Diffuse reactive changes in the pancreas (PG), which are detected during ultrasound examination, are not specific, but indicate the presence of a pathological process in it. Most often it is inflammation. Such a picture of the pancreas may be a finding in the case of ultrasound examination of other organs of the digestive tract. To clarify the causes of reactive changes, it is necessary to prescribe additional tests.
Causes of reactive changes in the pancreas
Among the pathologies of the digestive organs in children, reactive changes in the tissues of the pancreas are distinguished. They have some features:
- are a reaction to diseases of other digestive organs, therefore their nature of development is secondary,
- nonspecific, and are not considered a separate disease.
Therefore, a number of tests are required for differential diagnosis.
Diseases against which reactive changes develop most often include:
- complicated cholecystitis,
- ulcer of the stomach or duodenal bulb,
- colitis of various etiologies,
- hepatitis.
In the acute phase of these diseases, the structure of the gland tissue also changes. The process is slightly expressed, despite the clinical manifestations that cause discomfort. It is not always possible to determine such reactive changes in the pancreatic parenchyma using ultrasound; additional research methods are required in the form of laboratory blood and urine tests.

Infectious diseases lead to reactive pancreatic conditions:
- pneumonia,
- influenza and other acute respiratory viral infections,
- pharyngitis,
- stressful situations,
- acute intestinal infections or acute gastritis,
- viral hepatitis.
Reactive changes can also be caused by:
- improper diet,
- errors in diet: carbonated drinks, fatty, spicy, fried foods, canned foods,
- medications: antibiotics, diuretics, hormonals.
In children, congenital anomalies lead to disturbances in the pancreatic parenchyma and its reactive enlargement:
- cystic fibrosis,
- damage to the bile ducts,
- low hormone levels.
Causes
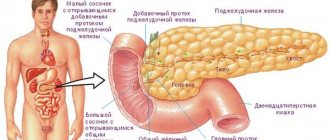
The pancreas is not only involved in the digestion process, but also produces hormones. Enzymes produced by the organ are part of pancreatic juice. When eating food, this liquid is released into the duodenum, where it binds to polysaccharide molecules and breaks them down.
The excretory duct of the gland is directly connected to the intestinal cavity. Therefore, inflammatory processes that occur in other parts of the digestive tract can spread to the pancreas. This is how reactive pancreatitis occurs. This pathological condition is characterized by swelling, inflammation, and dysfunction of the organ.
In most cases, this type of pancreatitis occurs in a chronic form and is not characterized by a clear clinical picture. Acute reactive inflammation usually occurs in the presence of congenital gastrointestinal pathology.

To diagnose reactive changes, it is necessary to perform an ultrasound
The most common causes of the development of reactive phenomena in the pancreas:
- taking antibacterial agents longer than recommended,
- abdominal injuries,
- eating disorders,
- abnormalities of the pancreas,
- inflammatory and other gastrointestinal diseases,
- infections,
- stress, prolonged significant psycho-emotional stress.
Disturbances in the structure of the parenchyma of a diffuse nature can also be a consequence of excess body weight, diabetes mellitus of the first or second type. Often, pathological changes occur in older people without the diseases listed above.
It is believed that alcohol abuse and large amounts of fatty foods in the diet play the greatest role in the development of reactive disorders. Inflammatory pathologies of the gallbladder and liver can also provoke the onset of the disease. This leads to pain and increased blood glucose levels.
Methods for diagnosing pathology in a child
Before making a diagnosis, the doctor finds out the complaints and carefully examines the child. The first symptoms of reactive changes in the liver and pancreas are:
- discomfort or pain in the umbilical region or in the upper abdomen if the head of the pancreas is affected,
- girdling nature of pain when all parts of the gland are involved in the process (body and tail),
- reducing the intensity of pain in a sitting position when bending the torso forward or in a position on the side with legs bent,
- nausea,
- burps of air, flatulence,
- loose stools,
- low-grade fever,
- increased blood sugar,
- dry mouth,
- coating on the tongue.

