When is it necessary to remove the pancreas?
Life without a pancreas is associated with many difficulties, so the organ is removed only in serious situations, such as:
- Serious injury - if an organ has been wounded or seriously damaged and its restoration and further functioning is impossible.
- Pancreatic cancer
- Pancreatic insufficiency This disease is caused, for example, by alcohol abuse, unhealthy diet, diabetes, stress or the use of a large number of medications.
On this topic
- Oncogastroenterology
Feces for stomach cancer
- Natalya Gennadievna Butsyk
- December 6, 2020
Surgical treatment is sometimes the only chance to save a patient's life. Removing the pancreas is a very complex procedure, often causing complications. The risk is that anatomically this area contains important organs and structures.
Here is the central aorta, which drains blood from most of the intestines, that is, the main artery of the body, which carries blood under high pressure from the heart and back from the whole body. The pancreas also contains blood vessels that supply much of the intestines. Their damage can lead to necrosis of the entire abdominal cavity.
What indications require removal of the pancreas?
If drug treatment and therapy do not help, the doctor is forced to recommend the patient surgery to partially or completely remove the pancreas.
Operation is needed when:
- Presence of a tumor
- fistula,
- false cyst,
- Malignant neoplasms,
- Local organ damage
- Destruction of pancreatic tissue,
- With complications of chronic pancreatitis,
- Some types of pathologies,
- Stones that block the gland channels,
- Pancreatic necrosis, if medications are powerless,
- Peritonitis of the pancreas.
If the gland is not completely removed, the extracted tissue undergoes laboratory testing. They help to formulate the most effective method of treatment and rehabilitation after surgery.
Contraindications
Postoperative mortality and complications after pancreaticoduodenectomy remain a significant problem. According to studies, the mortality rate for this operation is 0.4-16%, and the rate of complications remains high - 11-65%. On this basis, the following risk factors for postoperative complications and mortality can be identified:
- age > 70 years,
- extended resections,
- narrow pancreatic duct
- bile infection.
Nutrition after surgery
After surgery to remove the pancreas, all patients, without exception, are prescribed a strict diet. You will have to stick to it constantly. Remove from the diet once and for all:
- fried and fatty foods;
- smoked meats;
- pickles;
- flour;
- spices;
- canned food;
- semi-finished products;
- sausages;
- spicy dishes and sauces;
- carbonated and alcoholic drinks;
- chocolate;
- cocoa;
- legumes
The patient's daily diet must include lean meat and fish. However, they cannot be consumed together with the skin. He also needs to eat dairy and fermented milk products every day (their fat content should not be more than 2.5%).
You also need to eat food according to certain rules:
- for the first 3–4 months after surgery, it needs to be crushed to a puree-like consistency;
- you need to eat small portions at least 5 times a day;
- 30–40 minutes before meals you need to inject insulin (only if short-acting insulin is used), and while eating you need to take an enzyme preparation;
- food must be warm, hot and cold dishes are prohibited;
- The last meal should be taken 2-3 hours before bedtime.
If you strictly follow the diet and promptly use medications prescribed by your doctor, you can live a long and happy life even after complete removal of the pancreas. If you neglect the doctor’s recommendations, this can lead to serious consequences and significantly reduce your life expectancy.
The pancreas is an organ that is extremely difficult for our body to do without. Its functions are the production of insulin and digestive enzymes. Without insulin, a serious disease develops - diabetes, and without digestive enzymes - intestinal dyspepsia syndrome, in which it is impossible to fully digest food and absorb essential nutrients. Therefore, even partial removal of the gland entails many problems for the patient, not to mention its total resection.
Types of operations
The pancreas is not always completely removed. The type of surgery depends on the severity of the disease and the location of the tumor. Sometimes only a fragment of it is cut out, for example, in the initial stage of malignancy.
In the case of cancer of the head of the pancreas with metastases in the duodenum or part of the bile duct, complete resection is resorted to. The classic operation involves removing the head of the pancreas along with the adjacent segment of the duodenum, the remaining part of the common bile duct along with the gallbladder.
