The chronic course of the inflammatory process of the stomach in some patients leads to modification of the cells of the internal epithelium. Polyps are formed. They can be located in any part of the organ and have a different morphological structure. The prognosis and treatment of the disease depend on histology. One of the variants of the pathology is a hyperplastic polyp of the gastric mucosa. This type occurs in people over 60 years of age, but sometimes in the middle age group. The doctor’s tactics in the question of whether to remove the formation are decided individually after examination.
Features and nature of the pathology
A hyperplastic polyp is an initially benign neoplasm characterized by the growth of mucous membrane into the organ cavity. The size of the tumor can reach 3 cm. In appearance, the polyp has a clear structure: body, base and stalk. Sometimes the stem may be absent; such growths are called flat. The base or stroma of the polyp has an altered mucosa with impaired regeneration of cellular structures.
Polyps never appear on healthy tissue. The formation is based on a violation of the integrity of the mucous membranes under the influence of various factors.
Hyperplastic polyps are diagnosed in the vast majority of all clinical cases. The main risks as the polyp grows are associated with malignancy of tumor cells and transformation of the growth into an oncological neoplasm.
Classification and types
The modern classification of pathological foci is determined by two main criteria: quantity and forms of changes in the mucous membranes of the colon.
By number
There are three main directions in the growth of polypous foci:
- Limited or localized (1-2 polyps in the rectal lumen);
- Multiple (2 or more pathological growths);
- Diffuse familial polyposis (there are up to hundreds of pathological units).
With multiple focal growths, the development of rectal polyposis occurs. With diffuse polyposis, growths cover almost the entire rectal cavity with neoplasms of different sizes from 0.4 mm to 1-2 cm. Find out what a rectal polyp looks like here.
Diffuse polyposis is almost always inherited; it can be diagnosed in infants with autoimmune diseases if parents or close relatives have a history of multiple familial polyps.
According to the form of the neoplasm
There are 4 main forms of hyperplastic polypous foci:
- Adenomatoses or adenomatous polyps (most often degenerate into malignant ones; clinicians characterize adenomatosis as a precancerous condition). Adenomatous tumors are classified into the following subtypes: Tubular type (foci of a pinkish tint with a dense structure and a smoothed surface);
- Villous (the growth appears as branch-like growths resembling small villi, the body and base are filled with multiple vascular weaves);
- Tubular-villous (mixed type, based on changes in the hypertrophied mucosa of the tubular and villous type).
Hyperplastic forms of polyps are characterized by elongation of the tubes of epithelial structures with an increased tendency to cystic transformation.
Note ! According to the results of long-term observations, all hyperplastic neoplasms grow and change. When transformed into adenomatosis, such growths are most prone to cell malignancy.
Hyperplastic polyps of the sigmoid colon
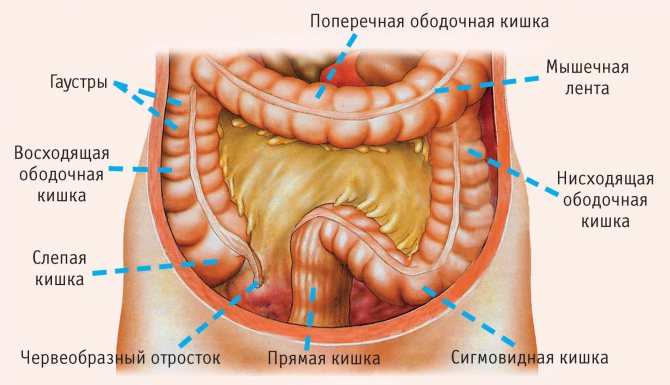
The sigmoid colon is a large distal section of the intestine, up to 70 cm long. The normal lumen diameter reaches 4 cm. The main function is the absorption and distribution of nutrients.
It is in this segment that most of the liquid and vitamins are absorbed. This is where the formation of primary feces begins. With the formation of hyperplastic polyps, the diameter of the sigmoid colon can expand, and the functionality of the organ is often impaired.
Polypous formations of the sigmoid colon are predominantly benign, and the localization is atypical. In terms of numbers, a localized single polyp (1-2 units) is formed in this section.
The spread of hyperplastic polyps accounts for 3-5% of all cases of polyposis disease of various parts of the intestine. However, clinicians are confident that the figures are significantly underestimated due to the lack of primary symptoms in many patients with small tumors.
