semi-open at all times, stomach contents can leak into the esophagus. The cause of this disorder may be regular stress conditions, chemical or nutritional factors, or increased pressure in the abdominal cavity.
The main causes of the pathology include a hiatal hernia, through which, with increased intra-abdominal pressure (for example, when there is excessive physical activity), part of the stomach and its contents penetrate into the chest cavity.
The occurrence of the disease is also due to:
- Forced body position with a forward bend;
- Obesity;
- Smoking, alcohol abuse;
- Frequent consumption of spices, coffee, chocolate;
- Pregnancy;
- Taking certain medications, such as nitroglycerin, theophylline, hindine, antibiotics, antidepressants, metoprolol;
- Peptic ulcer of the stomach and 12 intestinal rings;
- Violation of diet (overeating at night);
- Frequent constipation;
- Scleroderma;
- An anomaly in the formation of the neuromuscular system in children.
Diagnosis of the disease
This disease occurs unnoticed and there are no specific symptoms. It is difficult to recognize the disease, so laboratory examinations and tests are prescribed, on the basis of which a diagnosis is made. List of necessary examinations that the patient must undergo:
- General blood analysis.
- Detailed blood test.
- Biochemical tests.

- Bacteriological studies of stomach contents.
- Fibrogastroscopy.
- Biopsy.
- X-ray.

- Sonography of the abdominal organs.
- MRI or CT.

Symptoms of reflux - esophagitis
Reflux - esophagitis is detected by painful sensations behind the sternum. The pain may radiate closer to the heart and to the left shoulder; in some cases, a feeling of sucking in the pit of the stomach may appear. The patient often complains of heartburn, a burning sensation in the upper zone of the esophagus. Heartburn appears after eating, especially after drinking coffee, alcohol, spices, fatty foods, and hot dishes.
The pathological condition may also be accompanied by:
- Belching of air or sour contents;
- Difficulty swallowing and passing food (dysphagia). This symptom is observed with severe inflammation of the esophageal mucosa. The cause of the symptom may also be extraesophageal manifestations;
- Bronchoobstruction, when blockage of the bronchi by a secret mass is detected. The condition manifests itself as a cough and has a chronic course. The cough starts to bother me at night. Bronchoobstruction occurs as a result of the entry of small particles from the esophagus into the bronchi. Reflux esophagitis is considered to be a triggering mechanism of bronchial asthma;
- Chest pain reminiscent of an angina attack. Unlike angina, pain with reflux-esophagitis appears after overeating, eating sour, spicy foods;
- Pharyngitis, rhinitis. Inflammation of the nasal or pharyngeal mucosa develops as a result of frequent contact with the acidic contents of the stomach;
- Dental pathologies. Dental problems occur due to the reflux of acid from the esophagus into the oral cavity. Acid has a destructive effect on tooth enamel and can provoke the development of caries.
The patient often experiences a slight increase in temperature, hoarseness, a feeling of a lump or prolonged discomfort in the throat, damage to the vocal cords, laryngeal papillamatosis, neck pain, pain in the lower jaw, arrhythmia, bad breath, weakness and dizziness.
Erythematous gastropathy with focal atrophy of the gastric mucosa
Erythematous gastropathy refers to redness of the gastric mucosa, which may be accompanied by swelling, bleeding and excessive mucus production. A similar sign is determined when examining the stomach using an endoscope - fibroesophagogastroduodenoscopy.
Hyperemia of the mucous layers of the stomach is provoked by some unfavorable factors, for example, spicy, rough and too hot foods. Under the influence of the causative factor, microcirculation is activated in the affected areas of the stomach, which gives it a bright red color.
Not everyone knows what atrophy of the gastric mucosa is.

Degrees
Endoscopy allows you to visualize the inflammatory process:
- In the first degree (a), confluent erosive formations and/or erythema of the distal zone of the esophagus can be seen.
- The second degree (c) is characterized by fused erosion membranes, which occupy a small part of the organ mucosa.
- The picture in the third degree (c) is as follows: erosive lesions occupy the lower third of the esophagus. The entire surface of the mucosa may be covered by confluent erosive formations.
- In the fourth degree (d), the formation of a chronic ulcer of the esophagus is recorded, as well as gastric or intestinal metaplasia of the mucous membrane. Experts characterize the picture as Barrett's esophagus.
Characteristics of the disease, including causes, symptoms and methods of detection
Etiology and pathogenesis
The pathogenesis is due to the depth and extent of changes in the structure of the gastric membranes and impaired functionality of the digestive glands. Diseases are based on the degeneration of one type of tissue into another. In adults, the development of the disease occurs gradually, and in children it develops quickly and is caused by helminthic infestations, the transition from breastfeeding to artificial feeding, and replacement of the nutritional formula. The development of gastropathy can be triggered by the following internal and external factors:
Very important! Savina G.: “I can recommend only one remedy for the quick treatment of ulcers and gastritis” read more.
