Sigmoid colon cancer is the second most common cancer in men and women. For a normal population, the statistical risk of developing colorectal cancer is about 6%, and for risk groups (for example, with hereditary susceptibility) it is much higher. In this article we will look at sigmoid colon cancer, the first symptoms, pathophysiology and treatment methods.
Cancer
Attention! In the International Classification of Diseases, 10th revision, the disease is designated by code C18.7.
Physiology
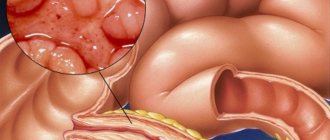
The vast majority of carcinomas are associated with benign tumors of the mucous membrane (adenomas, polyps). The likelihood of degeneration depends on the histological structure and size (from one centimeter) of the benign neoplasm.
The accumulation of mutations with age leads to irregular and uncontrolled cell division. They lose contact with other intestinal cells and invade surrounding tissues. If such abnormal cells reach the blood or lymphatic channels, they can travel to various parts of the body and form metastases. The most common site of degenerated tissue is the sigmoid colon.
Neoplasm
The tumor can migrate to the lungs and liver. From these organs, cancer cells can spread throughout the body. People who have colon polyps are at particular risk of developing colorectal cancer. Thus, there are certain genetic diseases (familial adenomatous polyposis) that, if not treated in a timely manner, can lead to cancer.
Methodology

How is sigmoid colon resection performed? The course of the operation depends on the type of pathology. In case of intestinal volvulus, which provokes the development of gangrene, a Hartmann or Mikulicz operation is usually prescribed.
What makes it special? Resection of the sigmoid colon according to Hartmann involves removing the dead portion of the sigmoid colon, suturing the distal end and further removing the meatus. This method is usually used for elderly and debilitated patients.
Resection of the sigmoid colon according to Mikulicz is carried out in two stages. First, part of the sigmoid colon is removed. Its ends are stitched together over a length of 5 cm. After this, they are sewn in the form of a double-barreled shotgun into the peritoneal wall. After 3.5 months, the intestinal fistula is closed.
The method of performing the operation is determined by the nature of the development of the pathology. If a tumor located in the middle third of the sigmoid is detected, complete removal of the sigmoid intestine may be required.
Causes of pathology
A tumor of the sigmoid colon is a “silent killer.” For many years it has been asymptomatic. If intestinal cancer manifests itself as discomfort, then, as a rule, this indicates the last stage of the disease. This is why 27,000 people die from the disease every year - a number that can be significantly reduced with early diagnosis.
It is now known that some of the genes are time bombs that are passed on through generations. Almost a third of people with cancer have relatives who suffered from the disease.
In the following cases, it is recommended to consult a doctor and undergo an examination:
- One or more family members were diagnosed (father, mother, sister or brother) with uterine or colorectal cancer before the age of 45,
- A first-degree relative (father, mother, sibling) was diagnosed with adenocarcinoma or polyposis (obligate precancer of the colon) before the age of 40 years,
- Two second-degree relatives who have sigmoid colon cancer or other types of carcinoma (uterine, ovarian, stomach, small intestine, or bladder cancer),
- Chronic inflammatory bowel disease (ulcerative colitis or Crohn's disease).
The occurrence of bowel cancer additionally depends on individual risk factors. The following factors can increase the likelihood of developing a malignant tumor:
- Age 50 and older (changed genes due to aging processes),
- Too little fiber in the diet
- Excessive consumption of meat products (especially red meat),
- Physical activity and exercise less than twice a week,
- Obesity 1, 2 and 3 degrees,
- Smoking,
- Regular consumption of alcoholic beverages (more than one glass of beer, schnapps or wine per day).
People who have one or more of these factors have a significantly higher risk of developing cancer. They should definitely undergo regular cancer screening.
Postoperative period
What makes it special? What should be the diet after resection of the sigmoid colon? Semi-finished products, fried and fatty foods are contraindicated for patients. It is better to cook food by steaming or in a slow cooker.
The diet after resection of the sigmoid colon involves eating mainly liquid foods: cereals, light soups and purees. You can gradually introduce solid foods into your diet. The menu is designed so that the body receives all the vitamins and microelements necessary for the patient’s recovery. After resection, canned food, smoked foods and alcohol should be excluded. About 10 days after surgery, you can begin eating low-fat dairy products, eggs, and meat. After a month, you can include regular dishes in the menu. The main condition is that the food must be well chopped.
Symptoms and clinical manifestations
For a long time, bowel cancer does not cause any symptoms. As mentioned above, it only appears in the last stage.
People over 45 years old should pay attention to the following signs:
- Any change in bowel habits (frequent flatulence, persistent diarrhea or constipation) over a short period,
- Abdominal pain,
- Blood in the stool (even with diagnosed hemorrhoids),
- Constant need to defecate.
The appearance of blood in the stool is an important sign of colorectal carcinoma. Any cause of blood in the stool should be thoroughly investigated. Some forms of tumors produce large amounts of mucus, which can then be seen in the stool.
Other symptoms include fatigue, decreased productivity, weight loss and abdominal pain. Serious signs of illness, such as massive stomach upset, nausea, or yellowing of the eyes (jaundice), appear only in terminal cancer that has metastasized to the liver.

