If left untreated, Staphylococcus aureus can cause severe diseases in various organs and systems of the body. This article will tell you how to detect and treat Staphylococcus aureus.
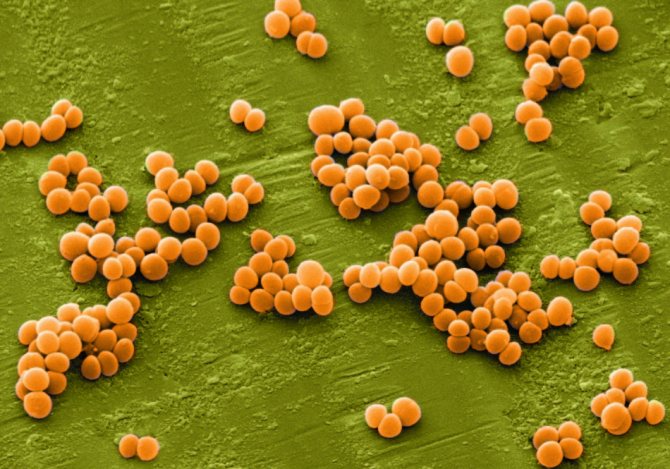
Staphylococcal infection refers to a number of different diseases caused by pathogenic bacteria. These bacteria have the form of round cocci, which are located in pure culture in the form of grape bunches.
Staphylococci are the cause of diseases such as tonsillitis and pneumonia, purulent diseases of the skin and subcutaneous tissue (acne, pimples), enterocolitis and sepsis.
Staphylococcus is the cause of purulent skin lesions
IMPORTANT: Pathogenic staphylococci are very dangerous and practically lead among purulent diseases accompanied by an inflammatory process, as they are highly resistant to antibiotics.
There are many varieties of these pathogenic bacteria, however, in terms of the degree of pathogenicity and the speed of spread of infection from an infected organ throughout the body, there are no competitors for Staphylococcus aureus, or scientifically Staphylococcus aureus .

Staphylococcus quickly spreads throughout the body, affecting various organs and systems
Causes of Staphylococcus aureus
As paradoxical as it sounds, the bacterial baggage of the human body is replenished with Staphylococcus aureus in most cases in medical institutions.
Hospital workers, immunocompromised patients, diabetics, and women during their “critical days” are the main carriers of bacteria.

Medical institutions often become the site of infection with Staphylococcus aureus
IMPORTANT: If a person’s immune system is strong enough, and there is no damage to the skin and mucous membranes, a small amount of staphylococcal bacteria that enter such an organism will not cause the disease. But if there is an open wound, or the number of bacteria is too high, then “trouble cannot be avoided.”
The golden ball of bacteria can be found in a variety of places: in the intestines, in the mouth and nasopharynx, in women in the most intimate places, in the armpits.
Staphylococcus aureus under a microscope
Symptoms of infection in children
Staphylococcus: under a microscope
This disease manifests itself differently in different children. Symptoms and signs of infection directly depend on the following factors:
- baby's age
- environment where pathogenic microorganisms live
- the child’s health status and the effectiveness of his immune system
- type of staphylococcus
Only a qualified doctor can correctly diagnose the disease. Parents must responsibly monitor the general condition of the baby and report it to a specialist. Staphylococcal infection can have two forms: early and late.
Read: Diet for gastritis and pancreatitis is the key to health and quick recovery
The early form is characterized by a more rapid manifestation of the development of infection in the body: the first signs are noticeable several hours after the child is infected. Signs of the late form appear after three to five days. Staphylococcal infection is characterized by the following possible symptoms:
- various rashes on the skin: boils, rashes, pustules, stomatitis. If unusual spots appear on your baby's skin, you should consult a doctor.
- conjunctivitis
- general deterioration of the baby’s condition (high temperature, lethargy)
- digestive disorders (diarrhea, poor appetite, vomiting)
Staph infection has various symptoms. Only a doctor can correctly diagnose the disease, therefore, if certain signs of the disease appear in the baby, it should be shown to a specialist.
Staphylococcus aureus in infants and newborns: symptoms
The human body becomes familiar with these ubiquitous bacteria from the first second of its birth.
Having existed peacefully for 9 months in the mother’s womb, disinfected by nature, at the moment of birth, first passing through the birth canal, then applying to the breast, the child experiences an attack by a mass of various bacteria, among which Staphylococcus aureus is not the least important.

