Many women try to endure the painful symptoms of hemorrhoids (pain in the anus, burning, itching) for a long time because of shyness and the belief that “it will go away on its own.” They do not think that hemorrhoids are dangerous not only as a disease, but also because of their consequences.
If treatment is delayed, you will still have to see a doctor, but with complications that are much more difficult to eliminate.
Three serious dangers of hemorrhoids
If you do not pay attention to the signs of pathology, this can lead to the progression of hemorrhoids.
There are a number of extremely dangerous consequences of hemorrhoids:
First. Swollen nodes are vulnerable and easily injured, which is fraught with the occurrence of systematic hemorrhages.
As the disease progresses, these hemorrhages can become more intense and lead to massive blood loss, after which it will take a long time to recover under the supervision of doctors.
Also, systematic bleeding leads to the development of anemia, which is accompanied by a number of dangerous symptoms: weakness, headaches, disruptions in the functioning of the heart, and breathing problems.
Second. If hemorrhoids are left untreated, their continued progression will lead to the formation of blood clots in the hemorrhoids.
Over time, the clot separates from the walls and travels throughout the body with the bloodstream. If it blocks the lumen of one of the key vessels in the body, this will lead to the development of a blood flow disorder.
Depending on the location of the thromboembolus, this consequence can lead to stroke, thromboembolism of the pulmonary, renal, and mesenteric vessels.
Third. The symptoms of hemorrhoids are easily confused with signs of other dangerous diseases: traumatic injuries, hemorrhages in the rectum, necrosis and cancer.
In order to identify these pathologies in time, you should undergo regular examinations with a proctologist and not treat yourself.
In order to identify these pathologies in time, you should undergo regular examinations with a proctologist and not treat yourself.

Hemorrhoid thrombosis
The symptoms of hemorrhoids can easily be confused with signs of other dangerous diseases:
- Traumatic injuries;
- Hemorrhages in the rectum;
- Necrosis and cancer.
Each of these consequences is scary in that it can result in death, and in order to prevent this, you need to consult a doctor at the first signs of pathology, undergo diagnosis and treatment. Hemorrhoids in the early stages can be successfully treated conservatively.
Primary signs of hemorrhoids and the need for timely treatment
The primary signs of hemorrhoids are the formation of some discomfort that occurs in the initial stages of the disease. At first, these sensations are intermittent and accompanied by slight unpleasant sensations. However, ignoring this condition and neglecting the disease can lead to its spread. This fact, in turn, has much more pronounced consequences. That is why the primary symptoms of the disease require close attention followed by a timely response.

Excessive straining, which is a consequence of constipation, leads to injury to the tissues that form the anus. As a result of this process, the primary symptoms of the development of the disease are formed, which look like this:
- discomfort;
- burning or tingling sensations;
- minor bleeding;
- swelling;
- mucus secretion;
- unpleasant smell.
All these factors represent only the primary signs of the development of hemorrhoids and best characterize the degree of its progression. As a rule, the initial stages of the disease, caused by minor trauma to the anus, carry only minor consequences. Ignoring these signs may contribute to the further development of the disease.
Its transition to more complex stages is fraught with the occurrence of quite pronounced symptoms that have a serious impact on the woman’s body. That is why timely taking action and seeking medical help is a key factor in quickly and effectively neutralizing the disease, as well as ensuring a person’s full recovery.

Causes
Hemorrhoids develop when there is insufficient blood supply to the anorectal area.
The following factors predispose to this:
- Constipation.
Toxic substances retained due to constipation negatively affect the rectum. Also, feces increase pressure, because of this, excess blood flows to the anorectal area and overloads the hemorrhoids, which gradually increase in size. - Pregnancy.
The fetus, especially in the second and third trimester, puts intense pressure on the abdominal organs, which leads to the development of hemorrhoids. The process of childbirth also aggravates the condition of hemorrhoids. To reduce the discomfort and severity of hemorrhoids during pregnancy, you should perform special exercises. - Spicy food.
Regular consumption of spicy foods over time leads to irritation in the anal area. - Heredity.
The likelihood of getting hemorrhoids increases if your immediate family has had this disease. - Sedentary work
leads to stagnation of blood in the anal area and poor circulation. - Excessive alcohol consumption
: it accelerates blood flow in the anorectal area, which affects the occurrence of bleeding. - Excessive physical activity.