Symptoms
The initial stages of growth formation in the transverse colon are asymptomatic. In patients, the presence of growths is discovered accidentally during endoscopy, the reason for which was another medical diagnosis.
In addition, early diagnosis is complicated by the fact that the clinical picture of this pathology has much in common with other diseases of the digestive tract. Symptoms of the pathogenic process appear along with active reproduction and growth of polyps. The patient notes:
- stomach ache;
- alternating constipation and loose stools;
- weakness;
- tendency to lose weight;
- the presence of mucus and bloody impurities in the stool;
- pain symptom during bowel movement;
- onset of relief and subsidence of pain after defecation;
- internal bleeding and anemia;
- physical exhaustion of the body;
- constant feeling of fullness in the intestines;
- As the growths grow, the skin near the anus becomes moist and itching appears.
Morphological picture of a hyperplastic type polyp
The tactics for managing patients with hyperplastic polyps is determined by the morphological structure of the neoplasm. The results of histology after taking a biopsy specimen during a biopsy usually definitively determine the degree of cancer risk.
The following indicators are taken as the main evaluation criteria:
- Structurality (outline, contours, tuberosity);
- Density;
- The presence of atypical cells;
- Component tissues of the body and stroma (glands, connective tissue, muscle fibers).
The main features of hyperplastic polyps are branched, elongated and significantly curved dimples, which are lined from the inside with foveal epithelium. In the stroma, chaotically located bundles of muscle structures are noted against the background of active inflammation. In 20% cases of active dysplastic process are registered.
During histology, each sample is cut and each section is examined under a microscope so as not to miss the presence of atypical cells and the onset of the oncological process. The larger the size of the tumor, the higher the risk of malignancy of tumor cells of the cancer type.
Diet
Food is something with which the gastrointestinal tract is constantly in contact. Therefore, what a person eats and how he does it directly determines the health of his digestive tract. In addition to treatment and observation, the patient at any stage is prescribed an appropriate nutritional system, which involves avoiding harmful foods and following a regimen. A diet for polyps is prescribed by a doctor; it is therapeutic and has strict restrictions. After removal, it is recommended to permanently switch to a healthy diet.
Important! You should give up not only unhealthy foods, but also alcohol and smoking.
Development mechanisms and causes
The true cause of pathological growths of the mucous membrane has not been reliably identified. Rather, it is a complex of provoking factors, congenital or acquired, simultaneously affecting the intestines.
The main predisposing factors are considered:
- Poor nutrition and bad habits . Fried, salty foods, preference for hot and spicy dishes, constant exposure to alcohol, in particular beer and cocktails, disrupt the microflora of the stomach and intestines. Deposits of bad cholesterol for this reason increase the development of various intestinal diseases.
- Diseases of the gastrointestinal tract . Typically, polyps appear on pathologically altered tissue: inflammation, erosive lesions, Helicobacter pylori lesions, colitis, dyskinesia, Crohn's disease - all this contributes to the formation of pathological lesions. In such cases, polyps are secondary in nature, forming as a complication of the underlying disease.
- Hereditary predisposition . Foci of polyposis occur even in newborns whose parents have a history of intestinal pathologies, rectal and colon cancer. This also includes spontaneous intrauterine mutations, which result in changes in the anatomy of the newborn’s intestines and disruption of cell division of mucous tissues.
- Constipation and unstable stool . Regular constipation, and even more so their inadequate treatment, often provokes changes in the mucous membranes of the organ, disrupting the processes of natural secretion and production of enzymes and the mucous component. Atrophy leads to the proliferation of pathologically altered tissue.
The risk group includes patients with:
- high body weight,
- hormonal disorders,
- autoimmune diseases that are associated with impaired cell division.
In addition, the older the patient, the higher the risk of developing polyps in the colon. Weak physical activity, unconventional sex, inadequate drug treatment, the recovery period after complex abdominal operations on the epigastrium - all this can become provoking factors in the formation of the disease.
Prevention
General recommendations for avoiding the growth of polyps in the duodenum or their recurrence, as for any intestinal disease, are:
- quitting smoking and alcohol;
- a gentle diet or a balanced, proper diet;
- active lifestyle;
- a sufficient amount of clean, high-quality water to drink;
- avoid or deal with stress;
- do not get carried away with uncontrolled use of medications and traditional medicine;
- be examined by a gastroenterologist at least once a year.
Recurrence of polyps occurs on average two years after their removal. To prevent them, you need to be registered with a specialist, regularly undergo examinations prescribed by him, and follow all his recommendations.