Jaundice
Late period of rehabilitation
Since the main purpose of the sigmoid colon is to absorb moisture from stool, when this part of the intestine is removed, the stool can become liquid and almost uncontrollable. This may cause some inconvenience. After the operation, you will have to radically revise your diet. The late period of rehabilitation requires certain restrictions. Usually the patient is prescribed a diet with a minimum content of toxins. The menu should not contain anything spicy, fatty, smoked or spicy. Doctors do not advise consuming legumes, rough foods made from plant fibers, carbonated drinks, and whole milk. This will reduce gas formation.
Stages of cancer
Based on the TNM classification, doctors describe stages of the disease to describe how far the cancer has progressed. There are stages from zero to four. This system was developed by the International Union Against Cancer and is used in many countries.
Stages of cancer development:
- UICC stage 0: These are early forms of colon cancer. The likelihood of such a tumor spreading is very low, since it does not yet have contact with the bloodstream or lymphatic vessels,
- UICC stage I (“stage 1”): The tumor has already grown into the connective tissue layer below the surface of the mucosa (T1) or further into the muscle layer (T2). However, the cancer cells have not spread to surrounding lymph nodes (N0) or other organs (M0),
- Stage II UICC (“stage 2”): tumors that have not yet spread (N0, M0). The affected cells have reached the outer layer of the intestinal wall (T3, UICC stage IIA), broken through it and entered the peritoneum (T4a, UICC stage IIB) or surrounding organs and tissues (T4b, UICC stage IIC),
- UICC stage III (“stage 3”): Surrounding lymph nodes are involved but there is no evidence of distant metastases (M0). For finer differentiation at stage IIIA-C, you need to know how many lymph nodes are affected by the tumor,
- UICC stage IV (“stage 4”): If distant metastases (M1) are present, each colorectal cancer is classified as stage 4, regardless of tumor size or number of lymph nodes involved. Stage IVA means the tumor is limited to one organ, while stage IVB means metastases are found in more than one organ. Stage IVC means the abdominal cavity is affected.
Important! Contrary to popular misconceptions, there is no stage 5 cancer. Many patients confuse it with stage IVC. Terminal stage of cancer development - UICC IV.
Early diagnosis
A stool occult blood test should be performed annually, with each positive result confirmed by colonoscopy. Because polyps and tumors do not bleed constantly but at indeterminate intervals, stool tests can only detect about 30% (stool immunoassay has a higher detection rate) of polyps or tumors. Blood chemistry test results can also be affected by certain medications and foods.

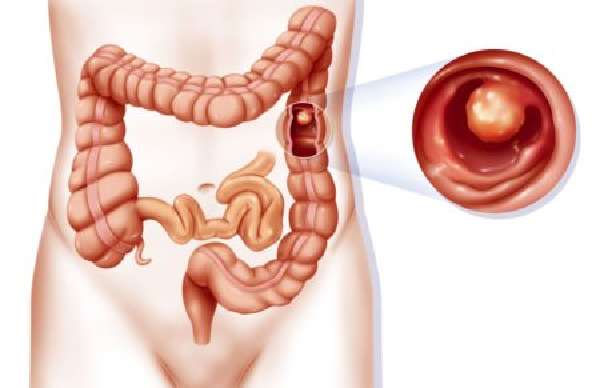
Colonoscopy
The standard stool test that has been used since 2002 is the M2-PK test. It detects a tumor-specific enzyme (marker) in the stool. The test can be taken from a doctor or purchased at a pharmacy. Scientific long-term studies of this test are not yet available.
Another method in the context of annual cancer screening is rectal palpation, in which the doctor scans the colon with a finger. However, this method alone is not sufficient for screening colorectal cancer, since only tumors in the lower part of the colon can be detected. Only a third of tumors grow in the rectum, and colon cancer is increasingly found in the upper part.
A new form of colon cancer screening is the Septin-9 blood test. If a tumor is present, altered genetic material is released into the blood early in the disease, which can be detected in a blood test. Depending on the stage, the detection rate for this method is at least 67%, which is higher than stool blood testing but lower than colonoscopy.
The Septin-9 assay does not require dietary modification or laxatives, which is a definite advantage. It can be used in patients for whom colonoscopy is not an option. However, the Septin-9 test is not widely used in clinical practice today.
Diagnostics
In most cases, colon carcinoma is detected by rectal palpation and colonoscopy. If you need to get an idea of the histological type and degree of degeneration (dysplasia) of the tumor, the doctor simultaneously with endoscopy performs a tissue sample (biopsy). If colonoscopy does not provide the desired information, X-ray examination using a contrast agent is used. It is important to carry out a differential diagnosis with autoimmune intestinal diseases, which have similar symptoms.
Using ultrasound, x-rays and computed tomography, the extent of cancer infection and the formation of metastases are recorded. Depending on the stage of the disease, some patients have a protein in their blood that is released by the tumor, called carcinoembryonic antigen (CEA). It is not suitable for diagnosing cancer, but determining its concentration is useful in the postoperative period. If the concentration increases again, it is a sign that the cancer is returning.