For the first time a person encounters Staphylococcus aureus in the first seconds after birth
In most cases, the newborn copes with this infection without problems. However, imperfections in the gastrointestinal tract and immune system of the little man can lead to the development of pathology.
The following may contribute to the development of the disease:
- pathological pregnancy and childbirth
- premature birth
- low birth weight
- failure to comply with basic baby hygiene rules
How to determine the presence of Staphylococcus aureus bacteria in a child’s body?
Typically, symptoms depend on which organ is damaged:
- When the skin , acne, boils, redness, and, in general, various suppurations appear on the baby’s epidermis. The fluid that fills the purulent blisters is yellow-green or green in color. If you do not respond in time and do not start treatment, this can develop into sepsis (blood poisoning)
- If the infection has settled on the mucous membranes of the nasopharynx and throat, the baby complains of pain in these places. As the infection progresses, otitis, sinusitis, and sore throat are possible.
- Once inside the body , the pathogenicity of Staphylococcus aureus can cause ARVI, pneumonia and even meningitis. Such diseases are accompanied by fever, cough, sometimes vomiting and diarrhea.
- If toxins enter the intestines, pathology is observed in the functioning of the gastrointestinal tract with all the usual symptoms: nausea, vomiting, diarrhea, abdominal pain, fever, lack of appetite and general weakness
IMPORTANT: It is very difficult to make a correct diagnosis based only on clinical characteristics, so it is necessary to undergo tests (blood, feces, cultures and scrapings) to make sure that the cause of the disease is the causative agent of Staphylococcus aureus.

Test results will help confirm or refute the presence of Staphylococcus aureus in the body
What kind of stool does Staphylococcus aureus have?
Staphylococcus aureus (in the study form it is designated as Staphylococcus aureus) is one of the many opportunistic cocci. Found in the stool of a healthy person. The disease (staphylococcal infection) develops only when there is a significant number of microbial cells and a significant weakening of the immune system.
Pathogen danger
Staphylococcus aureus is found on the surface of human skin and mucous membranes, as well as in biological fluids (feces, urine).
In most cases, Staphylococcus aureus is discovered accidentally during a routine examination. A person does not feel such a symbiosis with the microbe, that is, there are no clinical symptoms.
In such a situation, treatment is not required, since the microorganism does not have a damaging effect on human organs and tissues - there is no disease.
When the immune system is weakened (congenital or acquired immunodeficiency, long-term infectious diseases, chronic endocrine pathology), conditions arise under which Staphylococcus aureus actively multiplies, penetrates tissues, and produces pathogenicity factors (enzymes and toxins). As a result of the colonization of microorganisms with the bloodstream, the formation of purulent-inflammatory foci in the internal organs occurs. This condition is called staph infection .
Depending on the location of the pathological process, the following forms of staphylococcal infection are distinguished:
- osteomyelitis (inflammation of bone tissue);
- purulent foci in the skin, subcutaneous fat (cellulitis, abscess, furunculosis);
- bursitis or synovitis (joint damage);
- pneumonia, bronchitis, pleurisy;
- enterocolitis and enteritis (inflammation of the intestines);
- damage to brain tissue (meningoencephalitis and meningitis);
- blood poisoning (staphylococcal sepsis).
Any of the above conditions is a serious test for the human body, since with staphylococcal infection local changes are combined with severe general intoxication.
It is possible for the acute form of the disease to transform into a chronic form - with periodic exacerbations and remission. Damage to brain tissue, pulmonary and septic conditions do not always have a favorable prognosis - without adequate treatment, the death of the patient cannot be ruled out.
Pathways of transmission and growth of bacteria
Staphylococcus aureus is widespread in nature and on objects surrounding humans. This microbial agent is resistant to environmental factors, so it is not possible to talk about its complete destruction.
Staphylococcus aureus is transmitted in the following ways:
- food – when consuming “contaminated” products;
- contact – through direct communication with an infected person or when using common household items (dishes, towels);
- aerosol (through the air);
- artificial (in the process of medical manipulations in any health care facility).
It is impossible to avoid contact with Staphylococcus aureus; it is important to prevent the development of an infectious process. The growth and reproduction of staphylococcus is promoted by:
- immunodeficiency (acquired and congenital);
- unbalanced diet (with excess carbohydrates);
- chronic pathology;
- repeated infectious processes of another etiology;
- bad habits.
Simple and clear points reduce the likelihood of developing a staphylococcal infection:
- balanced diet;
- compliance with the work and rest regime;
- timely treatment of chronic diseases (achieving long-term remission).