Regular lifting of heavy objects overloads the ligamentous apparatus. Some sports are also fraught with the development of hemorrhoids: cycling, weightlifting, horse riding. - Liver diseases.
The vessels that are located in the intestinal structure are connected to the liver, and diseases that affect it increase intravascular pressure. - Neoplasms in the intestines.
These include both benign and malignant tumor formations. They increase pressure and load the nodes, increasing the likelihood of regular constipation and obstruction. - Infection.
If pathogenic microorganisms penetrate microcracks (during anal sex or for other reasons), this causes irritation of the anorectal area, which affects the development of pathology.
These reasons do not always lead to hemorrhoids, but a combination of several factors increases the likelihood.
Men develop hemorrhoids four times more often than women.
The development of hemorrhoids and factors contributing to its appearance
Hemorrhoids are a fairly specific disease, accompanied by the development of an inflammatory process in the anal area. It equally affects both the male half of the population of our planet and its female part. Moreover, it is for a woman that it can have the most devastating consequences, which can significantly complicate her life and affect her overall health. This disease has many negative manifestations that can significantly complicate a person’s life and cause him some discomfort.
As a result of certain factors, peculiar plaques form in the anus, contributing to the occurrence of the inflammatory process. There can be many reasons for the appearance of the disease.
However, the following factors have the greatest impact on a person:
- genetic predisposition;
- various diets;
- sedentary lifestyle;
- sedentary work;
- state of stress;
- excess body weight.
Any of the above factors can serve as a catalyst for the formation of the disease. The combination of several of them significantly accelerates the process of hemorrhoids and contributes to its spread.
Kinds
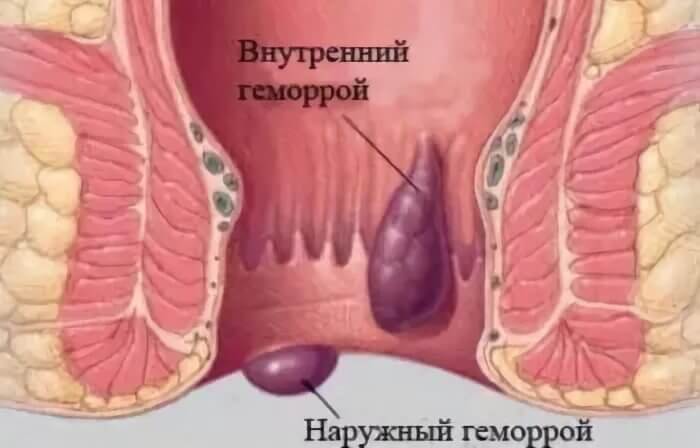
Based on the location of the swollen hemorrhoid, hemorrhoids are divided into:
- Internal hemorrhoids are a node located under the intestinal mucosa, the course of the disease is mild, in some cases hidden, painless. Because of this, diagnosis is difficult.
- External hemorrhoids are fraught with rapid development of symptoms and rarely occur hidden. The nodes are located under the surface of the skin of the anal area.
Accompanied by the following symptoms:
- Pain in the anorectal area.
In the first stages it is absent or weakly expressed, appears during defecation, and practically does not occur during the rest of the period. As the disease progresses, pain worsens and is observed not only during bowel movements, but also during movements (walking, running), and in a sitting position. - Discomfort
in the anus and in the rectal area, which is manifested by false urges and a feeling of fullness with feces. Also, the resulting hemorrhoids make defecation difficult and increase the frequency of constipation. - Burning.
The disease is manifested by the development of inflammation in the area of the intestinal mucosa, which is accompanied by the appearance of mucous secretions, and they, seeping into the anus, cause intense irritation. - Bleeding.
They are observed mainly during defecation due to the fact that feces touch the inflamed node and injure it. In the early stages, it appears as small specks of blood left on a piece of toilet paper and may be absent. But hemorrhoids are scary because as they progress, the intensity of hemorrhages increases, up to severe, life-threatening blood loss. - Knot loss.
The node falls into the lumen during defecation. If the disease is in the early stages, it is set on its own; at later stages, it has to be set with the fingers, and at the last stage it is impossible to return it to its place.

Consequences of the disease
Important:
There is also combined hemorrhoids, in which both internal and external nodes are present.