Ultrasound
For the prognosis of the disease, it is important how much cancer has entered the intestinal wall during the disease. The closer it is to the intestinal outlet, the worse the prognosis, since the tumor will spread throughout the body through the lymph nodes and blood vessels.
Cancer prevention and colonoscopy
Many experts recommend having colonoscopies at regular intervals (every three years). Colonoscopy along with a rectal examination from the age of 50 helps in the early diagnosis of cancer. Regular stool testing for occult blood should also be part of cancer screening.
Features of treatment
The earlier disorders of various etiologies (polyps or cancer) are detected, the fewer treatment procedures are required, and the better the prognosis of the disease. The goal of therapy is timely removal of the resulting carcinoma. Age and general condition, tumor grade are important factors influencing the outcome of the disease.
Polyps
Surgery
With invasive surgery, the surgeon seeks to preserve the integrity of the anal sphincter by removing the affected part of the colon. But this is not always possible, especially if the cancer is located in the lower part of the intestine or has already migrated widely. Metastases (mostly in the liver) are also removed surgically.
In recent years, overheating (hyperthermia) with microwaves or by injecting chemicals directly into metastases has been added as additional therapeutic options. Combining surgery followed by chemotherapy improves prognosis. It is hoped that in the future treatment will become possible even with severe metastases.

Surgical intervention
Palliative care
If surgery cannot be performed for certain reasons, doctors try to relieve symptoms (palliative care). This is achieved by maintaining intestinal patency, using medications and x-rays.
Proper diet
Scientists have proven that adding certain substances to the diet protects the intestines from the formation of tumors. Therefore, doctors recommend using vitamins (vitamin E, C, folic acid) and acetylsalicylic acid as preventive measures. However, some studies have produced conflicting results in this regard. Sometimes even when using high amounts of vitamins, cancer occurred.
Instead of taking dietary supplements, it is better to eat healthy foods that are low in fat, low in carbohydrates, and high in fiber.
Advice! Exercise helps maintain healthy bowel function and reduce obesity.
Preparation for resection of the sigmoid colon
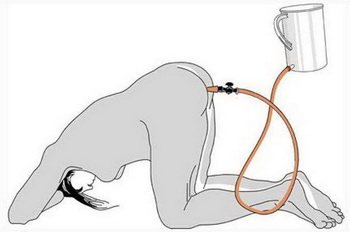
Before the day of resection, the patient must undergo preparation. It is imperative to completely clean the intestines to eliminate the possibility of infectious infection during resection. This will avoid further postoperative complications, since the colon contains a large number of bacteria that can cause inflammation. Laxatives and enemas are used for cleansing. The method is chosen individually for each client; laxatives are prescribed in such a proportion that taking them does not cause diarrhea. The preparation period can last all day.
A few days before the operation, you need to adhere to a special diet - do not eat solid or hard-to-digest foods. You can eat liquid dishes - soups, milk porridges.
Before resection of sigma, the doctor always prescribes the necessary medications. These include medications to normalize blood pressure, diuretics and inhibitors. These drugs help normalize blood pressure during surgery, reduce the risk of cardiac complications, and help remove fluid from the operation. A few weeks before surgery, you should stop taking medications with an anti-inflammatory effect (Aspirin, Nurofen, Ibuprofen). Their action is aimed at changing the functioning of platelets, which can affect blood clotting. The intake of dietary supplements and vitamins should be discussed with your doctor; it is better to exclude them for a certain period before resection of the sigmoid colon. 4-5 days before surgery you need to stick to a diet.
Before resection of the sigmoid colon, the patient is examined by an anesthesiologist. The anesthesiologist assesses the general condition of the patient, which influences the prescription of anesthesia. While preparing the bowel for resection, you should not eat any food, and after midnight before the operation, you should not drink water or other liquids.
Forecast
If the malignant tumor cells are limited to the intestines, the chances of recovery are high. Even if the intestinal wall is damaged and the lymph nodes are involved, more than half of patients can still be cancer-free. However, if multiple liver metastases are present, the chance of survival is still low. If there is only one metastasis, there is still hope for recovery. But even if the cancer is successfully removed, there is a 20 to 30% chance that it will come back.

Metastases in hepatocytes