- burns;
- injuries;
- taking NSAIDs;
- reflux of bile from the duodenum;
- errors and irregularities in nutrition;
- alcohol;
- smoking;
- stress.
Return to contents
Classification of gastropathy
It is based on morphological changes in stomach tissue, which go through 4 stages:
- The first degree is hyperemic gastropathy. Occurs under short-term influence of an aggressive factor, characterized by minor inflammation, without violating the integrity of the mucous membrane.
- The second stage is chronic. In this case, ulcers, erosions, and impaired secretion of the gastric glands are formed.
- Third subatrophic stage. An atrophic type of change appears, in some places it will be replaced by connective tissue.
- Hypertrophic gastropathy is characteristic of the fourth stage. The walls of the stomach become thickened, inelastic, and cysts and adenomas are visible on the mucous membrane.
Diagnostics
The severity of the clinical picture of reflux esophagitis does not correspond to the severity of the disease, and therefore an instrumental study is necessary for an accurate diagnosis. After examining the patient, the doctor prescribes:
- Fibroesophagogastroduodenoscopy (fegds). The study is carried out using a probe with a camera. The device is inserted through the mouth, the camera is moved to the problem area of the digestive tract. The method allows you to examine the esophagus and partially the stomach. With reflux esophagitis, the mucous membrane is hyperemic, and it is possible to detect the reflux of contents into the esophagus. The study allows you to accurately determine the presence of pathology; with the help of this examination, a biopsy is taken if necessary.
- Esophagomanometry. The study evaluates the peristalsis of the lower esophageal sphincter. The procedure is carried out using special catheters, which are inserted through the mouth or nose and with their help the pressure inside the lumen of the esophagus is measured. In the absence of pathology, the pressure in the lower esophageal sphincter is 6–25 mm Hg. Art. The pathological condition is characterized by a decrease in pressure as a result of relaxation of the sphincter.
- Daily ph-metry. Allows you to determine daily variations in acidity in the esophagus. The standard acidity value is no more than 4 (the environment is more alkaline), with frequent injections of hydrochloric acid into the esophagus, the pH decreases and the environment becomes more acidic. The frequency of reflux can be assessed by pH fluctuations. Frequent reflux indicates a severe course of the disease.
- Acid perfusion test or Bernstein test. An examination using a special probe can detect reflux esophagitis at the initial stage in children.
- X-ray using a contrast agent. The procedure helps to identify ulcers, narrowings, and changes in the esophageal mucosa as a result of the inflammatory process. And also evaluate its passability.
- Chest X-ray. It is carried out to exclude pulmonary diseases and bronchitis.
- ECG. It is carried out to exclude angina pectoris.
- Breathing tests. Helps determine the presence of Helibacter pylori bacteria.
- Manometry. Gives the opportunity to evaluate the contractile activity and synchrony of esophageal peristalsis.
- Ultrasound, MRI, CT. These studies are being conducted to detect changes in the esophagus and concomitant diseases of the gastrointestinal tract.
Diagnosis of pathology
To detect the disease - even if there are almost no problems with the stomach - make an appointment with a gastroenterologist.
A comprehensive diagnosis is required, since there is no specific clinical picture. A gastroenterologist, after a visual examination and history taking, may prescribe the following:
- general clinical and biochemical blood test;
- general urine analysis;
- general analysis of stool;
- pH-metry;
- PCR testing;
- endoscopic examination of the gastrointestinal tract;
- esophagogastroduodenoscopy;
- X-ray of the stomach with a contrast agent;
- ELISA.
At the discretion of the doctor, the diagnostic program can be supplemented with other laboratory or instrumental research methods.
Treatment of reflux esophagitis
Treatment of reflux esophagitis is aimed at eliminating the cause of the disease. Properly organized therapy can make the symptoms of the disease less pronounced, help reduce the negative effect of gastric juice on the esophageal mucosa, and increase the resistance of the mucosa.
Complex therapy for reflux esophagitis includes:
- Use of medications;
- Following a special diet;
- Use of folk remedies;
- Surgery if necessary.
Treatment of the patient also includes adjusting the daily routine. It is necessary to exclude nervous overload. You need to maintain a sleep schedule. It is recommended to sleep on a small pillow so that your head is 30 degrees higher than your body, which will help reduce the number of refluxes at night.
Tension of the abdominal muscles should be avoided, and medications that reduce the tone of the lower esophageal sphincter (nitrates, amino acid, sedatives and hypnotics) should be avoided. It is necessary to avoid tight clothing, which can cause an increase in intra-abdominal pressure.