According to the nature of the flow, they are distinguished:
- Acute hemorrhoids
- Chronic hemorrhoids
Acute hemorrhoids are usually an exacerbation of the chronic form, and after its completion the disease is practically asymptomatic.
Accompanied by:
- Acute pain that is constantly present and intensifies with straining;
- Cyanosis and swelling of the node;
- Hyperthermia due to an infectious lesion.
Symptoms of acute hemorrhoids
The first manifestations of acute hemorrhoids are:
- sharp increasing pain;
- bleeding;
- prolapse of dense, sharply painful nodes from the anal canal.
Pain in the anus may occur during or after bowel movements. Pain syndrome in OH can be either mild, causing only discomfort, or unbearable, constant, unabating, debilitating and significantly reducing the quality of life. With such intense pain, it is impossible to sit, stand or walk, the patient is restless and agitated due to the pain syndrome. It is difficult to find a body position in which the pain would subside even a little.
Bleeding most often occurs during the act of defecation, due to the rupture of the node at the moment of tension and the passage of feces. There were cases when bleeding reached 100-150 ml.
When a thrombosed node prolapses, attention is drawn to the presence of a sharply painful dense formation in the anus. The slightest touch to the knot causes a severe attack of pain, which causes restrictions in body position. If a thrombosed internal hemorrhoid has fallen out, is not strangulated, it is possible to move it back into the anal canal either independently or with the help of a manual aid, but this also only increases the pain.
Stages
Hemorrhoids in themselves do not pose a serious danger, but the complications that they cause as they progress if untreated are fraught with significant risks to life, health and physical comfort. The danger of this pathology increases as you move from stage to stage.
| Stage name | Description |
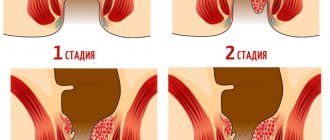
| First stage | Pain is absent or moderate, the disease does not create significant discomfort. There may be minor hemorrhages that are not accompanied by pain. |
| Second stage | The nodes may fall into the lumen when straining, but return to their place on their own. There is discomfort, hemorrhages become frequent, mucous discharge occurs, which causes burning and itching. |
| Third stage | Knots fall out when running, lifting weights, doing gymnastics, or during straining, and they no longer return to their place on their own. They need to be adjusted with your fingers every time this happens, and over time they begin to fall out even with coughing and sneezing. |
| Fourth stage | This stage of the disease is the most dangerous: there is a high probability of thrombosis, which is fraught with thromboembolism and necrosis. Bleeding is intense and regular, anemia develops. It is no longer possible to set the fallen nodes; surgical intervention is required. |
Complications in women
There are the following consequences of hemorrhoids, in addition to thrombosis and anemia:
- Ulcerative colitis.
If the inflammatory process rises higher, this leads to the occurrence of ulcers. Hemorrhoidal colitis can lead to peritonitis if perforation of the ulcer develops. - Infringement of the node.
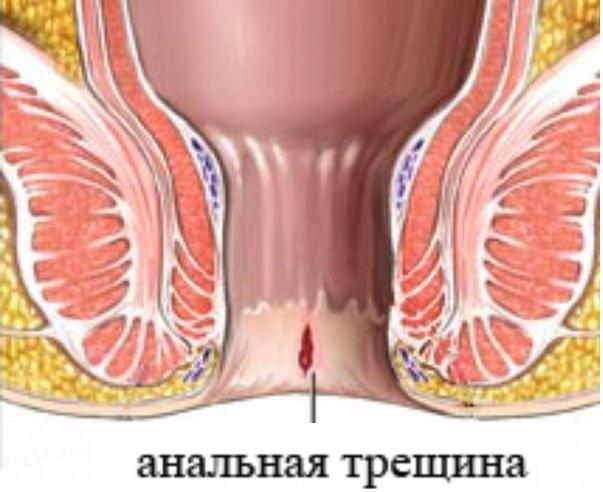
If the protruding node becomes pinched by the muscular system of the anal zone, without medical treatment this will quickly lead to necrotic changes: gangrene of the rectum will develop. - Anal fissures.
This complication is one of the most common and is accompanied by severe pain. - Malignant neoplasms.
Neglected hemorrhoids are dangerous because they lead to cancer due to constant inflammatory processes and hemorrhages. - Dermatitis.