A similar operation is performed for chronic pancreatitis. When diagnosing a pancreatic tumor, it is extremely difficult to rule out cancer before surgery. The final diagnosis is confirmed only by microscopic examination of the excised gland.
If the tumor is localized in the trunk or tail of the organ, the only effective way to combat cancer is resection of the entire pancreas and spleen. It is possible to preserve the spleen, but this is not recommended if the tumor is suspected of being malignant. Both pancreatic cancer and other benign and malignant neoplasms in this area are a serious clinical problem.
Reasons and indications for removing part of the pancreas
Radical treatment methods for severe pancreatic pathology are the last choice in the absence of positive effects from therapy at the previous stages. Any severe disease of the pancreas, if conservative treatment is ineffective, is subject to surgical intervention.
Partial resection is performed in the presence of the following identified indications:
- tumor, fistula, cyst, stone, abscess,
- malignant neoplasms in a certain part of the organ or metastatic damage when the source of cancer is another organ,
- traumatic tissue damage,
- peritonitis, the source of which was inflammation of the pancreas,
- intense bleeding from the vessels of the gland,
- exacerbation of chronic inflammation in the gland.

Surgery is performed if there is:
- complications after cholecystectomy (without bile, deep disturbances in the digestion of food occur, which increases the load on the spleen and requires constant adherence to dietary restrictions; errors in diet cause deep pathology of the pancreas),
- dysfunction or complete cessation of activity of the spleen (necrosis occurs and there is an urgent need to remove the affected pancreas, but even with its absence you can live a long time, leading a full normal life),
- development of tumors: even an ordinary pancreatic cyst under the influence of unfavorable external factors (smoking, alcohol, unhealthy food) can turn into a malignant formation that requires urgent resection,
- entry of a stone from the gallbladder through the common duct into the pancreas during surgery for cholelithiasis (it is impossible to remove a stone from the pancreatic tissue without significant damage to it, usually the pancreatic tissue is not restored, the organ must be resected),
- chronic pancreatitis with frequent severe exacerbations and poor prognosis.
The cost of any elective resection, such as a pancreatic cyst, in hospitals and medical centers varies depending on the geographical location and the qualifications of the operating specialists.
Removal of the head of the pancreas
Statistics show that in 80% of the development of a gland tumor, its head is affected. A pancreaticoduodenal method of surgical intervention is performed, which is called by the author - the Whipple procedure. The operation is carried out in two stages:
- Removal of the affected fragment and part of the neighboring organs involved in the pathological process.
- Subsequent restoration of damaged ducts, gallbladder and patency of the digestive canal.
- impaired absorption of nutrients due to the removal of an important part of the organ that synthesizes digestive enzymes,
- failure in carbohydrate metabolism with subsequent development of diabetes.
The laparoscopic method is used and the operation is performed under general anesthesia.
A laparoscope is inserted through small incisions, the operated area is examined, the feeding vessels and duodenum are blocked and removed, nearby regional lymph nodes are removed, and sometimes it is necessary to partially remove adjacent organs.

After this, a new connection is created between the stomach and small intestine and the body of the pancreas.
The operation is difficult and entails dangerous consequences after removal of the head of the pancreas:
If the head is removed, the following often develop:
- damage to the nerves and vessels adjacent to the gland,
- bleeding,
- infections.
Postoperative pancreatitis with severe secretory insufficiency almost always develops. The recommended treatment regimen must be followed for years. It may consist of lifelong oral replacement therapy plus a special diet for a long period. After surgery, a person becomes disabled.
Operation Beger
Isolated resection of the affected head of the pancreas without removal of the duodenum was developed and introduced by Beger in 1972. During this operation, the stomach and duodenal bulb tightly adjacent to the gland are preserved, which does not interfere with the passage of the food bolus through the digestive canal. The gastropancreatoduodenal discharge of secretions from the gallbladder and pancreas through the small intestine is preserved.
As a result of the research, positive results were obtained in the postoperative period, on the basis of which the method received good feedback from specialists and was widely used. Using this technique, the pancreas is dissected in the area of the isthmus with isolation of the superior mesenteric and portal veins. There is a possibility of bleeding due to existing complications of chronic pancreatitis, in particular, with the development of regional portal hypertension. In these cases, manipulation of the veins is dangerous due to large blood losses.