You need to eat about 6 small meals a day. The last meal should be 2 – 4 hours before bedtime. Walking after eating is useful, since in this way the food taken is quickly absorbed and moves more quickly from the stomach to the intestines.
Treatment
The onset of erythematous gastropathy of various forms can cause serious damage to the gastrointestinal tract, leading to a chronic form. Potential complications include: gastritis, gastroduodenitis, peptic ulcer, cholecystitis. Relying only on self-medication is dangerous. The slightest signs of stomach problems require consultation with a specialist. He will tell you how to properly treat gastroduodenopathy.

Getting rid of the disease depends on the form, type, and cause of the lesion. Methods for treating inflammation of the gastric mucosa are:
- restorative nutrition - diet 5;
- folk remedies;
- taking medications.
Diet
Spicy, fatty, smoked, fried foods are excluded from the diet. Prohibition of alcoholic beverages and tobacco products. The diet involves split meals in small portions. The intervals between meals are two to three hours. If the cause of the lesions is a malnutrition, following this diet will quickly relieve the signs of gastropathy. Symptoms and treatment are easily determined in the absence of other pathogens.
It is important to know! The focal form, usually caused by poor diet, resolves within a week.
Medicines
The nature of the course of inflammatory lesions determines effective medications. Each case requires a specific approach:
- increased acidity - medications are prescribed that lower its level, coat the walls of the stomach, antacids;
- the presence of pathogenic microorganisms requires the inclusion of antibiotics;
- low acidity requires drugs that regulate the action of motility of the gastrointestinal tract;
- Acute, advanced cases are accompanied by pain syndromes, and drugs that block them are prescribed.
Folk remedies
Diet and medication are the most common way to combat erythematous gastropathy. Treatment with folk remedies is preventive in nature and is used as part of complex therapy. However, natural components cope well with mild inflammatory processes.
Decoctions and tinctures based on herbs have become widespread: chamomile, calendula, St. John's wort, thyme. Popular products include sea buckthorn, oak bark, cabbage juice, and honey.
Surgery is rarely used for mucosal hyperemia. Surgery is prescribed only for bleeding, when drug treatment is powerless.
We recommend: What is hypertrophic gastritis and why is it dangerous?
Drug treatment
Drug treatment is aimed at healing erosion, protecting the mucous membrane, stabilizing the tone of the lower sphincter muscles and normalizing the acidity of gastric juice.
Certain groups of drugs are used:
- Prokinetics. Drugs in this group increase the tone of the lower esophageal sphincter. Motilium and motilak are prescribed, the active component of which is droperidone. Genaton, the active ingredient of which is itopride, is also used.
- Antacids. Helps reduce acidity by neutralizing hydrochloric acid. In most cases, almagel, almagel a (for severe pain after eating), phosphalugel, and maalox are prescribed.
- Antisecretory drugs. Medicines in this group reduce acidity, reducing its production. The choice is often made between omeprazole and famotidine.
The duration of therapy and the number of drugs are chosen by the doctor based on the severity of the disease. Treatment lasts 6 weeks. In some cases, the duration of the course can be two months.

Chronic enterocolitis
Chronic enterocolitis is a simultaneous inflammation of both the small and large intestines, which is characterized by atrophy of the mucous membrane lining the inner surface of the intestines, which causes disruption of intestinal functions. Depending on the location of the inflammatory process, the disease is classified for the small (enteritis) and large intestines (colitis) separately.
The causes of chronic enterocolitis are due to the impact on the human body of the following pathological factors:
- long-term malnutrition;
- impaired immunity and metabolism;
- hormonal disorders, stress;
— intoxication with medications and chemicals;
- structural features of the intestine;
— diseases of internal organs;
- intestinal and parasitic infections.
One of the most common pathogens of chronic enterocolitis is intestinal lamblia (photos of these parasites can be seen in the article). They can multiply quickly and cause giardiasis. Signs of the disease include diarrhea, excess gas, abdominal cramps and pain, nausea, and vomiting. Giardia, the photo of which is presented in the picture, exists in two forms: active and inactive. Active forms of parasites live in the human body; when released along with feces, they turn into an inactive form and spread the infection outside the body.

Chronic enterocolitis often results from untimely or poor-quality treatment of acute forms of inflammatory bowel processes. In addition, there is a risk of transmission of the disease by inheritance and in people who were bottle-fed in infancy.
Surgical treatment
Indications for surgery are the failure of long-term drug treatment, as well as the appearance of esophageal strictures. Surgical intervention is necessary for the development of Barrett's esophagus, when there is a risk of malignancy. Indications for surgery include regular esophageal bleeding, a combination of reflux esophagitis with bronchial asthma that cannot be adequately treated, and frequent aspiration pneumonia.