We recommend: What is steatorrhea and how to treat it
Clinical manifestations
The first signs of proliferation of the mucous membranes of the rectum are always blurred or absent altogether, which often explains the need to consult a doctor only when the size of the polypous lesion is significant.
The main features are:
- Pain during bowel movements;
- Persistent bowel dysfunction;
- Atypical discharge with feces (blood, mucous component, exudate, pus);
- Itching and constant wetting of the anus;
- The development of anemia as a result of internal bleeding.
Considering the development of polyps against the background of existing diseases, we can note an exacerbation of chronic inflammation such as paraproctitis, a deterioration in the patient’s general condition, and malaise. Typically, such symptoms are also characteristic of other diseases, so it is important to conduct a thorough differential diagnosis.
A little anatomy
The colon is a large section of the large intestine that is slightly shaped like a rim. It consists of the ascending colon, transverse and descending regions. The joints at an angle are called the hepatic, splenic flexure due to their location near the corresponding organs - the liver and spleen. Connection with the rectum through the rectosigmoid region.
Research methods
Given the weak clinical manifestations and the combination of signs with symptoms of major diseases of the epigastric organs, primary diagnosis is often difficult.
The goal of differential diagnosis is to exclude:
- exacerbation of hemorrhoids,
- intestinal endometriosis,
- paraproctitis,
- proctitis,
- parasitic infections,
- some stomach diseases.
The main research methods are:
- General clinical tests (feces, urine, blood, anal mucus);
- Studying the patient’s clinical history and complaints;
- Palpation of the peritoneal organs;
- Rectal examination (if possible).
Instrumental research methods are considered mandatory, which are usually the final stages in determining the final diagnosis.
The following special studies are highlighted::
- Irrigoscopy . X-ray research method using a contrast agent. Allows you to examine changes in the mucous membranes, contours, polypous lesions larger than 1 cm. Read more about how irrigoscopy differs from colonoscopy in this article.
- Colonoscopy . A collective term for many endoscopic examinations of all parts of the intestine (for example, sigmoidoscopy). The method involves studying the intestinal mucosa from the inside. During the manipulation, it is possible to immediately remove polypous structures, biopsy, stop bleeding, and eliminate adhesions. A full description of colonoscopy is available in a separate article on our website.
- MRI or CT examination . Otherwise, virtual colonoscopy, which allows you to assess the degree of structural changes in soft tissues. Effective against large polyps. What a virtual colonoscopy shows in more detail here.
- Ultrasound intrarectal or superficial . It is an additional method of primary diagnosis to exclude acute inflammation of the abdominal organs, study the anatomy and other features of the gastrointestinal tract in the patient.
Note : adequate diagnosis makes it possible to differentiate many diseases from polypous lesions, to find out the nature and potential risks of malignant tumor degeneration based on the results of histological examination.
Symptoms
Single formations occur practically without manifestations. If the hyperplastic polyp of the stomach is large or spreads to several parts, the patient consults a doctor with complaints. Symptoms and treatment depend on morphological features.

The following clinical signs are characteristic:
- Heaviness and distension in the upper abdomen. Occurs immediately after eating or after 1.5-2 hours, disturbing for 2-3 hours. In some cases, pain is not associated with eating.
- Dyspepsia in the form of belching, bloating, nausea, vomiting.
- Decreased appetite, lethargy, fatigue.
- Unstable chair.
If complications occur, the following symptoms may occur:
- temperature increase;
- vomiting with blood;
- change in the color of stool in the form of melena;
- cramping pain in the epigastric region that spreads to the entire abdomen.
Important!
Progressive deterioration of the condition is an indication for immediate consultation with a specialist.
Diagnostics
The main method to confirm the diagnosis is endoscopy. If a hyperplastic polyp of the stomach is discovered during the examination, not only a biopsy is performed. Additionally, histological material is taken in several places around the element. Because areas of malignancy are more often detected near the formation.
Additionally, other studies are being conducted. Important information is obtained when:
- general blood test;
- tests for Helicobacter pylori infection;
- fecal occult blood test;
- radiography, CT scan with contrast.
Treatment tactics
Many clinicians consider any atypical neoplasms on the mucous membranes of internal organs to be a precancerous condition. An effective treatment is surgery.
Depending on the degree of polypous lesion, the nature of the growth and the type of localization, surgical tactics are chosen.