A duodenum-preserving version of head resection without crossing the pancreas above the portal vein is also used - the Bernese version of the Beger operation.
Tail removal
If the caudal part of the pancreas is affected, a distal pancreatomy is performed. When a tumor arises in the tail and invades the spleen, part or the entire organ is removed. The spleen is resected along with the vessels. In such situations, disturbances in carbohydrate metabolism and the development of diabetes do not occur. The rehabilitation period takes 2–3 weeks.
For a malignant tumor localized in the tail and body of the pancreas, corpocaudal resection of the affected organ is used. This type of surgery is accompanied by splenectomy—removal of the spleen.
Operation Freya
More radical, traumatic and severe surgical interventions include partial resection of the pancreas with complete removal of the head or tail of the pancreas. It is performed rarely and only in severe cases, since its technique is particularly complex and does not always have a favorable prognosis. This is a radical surgical procedure, the indications for which are:
- total and subtotal pancreatic necrosis,
- injuries to a large part of the gland,
- malignant neoplasms with a large volume of organ tissue damage.
The course of the postoperative period depends on the scale of the operation. If tail resection was performed, the prognosis is more favorable, the operation is better tolerated by the patient, and complications do not arise.
Complete resection of the pancreas
Total removal of the gland is rarely performed and in exceptional cases. In case of any, even the most severe pathology, it is preferable to preserve the organ. To achieve this, all possible conservative methods are used:
- therapy using special infusions,
- drug treatment,
- physiotherapy.

Resection is a complex operation: in order to cut out the pancreas, the surgeon must be highly qualified and have extensive experience. This is technically difficult due to the proximity of the aorta, its visceral branches and tightly adjacent adjacent organs, which block surgical access. These include:
- stomach,
- duodenum,
- gallbladder,
- spleen,
- liver.
The operation lasts 6 hours.
Unconditional removal of the pancreas is carried out only in case of its necrosis, when it is necessary to save the patient. This requires strict indications.
Progress of the operation
The operation is performed under general anesthesia. The anesthesiologist informs the patient about the type of anesthesia, its effect and related details. The incision is usually made along the midline of the abdomen, bypassing the navel. The final volume of the part to be removed and the possibility of carrying out the procedure are assessed by the surgeon after opening the abdominal cavity. First of all, it depends on the severity of the disease and the possibility of resection of the change.
On this topic
- Oncogastroenterology
First signs of rectal cancer recurrence
- Natalya Gennadievna Butsyk
- December 3, 2020
In the case of a tumor of the head of the pancreas, it is completely excised along with areas of nearby organs damaged by the tumor. The extent of resection is determined by both anatomy and oncological indications arising from the anatomy of the lymphatic system of this area. In case of resection of the head of the pancreas along with the duodenum and part of the stomach, the next step is to restore the continuity of the gastrointestinal tract.
Sometimes pancreatic cancer is recognized at a late stage of development. In this case, it is often not possible to cut out the tumor. The cause may be infiltration of important vessels, tissues surrounding the pancreas, as well as the presence of distant metastases, indicating a significant degree of disease. It also happens that during the operation a later stage of the disease is recognized than the studies performed before the procedure showed. These patients require surgical treatment first.
In the area of the pancreas there are organs whose patency is of great importance for the future viability of the patient. Consequently, the development of a pancreatic tumor can lead to closure of the intestinal lumen (usually the duodenum) or blockage of the biliary tract.
Indications for surgery
Surgeries on the pancreas are performed according to strict indications, which are determined individually for each patient:
- pancreatitis, turning into pancreatic necrosis;
- abscess or phlegmon of an organ;
- the formation of stones blocking the lumen of the ducts;
- purulent pancreatitis with the development of peritonitis;
- massive injury with unstoppable bleeding;
- malignant tumor;
- multiple cysts causing persistent pain.
These conditions are considered absolute indications for surgical intervention - planned or emergency. Whether surgery is performed for other diseases of the pancreas depends on the characteristics of the pathology and the patient’s health status.