The operation is performed by Nissen fundoplication. The goal of surgery is to restore normal functioning of the cardinal sphincter.
Symptoms of erythematous gastroduodenopathy
The most common symptom of erythematous gastroduodenopathy is heaviness in the stomach that occurs after eating.
Moreover, for the symptom to appear, the patient does not have to overeat; heaviness occurs even after a snack. Sometimes this condition is accompanied by severe nausea, which is difficult to cope with. This is due to the fact that when the mucous membrane becomes inflamed, the production of enzymes is disrupted, food digestion proceeds slowly, causing discomfort. If the foci of redness are located in the antrum and spread to the area of the duodenal bulb, peristalsis suffers: the food bolus has difficulty moving through the digestive tract, stagnates in the lower parts of the stomach, causing the patient bloating, unpleasant belching of air, heaviness in the epigastrium and disorders intestinal activity. Pathology in this case provokes constipation or diarrhea.
If erythematous gastroduodenopathy with an erosive component is detected, pain syndrome is added to the above symptoms. This condition is dangerous due to its rapid degeneration into erosive gastritis or peptic ulcer. Therefore, the doctor must explain to the patient the need to follow a gentle diet.
The common symptoms of erythematous gastroduodenopathy include the following:
- weakness, fatigue, increased irritability;
- lack of appetite, stomach discomfort;
- anemia associated with impaired absorption of nutrients;
- weight loss;
- periodic vomiting not associated with poisoning;
- plaque on the mucous membranes of the mouth, especially on the tongue.
Painful symptoms disappear if the patient’s regimen and diet are normalized. If you ignore periodic ailments, the pathology will quickly develop complications and first transform into gastritis, and later into peptic ulcers. The signs of erythematous gastroduodenopathy in the acute stage or during initial detection are similar to the symptoms of exacerbation of chronic gastritis. Therefore, treatment and nutrition for acute conditions are similar to treatment recommendations and diet for chronic gastritis.
The inflammatory process in gastropathy is often less pronounced than in true gastritis, and only the superficial layers are affected, which is why it is often called superficial gastritis.
The appearance of inflamed areas on the surface of the stomach is often accompanied by pain that occurs in the center of the abdomen. This pathology may be accompanied by swelling of the epithelium, increased sensitivity, and excessive mucus synthesis.

The appearance of erythematous gastropathy is due to the influence of various damaging factors on the gastric mucosa. As a result of the negative influence of such factors, the formation of erythema occurs - redness caused by blood flow to the affected areas of the membrane.
Often, simultaneously with this disease, erythematous gastroduodenopathy appears - redness and the formation of an inflammatory process in the mucous membrane of the pylorus of the stomach and duodenum.
Both conditions are not independent diseases; these symptoms are diagnosed during clinical examinations for other diseases. If they are detected, it is recommended to start drug treatment as soon as possible and change your lifestyle and diet.
But in the presence of the above pathologies, there is a risk of developing a third symptom - erythematous bulbopathy - an inflammatory process in the loop connecting the duodenum with the intestine.
Complications
Neglect of the disease can lead to quite serious complications. There is a possibility of manifestation:
- Esophageal ulcers. A complication occurs with prolonged and regular reflux. The condition is often accompanied by bleeding, which requires endoscopic surgery.
- Stenosis of the esophagus, that is, there is a narrowing of the lumen of the organ. It occurs as a result of chronic inflammation of the esophagus, when thickening of the organ wall is recorded. The patient begins to complain of a feeling of a lump in the throat, and the swallowing process becomes difficult. Treatment of this complication is organized only surgically and is quite complex.
- Barrett's esophagus. With this complication, the epithelium of the esophagus is replaced by the epithelium of the stomach, which leads to an increased likelihood of developing esophageal cancer.
Classification
This disease has a specific classification:
- Focal atrophy of the gastric mucosa is characterized by the appearance of pathological foci in the connective tissue in place of the dead glands of the inner lining. The lesions have different sizes and shapes; their morphological structure and appearance resemble an atrophic scar on the skin of the face - a pink, flabby area with noticeable borders. Focal atrophy is dangerous because there are often no symptoms during its development.
- Focal atrophy of the mucous membrane of the antrum of the stomach is a type of pathological process that is characterized by damage to the distal part of the stomach and the death of the glands responsible for the production of hydrochloric acid and pepsin. As a result, the walls of the stomach begin to become inflamed. With an old course, bacterial damage and the development of ulcers may occur.
- Moderate atrophy, which can be mild, severe and moderate. A weak one is characterized by a slight change in the main glands. For moderate, negative measurements are more significant, in addition, the formation of pathological areas is observed. Severe atrophy is characterized by extensive necrotic lesions.