Mucous discharge irritates the skin around the anus; due to itching, this area is actively scratched, which leads to the development of skin inflammation. In women, if the infection affects the genitals, the disease will lead to colpitis.
Side effect of constipation.
Complications in men
Like women, men can experience malignant neoplasms, colitis, and anal fissures. There are also other complications:
- Fournier's gangrene.
It affects men, develops rapidly, and death is observed in 30-90% of cases depending on the affected area (if the disease develops in the testicles, mortality is higher). - Cryptit.
Feces remain in the recesses in the anal area, and over time this becomes the cause of inflammation and other complications.
Not treating hemorrhoids or treating yourself is dangerous - you can start the disease. In the early stages of the disease, the risks of complications are minimal, but gradually inflammatory processes become more pronounced.
Hemorrhoids during pregnancy
Pregnancy is one of the key factors that lead to the development of hemorrhoids. The disease creates problems during pregnancy due to bleeding, anemia and requires urgent initiation of therapeutic measures.
There are recommendations that can reduce the risk of developing hemorrhoids during pregnancy:
- A woman’s diet should contain a sufficient amount of fiber (cereals, vegetables, herbs);
- You should reduce your consumption of meat products and coffee, use seasonings in moderation;
- Regularly wash the anal area after defecation.
Hemorrhoids - manifestations and possible complications
Hemorrhoids translated from Greek mean bleeding (hema - blood, rheo - flow). In the modern understanding, hemorrhoids are an increase in the volume or expansion of the cavernous bodies of the rectum.
Typical symptoms of hemorrhoids are bleeding from the anus and prolapse of hemorrhoids. It should be remembered that the discharge of blood from the anus may be a manifestation of another pathology of the colon, primarily malignant neoplasms and nonspecific inflammatory diseases of the colon. With stage I-II hemorrhoids, when hemorrhoids do not prolapse or prolapse only during bowel movements, bleeding is usually also observed during bowel movements. The blood that comes out is scarlet. If a patient says that he finds drops of blood in the toilet, we are most likely talking about hemorrhoids. If he notes that blood is mixed with feces, one should think about other diseases of the colon. With stage III-IV hemorrhoids, patients notice drops of blood on their underwear.
If dark blood is released during bowel movements, a tumor of the colon should be ruled out first.
Other manifestations of hemorrhoids include unpleasant sensations (discomfort), itching and pain in the anus, discharge from the anus, and a feeling of irritation. Pain is usually observed with thrombosis of hemorrhoids or concomitant anal fissure. Complications of hemorrhoids include thrombosis of hemorrhoids, as well as the formation of perianal fimbria.
To diagnose hemorrhoids, a digital examination of the rectum is performed, as well as rectoscopy. All patients in whom the source of bleeding remains unclear after these studies undergo irrigoscopy or colonoscopy.
Acute hemorrhoids are a common disease. The reasons for visiting a doctor are usually bleeding, severe pain and the inability to reduce prolapsed hemorrhoids, thrombosis of external or internal hemorrhoids. Thrombosis may be the first manifestation of the disease or occur against the background of other symptoms. Some authors consider thrombosis of hemorrhoids to be acute hemorrhoids. Patients with this pathology require emergency medical care. In acute hemorrhoids, a significant dilation of the rectal venous plexuses occurs, leading to inflammation and ulceration of the mucosa, which is accompanied by an increase in the level of prostaglandin E2. As already noted, acute hemorrhoids are provoked by a number of mechanical and hemodynamic factors. For example, the opening of arteriovenous shunts is facilitated by the intake of hot and spicy foods, alcoholic beverages, as well as constipation, straining during bowel movements and childbirth.
There are three degrees of severity of acute hemorrhoids.
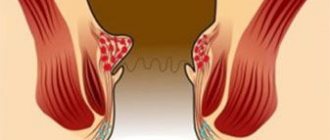
In grade I, external hemorrhoids are small in size, have a tight-elastic consistency, and are located below the dentate line. They are painful on palpation. The perianal skin is slightly hyperemic. Typical complaints are a burning sensation and itching, aggravated by defecation.
In grade II, more pronounced swelling of most of the perianal area and hyperemia are observed. Palpation of this area and digital examination of the rectum are sharp and painful. Patients complain of severe pain in the anus, especially when walking and sitting.
