What is the pancreas
The pancreas is an organ of the digestive system that performs external and internal functions. The essence of external secretion is the secretion of pancreatic juice. It contains all the necessary digestive enzymes, which ensure the normal functioning of the digestive tract. The external function is the production of hormones and the normalization of metabolic processes: protein, carbohydrate and fat.
What can trigger the disease?
There are a large number of reasons that can provoke pancreatic disease. The main factors include the following:
- pathologies of the duodenum and biliary tract;
- congenital abnormalities;
- infection;
- severe stress;
- poor nutrition;
- problems with the outflow of secretions due to the tumor process;
- gland injury.
The following congenital anomalies of the pancreas may be observed:
- hypoplasia;
- inflection;
- incorrect structure of the ducts.
The development of the disease is influenced by the age, gender of the patient, as well as his lifestyle and the environmental situation in which he lives.
What do parents need to know?

In addition to following the rules for preparing and eating food for children with pancreatitis, there are some other nuances that parents should know in order to prevent accidental errors in the baby’s diet:
- Children of preschool age attend preschool institutions. In kindergartens, although exclusively dietary food is prepared, this food is not suitable for children with pancreatitis. Therefore, the mother should warn the teacher that the child has some dietary restrictions. You also need to give the baby’s medical record with the recommendations indicated in it to the nurse of the preschool institution.
- Sometimes, when children follow a gentle diet, a situation arises when children are invited to a birthday or holiday. It is under no circumstances recommended to skip such an event due to dietary restrictions, as this will negatively affect the social adaptation of a small child. In this case, in order to avoid dietary or psychological problems, you need to talk in advance with the parents of the inviting child about the diet prescribed by the doctor.
But gastroenterologists also recommend that mothers remember that new foods should be introduced into the diet of babies suffering from pancreatic problems with extreme caution. The initial portions are made tiny, not exceeding 5–10 grams, and if negative symptoms appear, they are immediately removed from the diet. But after some time, they try to introduce the removed product into the menu again. It is excluded completely only when the baby’s body shows a negative reaction for the second time.
Bibliography
- Baranov A.A. Problems of pediatric enterology at the present stage. Russian Gastroenterological Journal 1995 No. 1 pp. 7–11.
- Baranov A.A., Klimanskaya E.V., Rimarchuk G.V. Pediatric gastroenterology. M., 2002
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. In the book “Handbook of Dietetics”, edited by V.A. Tutelyan, M.A. Samsonova. - 3rd ed., M.; Medicine. 2002 pp. 209–217.
- Plotnikova T.V. Recipes of dishes for children's institutions. Phoenix 2013
- Ilyin V.F., Therapeutic diets for pancreatitis and other diseases of the pancreas. M.: Vector, 2010.
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. Handbook of Dietetics edited by V.A. Tutulyana, M.A. Samsonova. 3rd ed., M.: Medicine, 2002, pp. 209–217.
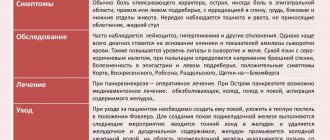
Symptoms
Symptoms of pancreatic damage in different diseases are similar. The patient experiences severe pain and dyspeptic disorders. Pain is felt in the abdomen and epigastric region. The pain can be either constant or intermittent. It intensifies if the patient eats fried and spicy foods. During palpation, pain may appear in the left hypochondrium.
Dyspeptic symptoms:
- vomit;
- diarrhea;
- nausea.
If you have problems with the pancreas, you may experience decreased appetite and weight loss.
General principles of child nutrition
The child's diet should be balanced. His body must receive a sufficient amount of vitamins and microelements that are necessary for his normal growth and development.
Basic principles of baby nutrition:
The energy value of the diet should correspond to daily energy expenditure.
- The amount of proteins, fats and carbohydrates in the diet should correspond to the proportion 1:1:4;
- The range of products should be varied.
- All products must undergo proper culinary and technical processing.
- It is recommended to give food to the baby 4-5 times.
For a growing body, it is important that through food it receives not only proteins, carbohydrates and fats, but also amino acids, trace elements and fatty acids. These components are not produced in the baby's body, so they must come from outside.
When compiling a menu, you should take into account height, weight, development speed and environmental conditions.
The child’s diet should contain trace elements and mineral salts:
- selenium;
- fluorine;
- iodine;
- selenium.
It is important to develop a child’s nutritional culture and self-care skills. It is parents who lay down useful habits and healthy lifestyle skills.