Folk remedies
The therapeutic course of reflux esophagitis also includes traditional methods of treatment. Taking decoctions and tinctures of medicinal herbs and plants helps normalize the acidity of gastric juice and activate the restoration of damaged esophageal mucosa. The integrated use of drug therapy and folk remedies makes it possible to treat pathology in a short time and improve the quality of life.
Treatment fees
- You need to take chamomile, flax seeds, licorice root, lemon balm leaves in a ratio of 2:2:1:1. All ingredients need to be crushed and poured into 1 liter of boiling water, then boil the resulting composition in a water bath for 10 minutes. The healing drink must be infused for 2 hours, then filtered. You need to take 4 times a day, 50 ml.
- You need to take calamus root, anise fruits, jasmine, oregano, mint, fireweed, calendula in equal proportions and in crushed form. 2 tbsp. L. The collection needs to be poured with 500 ml of boiling water and kept in a dark place for 20 minutes. Afterwards, the tincture needs to be filtered and drunk 100 ml 5 - 6 times a day.
Plantain and celery juice
- Juice from medicinal herbs can be replaced with gruel, which can be obtained by grinding plants in a blender (1 tbsp per day, before meals).
- If the choice is juice, then freshly squeezed plantain and celery juice (1 tbsp) is recommended to be diluted in 250 ml of water and taken before meals.
Potato juice
Freshly squeezed potato juice has beneficial properties. The healing drink should be taken daily in the morning on an empty stomach 30 minutes before breakfast. You can replace the juice with gruel from raw potatoes.

Chamomile tea
Chamomile has an anti-inflammatory and enveloping effect. Promotes activation of the regeneration process, relieves spasms and inflammation. You can prepare chamomile tea by pouring 1 - 2 tbsp. L. Plant flowers 200 ml boiling water. The composition should be infused for 10 minutes and taken before meals.
Dandelion syrup
You need to fill a 3-liter jar with dandelion flowers, sprinkling granulated sugar (0.5 kg) on top. After adding the sugar, you need to compact the contents of the jar until the flowers begin to release juice. The resulting syrup is used 3 times a day, diluting a teaspoon in 100 ml of water.
Flax seeds
A tablespoon of flaxseed should be poured into 100 ml of water at room temperature. The resulting composition must be infused until mucus is released. Should be taken on an empty stomach.
Infusion of chamomile and wormwood
You need to take one teaspoon each of crushed wormwood and chamomile flowers and pour 200 ml of boiling water. The resulting composition must be wrapped and placed in a dark place for an hour. The tincture should be taken three times a day, 1⁄4 cups each.
Etiology of occurrence
To get rid of erythematous gastropathy (gastroduodenopathy), it is necessary to identify and eliminate the damaging factor that caused it. The occurrence of this pathology is provoked by the following reasons:
- poor nutrition: excessive consumption of spicy, fried, salty, smoked foods, abuse of fast food, carbonated drinks, etc. ATTENTION! Eating such food before the FGDS procedure provokes the appearance of foci of hyperemia on the endoscopic picture;
- taking certain types of medications that affect the condition of the digestive tract mucosa (NSAIDs, glucocorticosteroids, antibiotics, anticoagulants, etc.);
- infectious factor. The development of this gastropathy is promoted by certain bacteria, in particular Helicobacter pylori, and fungal pathogens;
- reflux of bile into the stomach, exposure to hydrochloric acid during long intervals between meals;
- stress factors: anxiety, lack of sleep, nervous and physical overload;
- bad habits: smoking, alcoholism;
- hormonal dysfunction and metabolic disorders;
- congestion in the digestive tract;
- hereditary factor;
- concomitant diseases can trigger the etiological mechanism for the appearance of gastropathy (pancreatitis, cholecystitis, enteritis, etc.);
- ischemic manifestations in the gastric wall;
- food and drug allergies.
Erythematous gastropathy can be caused by the following reasons:
- Disruption of the circulatory process.
- Presence of pathogenic microorganisms or fungal infection. More often, the cause of the disease is the active activity of the bacterium Helicobacter pylori. In this case, treatment is aimed at getting rid of the provoking factor.
- Chemical burns.
- Infectious diseases.
- Medicinal (medicinal gastritis). The causes of this type of gastropathy include taking aspirin and non-steroidal anti-inflammatory drugs.
- Heredity.
- Poor nutrition.
- Excessive drinking and smoking.
- Daily routine and stress resistance are of no small importance. Under the influence of psychotraumatic factors, the synthesis of adrenaline increases. It affects the growth of hydrochloric acid production, and its prolonged exposure leads to irritation of the mucous membrane of the digestive organ, provokes redness, inflammation, and in some cases causes the formation of ulcers and erosions.