Norms for content in feces
The concept of the norm for the content of Staphylococcus aureus in feces for a non-specialist may look somewhat ambiguous.
- In a normal stool examination (bacteriological), this microorganism may not be detected - this is a negative answer, the best possible option.
- Another option is a positive answer, that is, Staphylococcus aureus was found in the patient’s feces.
A positive result of bacteriological examination of stool without clinical manifestations of the disease is not the basis for diagnosis and subsequent treatment.
Symptoms of the disease
Clinical manifestations of staphylococcal infection are determined by the predominant localization of the pathological process. When Staphylococcus aureus affects the digestive canal, the following is noted:
- prolonged nausea combined with repeated vomiting;
- lack of appetite and aversion to any food;
- diffuse abdominal pain;
- loose stools often mixed with mucus and streaks of blood.
Gastroenterocolitis of staphylococcal etiology is characterized by a long course and slow recovery of the patient. Staphylococcal gastroenterocolitis is especially severe in preschool children, as well as in premature babies. It is these patients who are most likely to develop a generalized staphylococcal infection - sepsis.
Treatment
If a person has Staphylococcus aureus in the stool, but there are no signs of dysfunction of the digestive canal, then treatment is not necessary. This condition is regarded only as the fact of the presence of Staphylococcus aureus in the intestine as a representative of opportunistic flora.
Therapy for staphylococcal infections, including those localized in the digestive canal, is necessary when a person’s general condition changes and characteristic clinical symptoms appear.
Doctors practice an integrated approach, including dietary nutrition, antibacterial agents and other medications.
Hygiene
Contamination with Staphylococcus aureus is possible due to simple non-compliance with personal hygiene rules. This will significantly complicate treatment and delay the recovery process. During the entire period of therapy, the patient must:
- wash your hands thoroughly and often;
- do not use other people’s household items and utensils;
- take a shower (not a bath) every day;
- Be careful when communicating with other people (minimize direct contact to avoid infecting others).
Nutrition
Diet also plays an important role in the treatment of staphylococcal infections of the digestive canal. Dietary restrictions are:
- all products must be boiled, baked or stewed; fried foods, as well as raw vegetables and fruits are not allowed;
- porridge with water, low-fat fermented milk products, vegetable soups, crackers are allowed;
- Sweets, hot and spicy foods are prohibited.
It is very important to gradually expand your diet. That is, after the general condition improves and the severity of local symptoms decreases, a new (non-dietary) product can be introduced every 1-2 days, for example, fatty cheese or vegetable soup with meat broth. If the patient feels well after this, then the diet continues to expand - the diet gradually approaches the usual table.
Drug treatment
Prescribed only by the attending physician. Attempts at self-therapy can only worsen the patient's condition. Complex treatment uses:
Source: https://morewomen.ru/info/kakoj-kal-pri-zolotistom-stafilokokke/
Staphylococcus aureus in the throat: symptoms
If Staphylococcus aureus bacteria find refuge on the mucous membranes of the baby’s throat, this will definitely cause a sore throat.
Its symptoms are absolutely identical to streptococcal disease:
- heat
- sore throat up to difficulty swallowing
- the appearance of ulcers on the mucous membrane and tonsils
In severe cases of the disease, disorders in the intestines and acute reluctance to eat are possible.

Staphylococcus aureus in the throat
Features of the infection
Staphylococcus aureus (from the Latin Staphylococcus aureus) appears to be a non-motile aerobic bacterium, shaped like a ball. The bacterium belongs to the group of gram-positive. The bacterium received its beautiful name for its golden glow at the time of sowing in a favorable environment (research in laboratory conditions). Under a microscope, staphylococcus resembles a bunch of grapes, hence the name of the bacterium itself (from the Greek slaphyle - “bunch”, and coccus - “in the form of a ball”). Staphylococcus aureus is present on the skin of all people, and with strong immunity it rarely manifests itself as pathogenic. The frequency of infection in children is due to the existence of bacteria everywhere: toys, breast milk, skin and mucous membranes of bacteria carriers, household items.
Children tend to explore the world with all their senses; it is especially important to taste new objects, neglect hygiene rules, and come into contact with people and animals, so it is children who become susceptible to infection. The pathogenic activity of Staphylococcus aureus is associated with the following conditions:
- resistance to antiseptic agents and external influences (withstands freezing, boiling, alcohol, peroxide, drying);
- high resistance to antibiotics (due to the production of special enzymes penicillinase and lidase);
- production of endotoxin (the substance provokes severe intoxication of the body).
