Nausea, frequent heartburn, pain in the upper abdomen - all these signs indicate a disruption in the normal functioning of the gastrointestinal tract. They are often accompanied by another characteristic phenomenon - belching with an unpleasant sour or bitter taste. Patients who come to a gastroenterologist with this set of symptoms may hear a diagnosis of gastritis with bile reflux syndrome.
How is bile reflux syndrome treated?
Characteristics of reflux lesions of the gastrointestinal tract
In official medicine, the disease is called “bile reflux gastritis type C.” So, what is reflux inflammation of the digestive organ - and can reflux be cured?
At the junction of the stomach and intestines, in the bile ducts there are special muscles in the form of a valve - sphincters that open or close the passage. When crushed food particles move from the digestive organ into the intestine, the valve opens and the contents from the epigastrium enter the duodenal intestine, then the muscle contracts, closing the cavity, and the digestion process continues in the intestine. Normally, the sphincters work synchronously to ensure proper digestive activity. When pyloric motility is impaired, undigested food remains, along with bile and enzymes, return to the antrum.
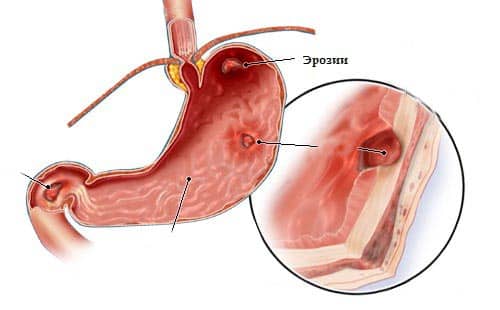
The aggressive intestinal mixture begins to corrode the walls of the organ mucosa.
In turn, hydrochloric acid from the gastric sections seeps into the duodenum with an alkaline environment, causing irritation and inflammation of the intestinal walls. The release of intestinal contents into the stomach and the reverse process is called reflux, and the resulting pathology is chronic reflux gastritis. This is due to the fact that, despite intensive treatment, the disease remains in the body forever, and the diet accompanying reflux gastritis must be followed by the patient for the rest of his life.
Diagnostics
The doctor becomes suspicious of the disease after careful questioning and clarification of the patient’s complaints, when the cause is identified. Special attitude towards persons who have undergone surgery. They are additionally examined by a surgeon. Indirect confirmation of digestive disorders is possible through blood and stool tests (scatology + occult blood).
The basis of diagnostics is hardware research. Fibrogastroduodenoscopy reveals foci of inflammation in the antrum, swelling of the epithelium, and widening of the sphincter opening between the duodenum and the pyloric part of the stomach.
Modern interpretation of gastritis requires assessment of the condition of the mucosa using a biopsy taken during fibrogastroduodenoscopy. In this way, the form of the disease is confirmed and the presence of epithelial metaplasia during the transition to cancer is checked.
To study the motility and contractility of the gastroduodenal zone, antroduodenal manometry or gastrography is used.
If necessary, daily pH measurements are carried out using the Gastroscan apparatus.
Acidity measurements using pH measurements and the use of a histamine test make it possible to study the influence of the level of acid formation in the stomach. X-ray of the stomach and intestines using a barium suspension helps to trace the movement of stomach contents, record violations of the contraction of the pyloric sphincter and reflux in the images. To check the participation of other organs of the digestive tract in the pathogenesis, an ultrasound of the abdominal cavity is performed.
Classification of reflux gastritis
Based on the nature and location of gastric damage, the following types of gastroreflux are distinguished:
- Superficial reflux gastritis, in which bile regularly leaks into the stomach, destroying the cells of the gastric walls. Instead, increased synthesis of new pathological cells begins in the stomach, which over time can develop into malignant tumors.
- Erosive reflux gastritis develops when, with several discharges of bile fluid, epithelial tissue is corroded and erosive foci form at the site of the lesion. The process is accompanied by severe pain in the stomach. Erosive gastritis, in which inflammation of the pyloric (antral) area of the epigastrium occurs with the formation of numerous ulcers, is called “erosive antral epigastric reflux.”