Diet
The nutrition of patients with reflux disease should be fractional. Meals should be in small portions, taking into account that the stomach is filled to only a third of its volume. You need to eat 5-6 times a day; after eating, it is recommended to take a quiet walk.
It is necessary to completely exclude alcoholic beverages, fruit juices, and carbonated drinks from the diet. You need to give up pickled, smoked, salty foods, chewing gum, fatty and fried foods. It is not allowed to consume foods that increase gas formation (cabbage, rye bread, legumes). It is not recommended to include in the diet foods that relax the function of the lower sphincter and provoke stagnation of the food bolus in the stomach. These products include sweets, strong tea, and chocolate.
The diet should include boiled eggs, low-fat cottage cheese and milk, other low-fat fermented milk products, meat and fish soufflé, cutlets and meatballs from lean fish meat, steamed or in the oven, as well as cutlets from veal and poultry. Eating homemade crackers or day-old bread is beneficial. The diet can be enriched using baked apples.
Compliance with the diet is very important, since treatment cannot be effective if the acidity of gastric juice is not normalized and irritation of the gastrointestinal mucosa constantly occurs.
Causes of erythematous gastropathy
Most often, the cause of the development of this condition is an improper diet - consumption of foods that negatively affect the gastric mucosa. In addition, the mode in which you work and rest, as well as how resistant your body is to stress, has a great influence.
Pathogenic microorganisms and fungi that disrupt the functioning of the stomach can have a negative effect on the gastric mucosa.
Another reason for the appearance of such symptoms is a disturbance in the metabolic process. Some medications can also have a negative effect on the mucous membrane (by irritating it).
Erythematous gastropathy can also be hereditary - if one of your close relatives has been diagnosed with a similar diagnosis, this increases the risk of developing it in you. Another reason is the presence of bad habits, as they contribute to the occurrence of gastrointestinal pathologies.
Certain diseases of the digestive system, such as cholecystitis, colitis, enteritis, pancreatitis, can also become etiological factors of erythematous gastropathy.
Forecast
Reflux esophagitis, in most cases, has a favorable prognosis for ability to work and normal life. There is no threat or reduction in life expectancy if there are no complications. Timely treatment is a guarantee of preventing relapses and progression of the disease.

Diet for cardia deficiency
If the sphincter is weak, split meals are useful. You need to eat often, but in small portions. If you eat too much food at one time, the rosette of the cardia will stop closing. The following nutritional principles must be observed:
- After eating, you cannot lie down for 2 hours, you can only walk or stand.
- You should eat food in semi-liquid form: porridge, low-fat broths.
- You can't overeat in the evening.
- You need to exclude chocolate, spicy, fried and fatty foods. Excessive amounts of salt and coffee can also aggravate symptoms of the disease.
- The consumption of alcohol and carbonated drinks is strictly prohibited.
- During each meal, you do not need to fully load your stomach.
- Food should not be too hot or too cold.
Drug treatment for erythematous gastroduodenopathy is rarely prescribed. The main therapeutic method in this case is diet. Don't be alarmed and think that your diet should be reduced to diet soup and cereals, this is not so. On the contrary, the daily food set should be varied in order to provide the body with the necessary substances.
The restrictions apply only to frankly unhealthy foods - smoked meats, marinades, too hot and too cold dishes. You should not drink alcoholic and carbonated drinks, overeat heavily, or “sit” on coffee alone throughout the day. A sick stomach should not be empty, so carefully consider your daily diet.
To help, we suggest you familiarize yourself with the material, where we examined in detail the principles of nutrition for superficial gastritis. Dietary recommendations for this disease and erythematous gastroduodenopathy are identical.
Prevention
You can prevent the occurrence of reflux esophagitis by following a healthy lifestyle. It is necessary to avoid stress, not drink alcohol, eat spicy, sour, fried foods in moderation, giving preference to boiled and baked dishes made from healthy foods.
You need to eat a balanced diet, at the same hours, you should avoid late dinners, you should not take a horizontal position after eating or sit for a long time. Activity and mobility, physical exercise, walks after eating the main meal help normalize the digestion process and prevent the occurrence of various gastrointestinal disorders, including reflux.
Recommended:
- Adjust weight;
- Sleep on a bed with a high headboard;
- Stop smoking;
- Stop the habit of drinking water with your meals.
Treatment of erythomatic reflux esophagitis should be started in the early stages, which will stop the progression of the disease and prevent the occurrence of complications, sometimes incompatible with life.
Prognosis and prevention
If the disease is treated promptly and effectively, it does not pose a threat to life. A negative prognosis will occur when the disease is advanced and leads to the development of malignant neoplasms, as well as in the presence of pernicious anemia.