The clinical picture is not clearly expressed; often not all of the listed symptoms appear, but only individual signs.
In young children, reactive changes in the pancreas often occur without specific symptoms: there is no pain, the condition is not disturbed. If the baby is one year old, the only manifestations of pathology are:
- lethargy,
- decreased appetite,
- bad dream.
Due to the lack of clear symptoms, diagnosis is difficult. In such cases, additional research methods are used.
Functional methods
A diffuse process in the tissues of the gland, its enlargement is detected during ultrasound examination. To verify the diagnosis, sonography of the digestive organs is performed: the liver, gall bladder, and spleen are studied. Defined:
- resizing,
- tissue structure,
- availability of additional education.
The heterogeneous nature of the parenchyma of the digestive organs, combined with the prevailing symptoms, if they occur, will help clarify the underlying diagnosis and associated lesions.
If the ultrasound method turns out to be uninformative and the diagnosis is still doubtful, a computed tomography (CT) scan may be performed. But in children, due to the high dose load, it is rarely performed, in severe, unclear cases.
From functional studies, if necessary, EGDS (esophagofibrogastroduodenoscopy) is prescribed. In addition to the inflammatory process, erosions, ulcers, the study reveals changes in the mucous membrane at the mouth of the sphincter of Oddi - the common duct of the pancreas and gallbladder.
Laboratory diagnostics
Laboratory tests are also required, which include:
- general clinical,
- biochemical blood and urine tests.
Coprogram is prescribed for diarrhea.

How to determine diffuse changes in children
A newborn or toddler will not explain what is bothering him. A child who has reached adolescence can name complaints and characterize his condition: clarify where the stomach hurts, what the nature of the pain is and after what it arose.
To more accurately determine changes in children, the same tests are used that are performed in adults:
- general blood test - reveals the presence of an inflammatory process in the body (leukocytosis and lymphopenia, increased ESR),
- stool analysis - the presence of undigested muscle fibers or starch grains (a characteristic sign of damage to the pancreas),
- elastase-1 in feces is one of the enzymes that indicates organ pathology,
- blood and urine test for amylase levels.
The results indicate the presence of an inflammatory process in the pancreas. Structural changes in the tissue itself can be detected by sonography or CT:
- heterogeneity,
- grain,
- increased level of echogenicity.
Each echo sign indicates diffuse changes. Pancreatitis, which has the same sonographic picture, can be manifested by an increase in size:
- in the presence of characteristic clinical manifestations, this indicates an acute process,
- if the symptoms are not pronounced, but complaints periodically appear, then a moderate increase in the organ characterizes the chronic course of the disease.
Symptoms
Reactive changes in the pancreas in a child or adult patient manifest themselves with symptoms:
- acute pain in the abdominal area, usually above the navel,
- indigestion - diarrhea, flatulence, nausea and vomiting,
- dryness of the oral mucosa, white coating on the tongue,
- fever - usually this symptom appears only in the first hours of illness,
- general malaise, lethargy, irritability.
A characteristic feature of the pain syndrome is that the discomfort decreases or may disappear when the patient is in a sitting position with the torso bent forward.

Abdominal pain often accompanies reactive disorders
In infants, it is very difficult to determine the presence of the disease based on symptoms. The child becomes restless, cries loudly and tries to attract the attention of his parents. A gastrointestinal disorder can be suspected by the fact that all manifestations of the disease usually occur immediately after eating. If the above phenomena occur in a child, it is necessary to consult a doctor as soon as possible.
Healing procedures
If parents notice that the baby is lethargic, refuses to eat, is capricious, or the teenager is losing weight, eating poorly, complaining of nausea and abdominal discomfort, you should immediately contact a specialist.
The doctor will prescribe the necessary treatment after clarifying the diagnosis and rule out diabetes mellitus, which often develops when the pancreas is damaged.
Detected pathological changes in the liver and pancreas tissue must be treated comprehensively. The following therapeutic regimens are used:
- antispasmodic drugs - eliminate pain, relieve spasm of the sphincters of the pancreatic ducts and gallbladder, improving the outflow of digestive juice and bile,
- enzymes to relieve pain and better digestion of food,
- antihistamines, if changes occur as a result of food or drug allergies,
- detoxification measures.

This treatment regimen received positive feedback from specialists and patients.
Mandatory treatment is carried out for the disease, as a result of which the structure of the pancreatic parenchyma has changed. With a peptic ulcer or erosive gastroduodenitis, due to the anatomical proximity of the organs, the head of the pancreas is involved in the pathological process: it begins to enlarge, and pain appears. To avoid complications of the underlying disease and the reactive state of the pancreas, it is recommended to do all prescribed procedures, take medications and follow a diet.
Changes in the gland disappear when the condition of the organ that caused them is normalized. The prognosis is always favorable, since functions are slightly impaired.
Diet in complex therapy of disorders
During the treatment process, you must adhere to the prescribed diet. During the first two to three days, as prescribed by the doctor, any food is prohibited: this creates functional rest for the pancreas. You are allowed to drink alkaline mineral water without gas, weakly brewed tea, compote, jelly. The volume of fluid these days is also determined by the doctor, taking into account the child’s condition.

For the next six days, the diet expands: grated warm food is added in small portions 5-6 times a day.
Prohibited:
- sweets,
- rich meat broths and soups prepared from them,
- canned food,
- fresh fruits and vegetables.
In the future, the list of permitted products increases, but they still need to be thermally processed.