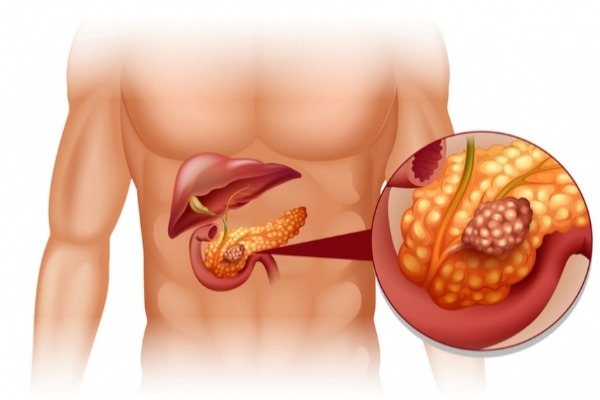
pancreatic cancer
Possible complications
An operation aimed at removing the pancreas is a threat to the health and life of the patient. The occurrence of complications is facilitated by: poor general condition, cachexia, progressive cancer, unsanitary conditions, obesity, diabetes mellitus, additional diseases (heart, liver, lungs).
The anatomy of the abdominal organs is different for each person. Therefore, despite the efforts of doctors during surgical treatment, sometimes technical difficulties arise that can lead to complications.
These include: damage to neighboring organs (for example, the spleen and liver), as well as nerves and blood vessels (the risk of their damage increases with significant obesity, with various anatomical abnormalities in patients who have undergone other operations).
On this topic
- Oncogastroenterology
What kind of pain occurs with rectal cancer?
- Olga Vladimirovna Khazova
- December 3, 2020
Complications of pancreatic resection directly related to the procedure in the early and late period include:
- impaired emptying , leading to nausea and vomiting;
- infection of a postoperative wound due to infection;
- suture rupture as a result of healing complications, impaired blood supply or mechanical stress;
- inflammation of the pancreatic stump;
- inflammation of the bile ducts;
- disruption of blood supply as a result of closure or damage to blood vessels;
- bleeding in the gastrointestinal tract;
- adhesions in the abdominal cavity, which even after many years can lead to intestinal obstruction.
Non-insulin-dependent diabetes mellitus develops when the remnant pancreas is unable to provide enough insulin. This complication is associated with the need to use insulin for the rest of life.
Most of these complications may require subsequent operations, changes in the method of treatment, its prolongation, and can also cause death.
Rehabilitation process after pancreatectomy
Living after removal of the pancreas and spleen, especially at first, is difficult. There is constant pain at the site of scarring of the sutures and a feeling of hunger: in the first few days, eating is prohibited, in the subsequent period you have to follow a strict diet. The doctor will determine how long it will last.

To prevent complications, a course of therapy is carried out:
- antibacterial,
- anti-inflammatory,
- insulin therapy.
A long, sometimes lifelong, course of enzyme preparations is prescribed. The name, dosage and duration of administration are prescribed by the doctor, taking into account the scope of the operation and the patient’s condition. If a resection of the head or tail of the gland is performed, the remaining part will eventually take on some of the functions. With total removal, problems arise with replacement therapy and nutrition.
Mode sequence:
Diet after pancreas removal
After surgery to remove the pancreas, a person lives on a diet for the rest of his life. To exist, you need to make diet a way of life. The essential principles of nutrition are adherence to:
- multiplicity,
- details,
- eating only permitted or permissible food and categorically refusing prohibited foods (you must be able to use a special table indicating calorie content and lists of permitted foods to draw up the correct menu and calculate its calorie value).

After surgery it is important:
Fried, spicy, pickled and salty foods are prohibited.
Rehabilitation period
After the procedure, it is strictly forbidden to eat or drink; you can carefully moisten your lips and tongue with a gauze swab. The ban on food and drink remains in effect until the appropriate diet is introduced by doctors.
Failure to comply with this prohibition can lead to very serious life-threatening complications. The patient receives the required amount of nutrition during the rehabilitation period in the form of droppers. As healing progresses, many foods will be gradually introduced into the diet.