Having studied the causes of the development of gastropathy, it is recommended to design prevention methods in such a way as to protect your body from negative external and internal influences. First of all, you need to monitor your diet, give up bad habits, not abuse medications, and avoid stressful situations. In order to minimize the risks of relapses in gastropathy and prevent further development, patients need to:
- follow all recommendations and prescriptions of the doctor;
- eradicate bad habits;
- constantly fight excess weight;
- adjust nutrition.
Sources: https://gastri.ru/gastropatiya-chto-eto-takoe.html https://teamhelp.ru/gastroenterologiya/giperemicheskaya-gastropatiya-chto-eto-takoe.html gastrit.guru/lechenie/gastropatiya-chto- eto-takoe.html https://ilive.com.ua/health/gastropatiya-zheludka-chto-eto-takoe-i-kak-lechit_124297i15938.html https://etozheludok.ru/zabolevania/osnovnye/gastropatiya-zheludka. html gastrit.pro/lechenie/gastropatiya/ lovenlive.ru/gastropatiya-zheludka-chto-eto-takoe-i-kak-lechit.html This material is exclusively subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/19/2020
Symptoms
As a rule, in the early stages of erythematous gastroduodenitis, clinical manifestations are mild, and in some cases completely absent. The following signs of the disease should alert a person:
- feeling of discomfort in the stomach after eating;
- burning sensation in the stomach;
- nauseating state;
- general weakness;
- decreased appetite;
- stool disorders;

- increased gas formation;
- belching;
- heartburn.
Advice! The reason to visit a doctor should be the presence of at least one of the symptoms.
Classification of the disease
The method for diagnosing this pathology is fibrogastroduodenoscopy. This is the most reliable way to determine hyperemic areas in the digestive tract. The doctor uses a special device - an endoscope - to examine the esophagus, stomach cavity and duodenum. In some cases, biomaterial is collected for histological examination.
During the procedure, various parameters of damage to the mucous membrane of the digestive tract are assessed in order to make a correct diagnosis and assess the patient’s condition. Depending on them, there is the following classification of erythematous gastropathy.
According to the form of manifestation
In this case, the extent of the area of hyperemia is assessed.
- The focal form is characterized by limited (local) damage, the inflammatory process occupies a small area of the mucosa. This condition rarely develops into gastritis; it often occurs situationally due to errors in nutrition or as a reaction to taking certain medications.
- The widespread, or diffuse form, has a diffuse nature; erythema can be detected in different gastric sections, covering a large surface of the tissue. In the absence of proper treatment, it can lead to complications - gastritis and peptic ulcers.
Classification in this case includes an assessment of the condition of the mucosa, measures of the impact of damaging factors on the membrane.
- Erythematous gastropathy of the first degree of inflammation is characterized by initial manifestations of damage to the gastric epithelium, with no signs of advanced disease;
- The second degree indicates the progression of the process as a result of the ongoing negative impact of damaging factors on the epithelium. In this case, the process becomes a chronic form of gastropathy or gastritis.
IMPORTANT! This condition usually occurs in the absence of treatment or with inadequate therapy.
Traditional methods of treatment

Therapy with home remedies can only be carried out as an addition to the main treatment. Before using traditional medicine, you should consult your doctor. When treating insufficiency of the esophageal cardia, the following traditional medicine recipes are used:
- Juice is squeezed out of plantain leaves and taken 1 teaspoon before meals during an exacerbation of the disease.
- A mixture of St. John's wort, motherwort and valerian herbs is brewed in equal proportions, filtered and taken with honey.
- Dandelion flowers are ground with sugar to form a syrup. Dissolve 1 teaspoon of the composition in a glass of water and drink before meals.
- Cumin (1 teaspoon) is brewed in a glass of boiling water and drunk before meals. This drink perfectly relieves spasms in the gastrointestinal tract.
We can conclude that cardia failure is accompanied by unpleasant symptoms. Such manifestations also occur in other gastrointestinal diseases. Therefore, you should not try to diagnose yourself. You need to contact a gastroenterologist as soon as possible for diagnosis and treatment.
For erythematous gastroduodenopathy, it is allowed to be treated with traditional methods. Herbal infusions gently relieve inflammation of the mucous membrane and help restore damaged mucous membranes. We offer you several simple herbal medicine options for the stomach.
The main component of this collection is yarrow. 50 grams of dried crushed yarrow flowers and herbs are poured into 400 ml of water and boiled over low heat for 40 minutes. After the broth has cooled, it is filtered and taken warm, a third of a glass, before main meals.
To prepare this decoction, prepare a mixture of the following components:
- centaury;
- yellow gentian;
- chicory flowers;
- fumaria officinalis;
- yarrow;
- St. John's wort.