In grade III, the entire circumference of the anus is occupied by an “inflammatory tumor.” Palpation of the nodes is very painful. In the area of the anus, purple or bluish-purple internal hemorrhoids covered with fibrin films are visible. In the absence of modern treatment, node necrosis may occur. The mucous membrane covering them becomes ulcerated, and black areas with a coating of fibrin appear. In advanced cases, paraproctitis (severe purulent complication) may develop.
Chronic hemorrhoids.
The most common clinical course of hemorrhoids is a chronic recurrent process. The disease begins with a period of precursors, when the patient notices unpleasant sensations in the anus: a feeling of discomfort, a sensation of a foreign body, mild itching, increased humidity.
Then rectal bleeding appears - the release of drops or streams of scarlet blood at the end of a bowel movement. This period, which lasts from several months to several years, is characterized by long phases of remission, when there are no complaints. For this reason, in the initial stage of chronic hemorrhoids, patients rarely consult a doctor.
Gradually the disease progresses. When defecating, pain appears in the anus, which intensifies when the diet is disrupted. Bleeding from the anus during defecation becomes constant, and its intensity can vary - from blood stains to massive blood loss, leading to anemia. The gradual enlargement of internal hemorrhoids leads to their prolapse from the anus.
Depending on the degree of enlargement of hemorrhoids and the development of the dystrophic process in the fibromuscular framework holding them, four stages of chronic hemorrhoids are distinguished:
- the first stage is characterized by bleeding from the anal canal without prolapse of hemorrhoids;
- in the second stage, hemorrhoids fall out during defecation, and after it is completed they are reduced on their own;
- the third stage is characterized by the fact that the nodes that fall out during defecation have to be set by hand;
- at the fourth stage of development of hemorrhoids, the nodes fall out when sneezing, coughing, or the slightest physical activity. It is not possible to push them into the anal canal.
Complications of hemorrhoids.
Thrombosis of hemorrhoids usually occurs when straining during bowel movements due to swelling of the prolapsed nodes. Spasm of the rectal sphincter increases swelling, leads to stagnation of blood in the lower rectal plexus and thrombosis of external hemorrhoids. The patient complains of pain, swelling, discharge from the rectum with an unpleasant odor and difficulty defecating. Upon examination, prolapsed, edematous, irreducible internal hemorrhoids are identified, often with fibrinous plaque. Thrombosis of hemorrhoids is an indication for the use of local anticoagulants. This group of drugs includes heparin and troxevasin ointments, ambenate, hepatrombin G and other drugs. In 70-80% of cases, thrombosis of hemorrhoids is complicated by their inflammation with transition to the subcutaneous tissue and perianal area. In this case, these drugs are used in combination with water-soluble ointments that have a pronounced anti-inflammatory effect. These include Levasin, Levomekol, Oflocaine and others.
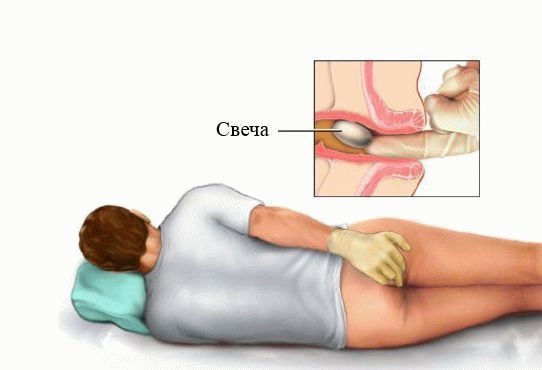
In acute hemorrhoids and in the early stages of chronic hemorrhoids, conservative treatment is carried out. Its main goal is to relieve pain and inflammation, normalize blood circulation in the rectal area, and regulate digestion. Conservative treatment is common: tablets that increase the tone of the veins, improving blood flow through small vessels and cavernous veins; and local: wound healing, analgesic and antipruritic ointments, suppositories, microenemas and baths. At the same time, an anti-hemorrhoids diet is prescribed: vegetables, fruits, bran, but you will have to forget about spices, spicy foods and alcohol.
Under local anesthesia, the prolapsed nodes are reduced, and then ligation of internal nodes with latex rings and thrombectomy from radial incisions are performed with concomitant acute thrombosis of external hemorrhoids. The intervention is performed on an outpatient basis. The immediate and long-term results are good. In case of thrombosis complicating stage IV hemorrhoids, emergency hemorrhoidectomy is indicated.