What needs to be completely excluded
After diagnosing a pancreatic disease, the child is prescribed a fairly strict diet, which involves giving up many foods. First of all, you should eliminate food, which improves the production of enzymes and also enhances the functioning of the pancreas.
The amount of sugar consumed should be significantly reduced; salt should be, if not completely eliminated, then its consumption should be minimized.
For any form of pancreatic disease, rich broths, fatty meats and fish should be excluded from the menu. The following categories of products are also prohibited:
- mushrooms;
- sausages;
- chocolate;
- sauces and hot seasonings;
- radish;
- tomatoes;
- citrus;
- baking;
- coffee;
- condensed milk.
It is important to follow all the doctor’s recommendations; this is the only way to avoid exacerbation of the disease.
Features of a child’s diet in different forms of the disease
In childhood, based on statistical data, a disease such as pancreatitis, which occurs in chronic or acute form, rarely occurs. Mostly children are susceptible to a reactive type of illness, which in medical terminology is called dyspancreatism. With this type of pathological condition, the children's pancreas, which is responsible for the production of digestive enzymes, ceases to function normally due to somatic disorders or frequent dietary disorders.
In order to help your child cope with the disease, it is necessary to correctly adjust the diet, including in the daily menu only those foods that the doctor allows.
All restrictions in the children's diet necessary for inflammation of the pancreas are directly dependent on the type of disease developing in a small child. To learn more about the nuances of the diet prescribed for children, you should look at the table below. It indicates the main characteristics of the children's dietary menu, which are recommended by the famous TV presenter, Dr. Komarovsky.
Principles of the dietary table for pancreatitis in a child

| Form of the disease | Principles of nutrition |
| Acute pancreatitis | From the moment the disease is diagnosed, diet No. 5 is prescribed, which is followed for at least a month. The first week she is very strict, and then as the baby’s health improves, the table begins to gradually expand. But the child must follow the principles of the dietary diet for at least five years, even if there are no negative symptoms. Gross errors in the menu and in the future are undesirable. |
| Reactive type of disease | The diet correction recommended for the baby by a gastroenterologist must be followed for at least 14 days. After this period, there will be no strict restrictions in the diet, but the doctor will advise you to feed the child according to his age, including only benign foods in the menu that do not cause damage to the mucous membrane. |
| Chronic process | After the exacerbation ends, the strict diet will be canceled and a less gentle diet option will be prescribed. But the diet will remain selective (many products will be completely prohibited) and it will be necessary to adhere to it for life. |
Each stage of the disease requires the baby to adhere to a certain diet with strict adherence to all doctor’s recommendations. But even despite the existing bans on certain types of foods due to this disease and strict requirements for food management, parents can make their child’s daily menu not only nutritious, but also tasty. By showing a little imagination when preparing a dish from a meager list of ingredients, you can please even the most capricious and picky eater of a child.
Diet for exacerbation of pancreatic disease
The purpose of the diet during exacerbation of pancreatic pathology is to reduce the production of enzymes that affect the organ tissue. Diet requirements:
- low fat and sugar;
- average energy value;
- minimal amount of carbohydrates;
- heat treatment by boiling or steaming;
- a small amount of coarse fiber;
- lack of spices and seasonings.
We recommend: Convulsions during fever in a child
During an exacerbation, it is better to fast and introduce vegetable broths into the diet. After 3-4 days, you are allowed to take porridge. They can be cooked in water or diluted milk.
Portions should be reduced, and the frequency of meals increased to 5-6 times a day.
Authorized Products
The diet for reactive pancreatitis may consist of:
- vegetable, cereal and pasta soups;
- lean varieties of poultry, meat, fish;
- dried white bread, unsweetened cookies, crackers;
- low-fat fermented milk products;
- porridge (oatmeal, rice, semolina, buckwheat) and pasta;
- vegetable (up to 15 g per day) and butter (up to 30 g) oil;
- boiled or baked potatoes, cauliflower, beets, carrots, green peas, pumpkin;
- egg white omelettes;
- non-acidic berries and fruits;
- rosehip decoction, weak tea, juices, compotes, jellies, mousses without sugar.
Approximate diet
On the third day after fasting, low calorie foods are introduced. They do not activate the secretion of large amounts of gastric juice and enzymes. Liquid meals are also introduced. The daily diet is best divided into 7 meals.