The duration of recovery varies and depends on the patient’s condition before surgery, the course of the operation itself, and concomitant diseases. Pancreatic resection carries a significant risk of complications, which prolongs the patient's hospital stay. If the course of treatment is completed without complications, the patient is allowed to go home after 10 days. By this time, the drainage tubes had been removed, normal nutrition was turned on, and the patient was already able to walk independently.
Postoperative care for patients in a hospital setting
In the postoperative period, the condition may worsen due to sudden complications. The most common of these is acute pancreatitis, especially if the surgical intervention extended to the duodenum (duodenum), stomach, or ducts of the gallbladder and pancreas. It occurs as pancreatic necrosis: the patient begins to have severe abdominal pain, fever, vomiting, and leukocytosis in the blood, increased ESR, high levels of amylase and sugar. These signs are a consequence of the removal of part of the pancreas or nearby organs. They indicate that a purulent process has developed, and a stone or blood clot may also pass away.

In addition to acute pancreatitis, there is a risk of other postoperative complications. These include:
- bleeding,
- peritonitis,
- hepatic-renal failure,
- pancreatic necrosis,
- diabetes.
Given the high probability of their development, immediately after the operation the patient is admitted to the intensive care unit. He is under observation throughout the day. Important vital signs are monitored: blood pressure, ECG, pulse rate, body temperature, hemodynamics, blood sugar, hematocrit, urine values.
During his stay in the intensive care unit, the patient is prescribed diet No. 0 - complete starvation. Only drinking is allowed - up to 2 liters in the form of still mineral alkaline water, rosehip decoction, weakly brewed tea, compote. The doctor calculates how much fluid you need to drink. Replenishment of necessary proteins, fats and carbohydrates is carried out through parenteral administration of special protein, glucose-salt lipid solutions. The required volume and composition are also calculated by the doctor individually for each patient.
If the condition is stable, the patient is transferred to the surgical department after 24 hours. There, further treatment and care are carried out, and dietary nutrition is prescribed from the third day. Complex therapy, including special nutrition, is also prescribed individually, taking into account the operation performed, condition, and the presence of complications.
The patient remains in the hospital for a long time. The length of stay depends on the pathology and the extent of the surgical intervention. At least 2 months are necessary to restore digestion. During this period, the diet is adjusted, blood sugar and enzymes are controlled and brought back to normal. Since enzyme deficiency and hyperglycemia may occur after surgery, enzyme replacement therapy and glucose-lowering drugs are prescribed. Post-operative care is just as important as a successful surgery. How a person will live and feel in the future largely depends on it.

The patient is discharged in stable condition with an open sick leave for further outpatient treatment. By this time, his digestive system had adapted to the new condition and its functioning was restored. The recommendations indicate in detail the necessary rehabilitation measures, drug treatment, and diet. It is discussed with the patient what regimen he should follow, what to eat in order to avoid relapse.
Consequences of the operation
Modern medicine has made great strides in the field of surgery. Most operations are successful and patients recover quickly. But, unfortunately, there are also unpleasant consequences of chronic pancreatitis due to the fault of the patient, medical personnel or circumstances beyond anyone’s control:
- Anemia associated with large blood loss during surgery. This happens if large vessels were accidentally hit during surgery or the patient has a blood clotting disorder. To prevent this phenomenon, before surgery, blood is always taken for a coagulogram and, if necessary, special drugs are administered to improve coagulation. In the event that blood loss does occur, the person is given an infusion of blood or its components.
- Suture decay. It often happens in patients with diabetes mellitus, as well as in cases of dressing violations and non-compliance with hygiene rules. In case of suppuration, the wound is washed, the pus is removed and, if necessary, drainage is installed.
- Postoperative bleeding. Occurs due to poor-quality suturing, blood clotting disorders, patient violation of the hospital regime, infection, diabetes mellitus. As a rule, they occur in the first days after surgery, when the patient is still in the hospital. Treatment is carried out surgically.