The following methods are used for removal:
- Polypectomy . The traditional method of excision of a polyp using an electric knife, followed by cauterization of the wound surface with a laser or electrodes. The operation is performed using a rectoroscope or colonoscope.
- Transanal section . The method allows you to remove polypous lesions in the lower or middle parts of the colon using a rectoscope or colonoscope. A special loop is placed over the polyp, which is compressed and the polyp is excised. Next, the wound site is cauterized with an electric charge to prevent bleeding.
- Laparoscopic polypectomy . It is used when localizing a polypous lesion in hard-to-reach places. It involves several incisions in the peritoneum and further manipulation using surgical instruments.
- Resection . A radical method of polyp removal, prescribed for metastases and malignant tumors, may involve complete removal of the colon or part of it along with the affected mucosa.
Attention ! Unfortunately, no operation guarantees the absence of potential oncogenic risks and the formation of a new lesion. In the overwhelming majority, surgery to remove polypous tumors is an adequate prevention against intestinal cancer.
Colonoscopy with removal of polyps (endoscopic polypectomy) is possible:
- free of charge within the framework of compulsory health insurance, that is, under the compulsory medical insurance policy, if there is a referral from a medical institution or a territorial health authority
— free of charge as part of high-tech medical care, if a previously performed biopsy confirms malignant degeneration of the polyp
- on a contractual basis at the request of the patient
Diagnostic colonoscopy, as well as removal of polyps during colonoscopy, can be performed with intravenous sedation (pain relief).
Recovery period
After removal, regardless of the extent of the operation performed, a course of rehabilitation therapy is prescribed. Recovery is based on the prescription of drug therapy, nutritional correction, physical therapy and traditional medicine.
Drug treatment
In the early and late postoperative period, a course of the following drugs is prescribed:
- Antibiotics (Ceftriaxone, Sumamed, Azithromycin) to prevent infectious complications;
- Antispasmodics (Drotaverine, No-shpa, Papaverine) to relax the intestinal muscles;
- Painkillers (Ibuprofen, Ketoprofen, Nurofen) for pain;
- Mild laxatives to prevent constipation (Duphalac, Microlax);
- Iron-containing drugs for the development of anemia due to internal bleeding.
A course of drug therapy is prescribed by a doctor based on multiple diagnostic criteria. Typically, after endoscopic surgery, medical recovery lasts about 14 days.
With resection, treatment can last up to six months, here it is prescribed:
- hormone therapy,
- enzyme replacement treatment,
- long-term antibacterial therapy.
To reduce postoperative infections, enemas with antiseptics (Chlorhexidine, Miramistin, Furacilin) can be prescribed.
Nutritional Features
The main prevention of complications is predetermined by adequate nutrition:
- Firstly , a therapeutic diet prevents the formation of hard stool and constipation.
- Secondly , the load on all organs of the digestive system is reduced. During the recovery period, the body directs all its forces to healing wounds, returning to its previous functionality, and it is difficult for it to digest complex foods. A rough diet can provoke the development of stomach diseases.
Healthy foods are:
- jelly, decoctions of berries without sugar, herbal infusions, green tea;
- simple soups with low-fat broth made from fish and meat;
- slimy porridges, all cereals except rice;
- steamed meatballs, cutlets (minced meat should be ground 2-3 times).
Proper nutrition in the long-term postoperative period significantly:
- alleviates the patient's condition,
- stimulate intestinal motility,
- promotes healthy cell regeneration,
- accelerated healing of even congestive inflammations, ulcers, and erosive lesions.
Diagnosis of the disease
To make an accurate diagnosis, the doctor conducts a comprehensive examination. The patient is prescribed the following procedures and tests:
- Ultrasound;
- sigmoidoscopy;
- colonoscopy and endoscopic diagnostics;
- CT and MRI;
- radiography;
- bacteriological studies of biological material;
- histology;
- biopsy.
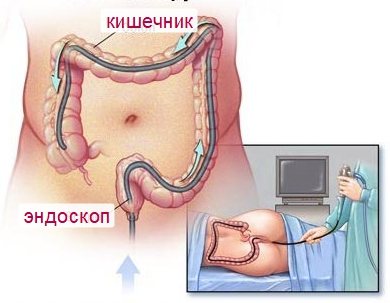
The most informative diagnostic methods are colonoscopy and radiography. These methods make it possible to distinguish polyposis of the colon from other pathologies of the gastrointestinal tract.