- Atrophic reflux gastritis is the most dangerous type of pathology, in which necrosis of the coolant is observed; as a result, the walls of the epigastrium are destroyed even when exposed to “native” gastric juice.
- Catarrhal reflux gastritis is characterized by severe damage to the walls of the organ, which affects its deep muscle tissue; swelling and dystrophic destruction of the gastric epithelium develops.
- Duodenal gastric lesion is a type of epigastric lesion as a result of harmful substances from the duodenal intestine entering it. The disease is provoked by increased pressure in the gastrointestinal tract, pathological changes in the mucous membrane of the duodenum, and weakness of the pyloric muscles.
- With biliary gastroreflux, complete atrophy of the sphincter muscles of the bile ducts and gallbladder occurs, and bile is poured into both the intestines and the stomach. They provoke pathology of endocrine and nervous system dysfunction. This is accompanied by clinical signs of classic gastritis - heaviness and fullness of the stomach, an unpleasant taste on the tongue, dyspepsia, stool disorders, intestinal gas pollution, dull and aching pain in the gastric region, weight loss, iron deficiency, and weakness.
Important information: What is superficial gastritis and how to treat it
Based on the degree of damage, focal and diffuse reflux are distinguished. When focal, certain areas of the epigastrium are affected; diffuse causes inflammation and ulceration of all organ walls. According to the intensity of manifestation, the pathology can be acute (the clinical manifestations are pronounced and proceed quickly) and chronic forms. Treatment of reflux gastritis should be carried out only as prescribed by the attending gastroenterologist.
Description of the disease
When the mucous membrane is damaged, it cannot perform its functions correctly. Pepsin enters the body in a “dormant” state, is activated in a reaction with hydrochloric acid, and begins to participate in digestion.
With atrophic gastritis, this pattern is disrupted. The acidity of the stomach decreases significantly, and its walls gradually become thinner. Dead cells are replaced by connective tissue. As a result, there is a deficiency of gastric juice.

The stomach cannot perform its functions correctly. At the initial stage, subatrophic gastritis is easy to treat, while chronic gastritis is difficult to treat. When the disease is advanced, not only a small area is affected, but also the entire stomach.
Important! The chronic form can provoke the formation of cancerous tumors.
Symptomatic manifestations
Symptoms of gastroreflux appear depending on the type and form of pathology.
The main characteristics common to all types are:
- pain in the solar plexus area;
- heaviness in the stomach after eating;
- regurgitation of air;
- heartburn;
- attacks of nausea;
- increased gas formation;
- sour or bitter taste in the mouth;
- when belching, pieces of food come out;
- unstable stool, alternating constipation and diarrhea;
- release of bile during vomiting;
- coughing attacks due to the entry of pieces of food from the stomach into the esophagus;
- loss of appetite;
- weight loss;
- dehydration;
- the corners of the lips begin to crack;
- signs of general malaise - weakness, fatigue, dizziness.
Specific signs of catarrhal gastric reflux:
- episodic pain, mainly after eating;
- gastric bleeding due to erosive lesions of the coolant, the development of proliferation and dysplasia, and then the death of organ cells;
- decreased production of gastric juice;
- white coating on the tongue;
- pale skin;
- blurred vision and brittle nails and hair due to vitamin deficiency;
- formation of various growths (cysts, polyps).
Symptoms
In the first stages of reflux gastritis, it can be expressed only by a slight disruption of the functioning of the gastrointestinal tract, which is why patients do not go to a medical facility in a timely manner.
As the pathological process progresses, symptoms of reflux gastritis will appear, such as:
- pain in the stomach, which will increase after eating or from prolonged fasting;
- bowel dysfunction - constipation is replaced by diarrhea and vice versa;
- attacks of nausea, which often end in vomiting. Vomit may contain impurities of bile or blood;
- increase in abdominal size;
- dryness and bitter taste in the mouth;
- severe heartburn and burning in the chest area;
- loss of appetite, resulting in weight loss;
- a feeling of heaviness in the stomach after eating, as well as rapid satiety from food;
- signs of general malaise - severe weakness and increased body temperature.