- Postoperative shock. Very often it occurs after surgery, when anesthesia or anesthesia stops working. The patient begins to feel severe pain, blood pressure may rise, or breathing may stop. In order to prevent these harmful consequences, the first day after the operation the person is in intensive care under the constant supervision of doctors. The patient is given painkillers upon request and, if necessary, is connected to a ventilator or given an oxygen cushion.
- Infection during surgery. Today, this happens extremely rarely when an infection enters the surgical field during surgery. In order to avoid this, all instruments are sterilized in an autoclave, the air is purified with ultraviolet light and ionized, and the materials used are disposable and sterile.
Attention! If infection does occur, the patient's temperature rises and pain occurs. If assistance is provided in a timely manner, harmful consequences can be avoided, but if you do not pay attention to the symptoms, the complication can develop into peritonitis and even sepsis.
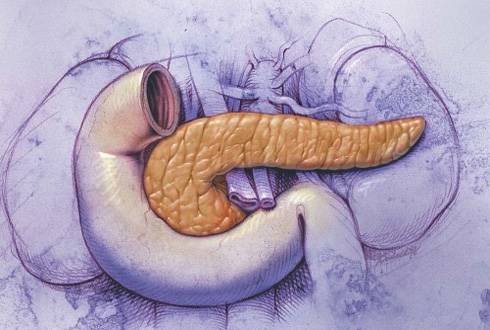
Carrying out the operation
Considering that the pancreas is surrounded by such important formations for the body as the celiac and superior mesenteric arteries, the abdominal aorta, the hilum of the spleen, the inferior vena cava and the common bile duct, and its weight is only 65-80 grams, it becomes obvious that the performance of pancreatectomy is characterized by high level of complexity and requires special skills and skill from the surgeon.
During the operation, general anesthesia is used, an injection of which is injected into the arm intravenously and blocks pain, keeping the patient asleep. The surgeon, making an incision in the abdominal cavity, removes the affected gland, as well as, if necessary, other nearby organs. At the end of the procedure, the doctor closes the incision with staples or stitches.
During the operation, a drainage may be placed in the abdominal cavity, through which the accumulated fluid will be drained out. If necessary, an additional tube can be removed from the intestine for enteral nutrition.
In cases where it is necessary to remove only part of the pancreas, the surgeon performs the operation using laparoscopy. This method involves the use of a laparoscope - an instrument with a camera and a light source - and miniature surgical instruments, with which the doctor performs a partial pancreatectomy through small holes.
At the end of the operation, which lasts 5-8 hours depending on the size of the pancreas being removed, the breathing tube can be removed and the patient can be sent to the recovery room.
Enzyme replacement therapy
After removal of the pancreas, the patient is prescribed complex enzyme and insulin therapy. The main goal of enzyme therapy is to stimulate the production of enzymes involved in the process of digestion of food taken. Prescribed drugs that include pancreatin. Most often prescribed are Micrazim, Vestal, Creon. These enzymatic preparations normalize digestion, intestinal function and stool, eliminate bloating, nausea and stomach discomfort. Enzymatic agents practically do not cause a negative reaction in the body. They replace the work of the pancreas, releasing amylase and lipase into the digestive tract. Enzymes should be taken with each meal in individually selected doses.
We recommend watching a video about the pancreas
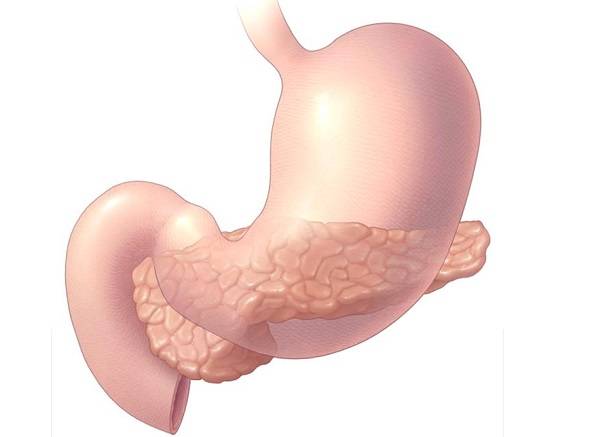
The pancreas is one of the most important parts of the human body. It is presented in a single copy and is an indispensable component of the body. It is located slightly below the stomach, in the “horseshoe” of the duodenum. Performs the following essential functions:
Secretion of digestive enzymes (lipase, trypsin, chymotrypsin, amylase, nuclease and others). The organ is the main “workshop” for the production of substances for digesting food. Without it, a person could not live, since proteins, fats and carbohydrates were simply not absorbed. Secretion of insulin and glucagon - hormones that respectively reduce and increase the amount of sugar in the blood. For this purpose, there are special endocrine B cells, which are grouped into islets of Langerhans. They ensure normal glucose levels in healthy people. If you cut out the gland, then type 1 diabetes will 100% form.