Bleeding is one of the main symptoms of hemorrhoids. Continuous bleeding for 1 hour is a sign of an acute process. To eliminate it, you can use suppositories containing adrenaline. In addition, local hemostatic materials such as adroxon, beriplast, tachycomb, spongostan, consisting of fibrinogen and thrombin, are used. When introduced into the anal canal, they dissolve, forming a fibrin film. A number of authors (M.A. Kamalov, 1988; A.M. Koplatadze et al., 1989; V.V. Stavitsky et al., 1993; K. Eu et al., 1994) for acute hemorrhoids recommend surgical intervention in volume of hemorrhoidectomy.
Paraproctitis is a purulent inflammation of the tissues surrounding the rectum.
There are acute (newly occurring) and chronic paraproctitis (develops as a result of untreated acute paraproctitis).
The causes of acute paraproctitis can be non-compliance with personal hygiene rules, traumatic manipulations in the anal canal area, the presence of anal diseases (anal fissures, hemorrhoids).
Through special glands located in the anus, the infection from the lumen of the rectum penetrates into the surrounding tissues. Inflammation develops and an abscess forms.
Depending on a person’s immunity, the size and location of the abscess may vary. The abscess can be located either directly under the skin of the perineum or deep between the muscles of the perineum and buttocks.
The disease begins suddenly. Weakness, malaise, fever and chills, pain in the rectum and perineum appear.
In the area of the anus there is noticeable limited redness, swelling and pain when palpated.
In the absence of treatment, the temperature rises over several days, the pain intensifies, and stool and urine retention are noted.
When the first signs of disease or discomfort in the anus appear, you should urgently consult a surgeon or proctologist.
Diagnostics.
The disease is detected by examination and digital examination of the rectum.
To exclude complications of acute paraproctitis, women also need to consult a gynecologist, and men - a urologist.
Treatment
Treatment of acute paraproctitis is only surgical. Surgery should be performed immediately after diagnosis. The operation is performed under anesthesia.
The purpose of the operation is to open the abscess (abscess) and remove the pus. After the operation, dressings are performed, antibiotics, vitamins, and immune boosters are prescribed. This operation can be performed in any surgical hospital.
However, opening the abscess is not a radical operation: after it, as a rule, repeated suppurations occur (chronic paraproctitis is formed). The reason for this phenomenon is the preservation of the inflammatory channel (fistula) between the rectum and surrounding tissues.
For a complete cure, a repeat operation is required, performed in a specialized proctology hospital. As a result of such an operation, the connection between the intestinal cavity and the abscess is eliminated. It is called radical because leads to complete recovery.
Performing a radical operation immediately after a diagnosis of acute paraproctitis is often not successful, since there is a high probability of injury to the anus and the development of fecal incontinence. However, radical surgery performed after the abscess has healed provides a complete cure of the disease.
With untimely surgical treatment of acute paraproctitis, complications may develop: purulent destruction of the wall of the rectum and/or the wall of the urethra in men, breakthrough of pus into the vagina in women. The most serious complication is the breakthrough of pus into the pelvic cavity, which can be fatal if diagnosed late.
Rybalko S.A. surgeon
How to treat hemorrhoids?
The following medications are used in the treatment of hemorrhoids:
- Anti-inflammatory ointments, gels to eliminate swelling, burning and pain;
- Phlebotonics improve the tone of vascular walls and have a positive effect on blood circulation;
- Anti-inflammatory medications in the form of suppositories, tablets (steroids can also be used);
- Painkillers to relieve pain;
- Antiseptic medications (suppositories, ointments) reduce the risk of infection;
- When thrombosis develops, thrombolytics are used to dissolve blood clots.
Treatment at home
Important:
If conservative methods have not shown sufficient effectiveness or the disease is at the last stage, surgical intervention is indicated.
The attending physician will answer how many days of sick leave are required for hemorrhoids, depending on the individual situation. On average, sick leave is given for a week.
Treatment of advanced hemorrhoids is difficult, and surgical intervention is not always able to completely eliminate all problems and is fraught with complications, so you should go to the hospital as early as possible.
Living with hemorrhoids requires following medical recommendations, giving up bad habits, and correcting your diet. Once the condition is resolved, it is important to continue to eat healthy and come in for regular checkups.