Do not be alarmed by such variety - the raw materials for preparing the decoction are sold in any pharmacy. Mix the ingredients in equal quantities, take 3 tablespoons of the prepared mixture and pour 400 ml of boiling water. Seal tightly and leave for 4 hours. Strain the broth and take it warm before your main meals - breakfast, lunch and dinner.
These recipes are given in the “Newest Therapist's Handbook”, written by the famous Russian doctor, E. A. Nikolaev.
The rate of progression of erythematous gastropathy directly depends on the time of exposure of the gastric mucosa to damaging factors. The sooner the cause that caused tissue hyperemia is identified and eliminated, the faster the recovery will occur.
First of all, it is recommended to follow a proper diet. Food is steamed, irritating foods are excluded: hot, spicy, salty, smoked foods, carbonated drinks, alcohol, coffee. It is advisable to replace black tea with herbal tea or plain water. Liquid porridges, lean meats and fish, jelly, broths, cottage cheese, egg whites, and jelly are recommended for consumption. Food should be warm; excessively hot or cold food additionally irritates the mucous membrane and causes spasm of smooth muscles.
In addition to the diet, it is necessary to follow a diet. It is recommended to eat meals at intervals of 2-3 hours. Portions should be small (about 350 g) so as not to overload the digestive tract. Overeating should be avoided, after which the excess food rots in the stomach, which is accompanied by symptoms of belching, nausea, and heaviness.
IMPORTANT! If the underlying cause of erythematous gastropathy was errors in nutrition, then following a diet for a week should contribute to the positive dynamics of the condition.
If hyperemia of the gastric lining occurs as a result of taking medications, it is advisable to abandon them if possible, or replace them with others that have a milder effect. If this is not possible, in order to mitigate the irritating effect on the mucous membrane, these drugs are combined with stomach supporting medications.
For example, forced use of drugs from the NSAID group (nimulid, ketanol, paracetamol, etc.) can be combined with the use of antisecretory drugs (Omez, Omeprazole, Kvamatel, etc.). It is also advisable to alternate taking irritating drugs with antacids (Almagel, Phosphalugel). However, this should be done with an interval of about 2 hours between them, in order to avoid a decrease in the medicinal effect.
It is necessary to give up bad habits, in particular smoking. It is also recommended to minimize stress factors and establish an optimal work and rest schedule.
Drug therapy is prescribed based on a comprehensive assessment of the patient’s complaints and diagnostic criteria. For increased acidity, it is recommended to take proton pump inhibitors, which have an antisecretory effect. Astringents, gastroprotective agents (bismuth preparations), antacids with an enveloping effect (Almagel, Maalox, etc.) are prescribed.
Surgical treatment of this pathology is carried out in very rare cases when drug therapy is unsuccessful. It is carried out by resection (removal) of the affected areas, access to which occurs through the oral cavity and esophagus into the stomach. This method ensures minimal tissue trauma.
Treatment with traditional methods in combination with medications contributes to a faster recovery. For this, infusions and decoctions of herbs are used, for example, a gastric mixture, which can be purchased at a pharmacy. Oat decoction has an enveloping effect; for low acidity, fresh cabbage juice is used. Before using any folk remedies, it is recommended to consult with your doctor.
The essence of pathology
Erythematous gastropathy is hyperemia of the gastric mucosa, identified during fibrogastroduodenoscopy. Additionally, during the study, swelling of the epithelium, its vulnerability, and increased mucus production may be present.
This endoscopic syndrome occurs as a result of the damaging effects of various factors on the lining of the digestive tract. As a result, erythema occurs - redness caused by a rush of blood to the affected area. Damage is observed on the surface of the tissue and does not affect the deeper layers.
This condition is not a disease, but it is characteristic of superficial chronic erythematous gastritis. With this option, gastropathy persists for a long time; in the absence of adequate therapy, it can develop into more serious diseases, for example, an ulcer.

If there is hyperemia of the epithelium in the endoscopic picture, additional diagnostic tests may be required: for the presence of a bacterial infection (Helicobacter), for determining acidity, in some cases, a biopsy is taken from the affected areas.
Sometimes this symptom does not manifest itself at all and is discovered by chance during a routine examination.
Gastroesophageal reflux disease
Gastroenterologist, head. Gastroesophageal reflux disease GERD, reflux esophagitis - morphological changes and symptom complex that develop as a result of the reflux of the contents of the stomach and duodenum into the esophagus. GERD is one of the most common pathologies of the digestive system, with a tendency to develop numerous complications. The constant increase in incidence requires a thorough study of the mechanisms of development of GERD, improvement of early diagnostic methods and development of effective pathogenetic treatment measures. The main factor in the development of gastroesophageal reflux disease is insufficiency of the lower esophageal sphincter. In healthy people, this muscular circular formation in its normal state keeps the opening between the esophagus and stomach closed and prevents the reverse movement of the food bolus due to reflux.