Possible consequences in the postoperative period after removal of the pancreas
Big problems arise if the gland is completely removed. The enzymes produced by the pancreas must be supplemented with medical preparations, which include substances obtained from the pancreas of cattle.
To maintain insulin levels, the patient is prescribed injections of artificial insulin. Some negative reactions are possible after anesthesia. The patient may complain of dizziness and nausea. A dangerous complication is internal bleeding. It is also possible that serious disorders in the body will develop.
Functions of the organ
The pancreas plays an important role in ensuring normal human life. Among the functions it performs are the secretion of digestive enzymes and the synthesis of hormones, including glucagon and insulin, the deficiency of which leads to the development of diabetes mellitus. In this regard, many people today are concerned about whether it is safe to remove the pancreas, and whether it is possible to live a full life after such an operation?
Indications for removal
An operation during which the pancreas or part of it is removed is called pancreatectomy.
As a rule, only inflammation of this organ can be treated without surgery. A direct indication for performing an operation on it in order to improve the patient’s condition or completely cure it is the presence of diseases such as:
false cyst; chronic inflammation; benign or malignant tumor.
In some cases, it is necessary to remove not only the pancreas, but also nearby organs, including:
gallbladder; spleen; part of the stomach or small intestine; The lymph nodes.
Removing parts
Statistics show that 80% of pancreatic cancer is localized in the area of its head. If the tumor can be removed, surgery is performed to remove the head. Surgery always has serious consequences, even when not the entire organ is removed. After pathology is detected in the head area, it is also removed, and if the spleen is affected, the tail and spleen are removed as a single complex.
The prognosis after surgery in the head or tail area is favorable. After surgery, special nutrition will also be required, especially in the first period after surgery.
Carrying out the operation
Considering that the pancreas is surrounded by such important formations for the body as the celiac and superior mesenteric arteries, the abdominal aorta, the hilum of the spleen, the inferior vena cava and the common bile duct, and its weight is only 65-80 grams, it becomes obvious that the performance of pancreatectomy is characterized by high level of complexity and requires special skills and skill from the surgeon.
During the operation, general anesthesia is used, an injection of which is injected into the arm intravenously and blocks pain, keeping the patient asleep. The surgeon, making an incision in the abdominal cavity, removes the affected gland, as well as, if necessary, other nearby organs. At the end of the procedure, the doctor closes the incision with staples or stitches.
During the operation, a drainage may be placed in the abdominal cavity, through which the accumulated fluid will be drained out. If necessary, an additional tube can be removed from the intestine for enteral nutrition.
In cases where it is necessary to remove only part of the pancreas, the surgeon performs the operation using laparoscopy. This method involves the use of a laparoscope - an instrument with a camera and a light source - and miniature surgical instruments, with which the doctor performs a partial pancreatectomy through small holes.
At the end of the operation, which lasts 5-8 hours depending on the size of the pancreas being removed, the breathing tube can be removed and the patient can be sent to the recovery room.
Indications for removal
An operation during which the pancreas or part of it is removed is called pancreatectomy.
As a rule, only inflammation of this organ can be treated without surgery. A direct indication for performing an operation on it in order to improve the patient’s condition or completely cure it is the presence of diseases such as:
false cyst; chronic inflammation; benign or malignant tumor.
In some cases, it is necessary to remove not only the pancreas, but also nearby organs, including:
gallbladder; spleen; part of the stomach or small intestine; The lymph nodes.