In cases where one or more symptoms appear, it is necessary to seek help from specialists as soon as possible, and not to try to eliminate the clinical manifestation of the disease on your own. This can not only aggravate the course of reflux gastritis, but also cause severe complications.
Reasons for the development of pathology
Gastric pathology with signs of reflux can be caused by the following reasons:
- weakening of sphincter muscle motility;
- surgical removal of part of the stomach;
- operations to narrow the duodenum;
- removal of the gallbladder;
- plastic and other operations on the epigastrium;
- anatomical displacement of the stomach;
- chronic forms of gastrointestinal pathologies;
- malignant neoplasms in the digestive organs;
- duodenal obstruction;
- increased pressure in the intestines;
- congenital pathologies in the structure of the gastrointestinal tract and valves.
Important information: What is hemorrhagic gastritis and methods of treatment
Factors that provoke the development of biliary gastroreflux:
- eating disorder;
- abuse of alcoholic beverages and tobacco products;
- inflammatory pathologies of the pancreas and gallbladder;
- formation of stones in the biliary tract, bladder and kidneys;
- long-term and uncontrolled use of medications that affect the coolant;
- emotional overload and stressful situations.
Types of subatrophic gastritis
Subatrophic gastritis can form due to various factors. The disease is divided into several forms:
- Chronic is accompanied by periodic relapses. The disease gradually progresses. As a result, complications arise in other internal organs (pancreas, duodenum, esophagus, liver). Chronic disease negatively affects the nervous system and blood supply.
- The catarrhal form is otherwise called superficial or simple. Accompanied by injury only to the superficial gastric layer. The catarrhal form refers to the initial stage of the disease and is treated quickly.
- Antral subatrophic gastritis is localized at the bottom of the stomach, next to the 12-point colon. Due to tissue proliferation and inflammation of the mucous membrane, the functioning of the stomach is disrupted.
- In the deep form, inflammation penetrates the walls of the organ, affecting the muscles. Certain areas of glandular epithelium degenerate into flat epithelium.
- The focal form appears in specific areas of the stomach. In acute manifestations of the disease, increased acidity is observed.
- The diffuse form is an inflammatory process that is not yet accompanied by serious degenerative changes. Only primary cell damage begins, the appearance of small ridges on the stomach.
- The erosive form is a pre-ulcerative condition. The disease has an acute or chronic form.
- Distal – inflammation affecting distant areas of the organ. This type of gastritis most often occurs in residents of megacities. The distal form may be acute or erosive.
Children's gastritis occurs in the same way as in adults. The symptoms are the same. An acute and chronic form is also observed. The autoimmune type appears due to the genetic characteristics of a person. Multifocal is closely related to the environment (consumption of toxins, nitrates in food, poor diet, Helicobacter pylori infection, etc.).
Diagnostic measures
In order to determine how to treat reflux, it is necessary to conduct a comprehensive diagnosis of the pathology.
Laboratory research:
- blood and urine collection for general analysis;
- biochemical studies of the material;
- stool occult blood test.
Instrumental research methods:
- Ultrasound of the gastrointestinal tract;
- FGDS or gastroscopy;
- biopsy and histological examination;
- X-ray of the gastrointestinal tract with injection of a contrast agent into the abdominal cavity;
- daily monitoring of stomach acidity levels.
To make a diagnosis, the symptoms characterizing reflux gastritis are studied, and treatment is prescribed by a gastroenterologist.
Principles of treatment
As a rule, traditional treatment is used for gastroreflux. Hospitalization of the patient is carried out only in case of dangerous complications of the disease.