The patient needs to drink plenty of water, juices and decoctions. From the fifth day, the caloric content of dishes increases slightly. You can consume up to 600-700 calories per day. For breakfast on days 6-8, you can prepare porridge in water with a little sugar and apples. Vegetable puree is perfect for second breakfast. It can be potato or carrot. As the main part of the second breakfast, you can serve a piece of boiled fillet.
Lunch - vegetable broth, mashed potatoes with a small piece of boiled beef. As a dessert, you can have a grated apple. Cottage cheese diluted with milk is perfect for an afternoon snack. Cottage cheese should be low-fat. Before going to bed, you can give your child non-acidic kefir.
From the second week of diet, the amount of fats, carbohydrates and proteins increases. Dishes are also served without salt, but in 5 servings. It is recommended to enrich the diet with water-soluble vitamins.
After the acute phase, the patient can be given light vegetable broths, boiled meat and homemade cottage cheese. The diet should be followed for a maximum of one year. Further nutrition will depend on the condition of the pancreas.
Diet during an exacerbation
The diet for reactive pancreatitis depends on what phase the disease is in - exacerbation or remission.
In the acute stage of the disease, during which the patient experiences very strong pain, complete fasting is indicated for the first few days. Only drinking medicinal mineral waters in small quantities and in small sips is allowed.
The complete physiological rest created in this way for the pancreas helps to reduce gastric and pancreatic secretion, which leads to the removal of clinical symptoms of the disease.
Eating should begin gradually and very carefully, no earlier than the fourth day, making sure that the food is as gentle as possible not only for the pancreas, but also for the entire digestive system as a whole and corresponds to treatment table No. 5P.
After a week, the menu of a patient diagnosed with “acute reactive pancreatitis” can include:
- jelly and slimy soups;
- stewed and boiled vegetables;
- liquid porridge;
- steamed beef, chicken and fish cutlets;
- kefir;
- weakly brewed tea, rosehip decoction;
- baked apples.
The total calorie content of the diet at this time should not exceed 2500-2700 kcal per day, the norm of liquid consumed is 1.5 liters, salt consumed is 10 g (in the first 2 weeks you should cook without salt). The temperature of the food should be between 45 and 60ºС, the consistency of the dishes should be semi-liquid or liquid.

A diet for reactive pancreatitis in acute form implies a complete exclusion from the menu for a long time:
- smoked, fried foods;
- marinades, canned food and pickles;
- sour cream and cream;
- lard;
- muffins and fresh bread;
- alcohol.
A strict diet and compliance with all recommendations can prevent the development of a disease such as acute reactive pancreatitis into a chronic form.
Prevention
To avoid the development of pancreatic disease, it is necessary to maintain a healthy lifestyle and carefully monitor your diet. The following products must be included in the diet:
- turmeric;
- buckwheat;
- spinach;
- broccoli.
Turmeric has anti-inflammatory effects and also prevents the formation of gallstones. Buckwheat normalizes the functioning of the digestive system and removes toxins. Spinach supports pancreatic health, and broccoli contains vitamins K and C. You should avoid unhealthy, fatty foods, as well as alcohol consumption.
Diseases of the pancreas cause severe discomfort. It is important to diagnose and begin treatment in a timely manner. For therapy to be effective, you must follow the diet prescribed by your doctor.
Sample menu
An approximate daily menu for a person suffering from a disease such as reactive pancreatitis may consist of the following products and dishes:
- First breakfast: steam omelette, oatmeal with water, a glass of carrot juice. (Both the vegetables themselves and their juices are rich in antioxidants and can relieve clinical symptoms of pancreatitis.)
- Second breakfast: a portion of low-fat yogurt with blueberries, whole grain bread. (Whole grains and fresh berries are low in fat, making them very healthy to eat.)
- Lunch: buckwheat soup, boiled turkey meat stew, grain bread, apple jelly, rose hip decoction. (Lean meat satisfies the body’s need for easily digestible proteins, fats, and microelements.)
- Dinner: baked pollock, mashed potatoes, salad with low-fat dressing, weak tea. (Gentle methods of cooking - boiling, baking, grilling - make meals tasty and healthy.)
- At night: kefir and a few crackers.
Reactive pancreatitis is a serious and insidious disease, fraught with repeated relapses if the principles of proper nutrition are not followed. Only a long-term diet and a serious attitude towards it, a well-chosen nutrition menu and giving up bad habits will help to avoid complications and new attacks of a disease such as pancreatitis, and will allow you to maintain health for a long time.
Author : Zagorodnyuk Mikhail Petrovich, especially for the site Zhkt.ru