Medication is prescribed in the following areas:
- to restore coolant, agents with an enveloping effect are prescribed - Omez, Epicurus, Lansoprazole, Omeprazole, Rabiet, Pariet, etc.;
- to reduce acidity levels - Tisacid, Rutacid, Phosphalugel, Almagel;
- restoration of gastric motility and intestinal peristalsis - Motilium, Motilak, Domperidon-Teva, Passazhiks;
- elimination of the main symptoms;
- to relieve excess bile - Ursosan, Ursofalk, Ursodez, Urdoxa.
As a means of supporting immunity, vitamin complexes containing B-vitamins and retinol are prescribed.
Special diet
Treatment is carried out in compliance with the principles of dietary nutrition. The diet for reflux gastritis should be gentle and not injure the gastric mucosa. Spicy, salty, fried foods, bread and baked goods, alcoholic beverages, sweets and smoked foods are excluded from the diet. Special nutrition for reflux gastritis of the superficial, erosive, catarrhal or biliary type is prescribed by a nutritionist.
Important information: What is catarrhal gastritis and how to treat it
For a disease such as reflux gastritis, the diet involves eating liquid, semi-liquid, boiled or steamed food (soups, purees, steamed cutlets, porridge boiled in water, eggs). During the period of remission, you can include juices and fermented milk products in the menu. Be sure to drink mineral water. Meals are fractional, 5-6 times a day in small portions.
Food should be warm.
Doctors recommend treatment with folk remedies as an additional therapy for a disease such as reflux gastritis. Attacks of heartburn are well relieved with flax and angelica seeds, a decoction of calamus and celery roots. These medicinal herbs have an effective enveloping effect and protect the gastric mucosa from irritation.
Diet and nutrition
The diet of a patient with reflux is aimed at reducing stomach overload. Therefore, you need to eat often (5-7 times), but in small portions, and do not overeat. You can’t go to bed to rest immediately after a meal; you need to move actively for about half an hour. Eating before bedtime and at night is prohibited. The food you eat should not be spicy and well cooked. Food is steamed, boiled or baked without adding fat. Changes are also made to the diet of such patients. It is forbidden:
- sweets containing cocoa;
- coffee and caffeinated drinks;
- fortified and alcoholic drinks;
- soda;
- spicy, fatty and spicy dishes;
- preservation and marinades;
- sour foods;
- fresh flour pastries.
The emphasis in nutrition is on vegetables, fruits, cereals, pasta and eggs are limited. You can have rabbit, veal, chicken, not fatty fish, but you should avoid pork and beef with hard streaks. The same applies to fatty fish.

Preventive actions
You can prevent the occurrence or exacerbation of gastric reflux pathology by following certain rules:
- healthy eating at regular times;
- diet;
- timely treatment of concomitant diseases of the abdominal organs;
- active lifestyle;
- rejection of bad habits;
- immune support.
For any manifestations of dysfunction of the digestive system (bitterness in the mouth, dyspepsia, stool disorders, stomach pain), it is better to visit a doctor and undergo qualified treatment. It is important to remember that biliary gastroreflux is a disease that requires immediate treatment.
Symptoms
The disease develops over years, without making itself felt for a long time. Minor dyspeptic disorders are rarely a cause for concern. When the symptoms become more pronounced, the process already progresses into the chronic stage, which is fraught with more serious consequences: malignant degeneration of cells, ulcers, damage to neighboring organs and systems.
You should consult a gastroenterologist if you notice the following symptoms:
- feeling of heaviness during or after eating;
- nausea;
- bowel problems (diarrhea or constipation);
- bloating, gurgling sounds;
- sour breath;
- white coating on the tongue;
- unpleasant heaviness in the epigastric region;
- irritability;
- lack of appetite, leading to weight loss up to anorexia;
- frequent belching.

Weakness, drowsiness, sweating are signs of anemia, which is inevitable when gastric secretion is impaired and subsequent deterioration of the trophism of the circulatory and nervous systems.
A deficiency of enzymes and hydrochloric acid affects the quality of food digestion, the supply of macro- and microelements to the body, and this leads to the manifestation of vitamin deficiencies: brittle nails, hair loss, poor condition of the skin and teeth.