Important! The human body completely lacks immunity to Staphylococcus aureus, so a person who has been ill can easily get sick again. Staphylococcus aureus in the feces of infants can also occur in a hospital setting, which often explains the infection of newborns. Hospital staphylococcus occurs due to violations of the rules of aseptic procedures and medical instruments.
Staphylococcus aureus in the nose: symptoms
Every second person is a carrier of infection in the nasal cavity. Therefore, in this part of the body, staphylococcus is treated only when inflammation leads to a chronic runny nose.
IMPORTANT: As soon as favorable conditions appear (hypothermia, taking antibiotics, long-term use of vasoconstrictor nasal medications, general decrease in immunity), bacteria begin to actively multiply, which leads to rhinitis and sinusitis.

Staphylococcus aureus in the nose can cause chronic rhinitis
Features of treatment
Staphylococcus is a dangerous infection that cannot be ignored. Treatment of Staphylococcus aureus in an infant can only be prescribed by a pediatrician:
- Immediately after the baby is born, millions of bacteria begin to attack his body. If the presence of staphylococcus is detected in a newborn, then it should be treated only in a hospital setting. Mothers are not recommended to give up breastfeeding, since it is through breastfeeding that the basic level of the protective system is formed.
- Staphylococcus aureus in a baby's stool requires immediate hospitalization. Parents should not give up on her under any circumstances.
- If the bacteria begins to actively multiply in the nose or throat, then this type of disease can be treated at home.
To treat the external version of the lesion, it is allowed to use brilliant green or chlorophyllipt. Among the folk methods, a decoction of calendula, chamomile or St. John's wort is very popular. Medications should only be prescribed by the attending physician. Self-medication will not give the desired result. Additionally, a bacterial culture will be required. To strengthen the immune system, it is advisable to take vitamin complexes.
It is much more important to pay attention to preventive measures. They will help the immune system to form correctly. In the future, the body itself will be able to overcome a purulent sore throat or any other infection.
The disease in the baby manifests itself in the form of severe pain in the abdomen, as well as in the form of yellow feces with impurities of foam. In this case, we can talk about infection. The child is prescribed a test that will determine the content of staphylococcus.
The doctor takes a swab from the throat and nose. The interpretation of the results obtained depends on the age and general well-being of the baby. Treatment involves taking medications to improve the functioning of the immune system. It is advisable to take medications if there are a large number of harmful bacteria in the smear.
Staphylococcus is difficult to fight. That is why parents are recommended to take exclusively preventive measures. Remember that only a doctor can choose the right antibiotics. Self-medication is dangerous and can even be fatal.
The moment when a baby is just born is always wonderful. It is from here that the child’s active exploration of the surrounding world begins. But here various infections may await him, among which the most dangerous is staphylococcal (especially hospital-acquired). Parents who have encountered a staphylococcal infection in an infant understand how much of a burden this is for an immature immune system, and how serious the consequences of the disease can be.
The infection is caused by bacteria of the genus Staphylococcus. Staphylococcus aureus is most often to blame for the occurrence of the disease in infants. According to statistics, 20% of children 2 years old are carriers of this bacterium in the nasal cavity. At the age of 4–6 years, staphylococci are already detected in 30–50% of children. Do not panic, because this type of microorganism is considered opportunistic. Normally, staphylococcus lives on the surface of the skin, mucous membranes of the nose, pharynx, pharynx, eyes, but does not cause infection. Under special conditions and if certain risk factors are present, infants may develop the disease.
There are several forms of infection in children. Let's look at the most common one - when Staphylococcus aureus begins to exert its toxic effects in the intestines of a newborn. In this case, the development of diseases such as paraproctitis, enteritis, enterocolitis, and acute food intoxication is possible.
Often the clinical symptoms of the pathogenic activity of staphylococcus in the intestines resemble manifestations of dysbiosis, acute intestinal infections, and acute respiratory viral infections. The child has frequent stools that have a pasty, watery consistency, often with mucus. Abdominal pain, lack of appetite, lethargy and weakness in the body, and vomiting appear. Due to intestinal colic, the child often cries.
Particular attention should be paid to the appearance of the following symptoms:
- greenish stool;
- foamy formations during bowel movements;
- pain in the abdomen.
These symptoms are more typical for staphylococcus in newborns. Some children may develop a fever. The incubation period can last from several hours to 4 days, depending on the form of infection, localization of the process, immunity and age of the patient. To establish an accurate diagnosis (many diseases have very similar symptoms), it is necessary to do a staphylococcus test and laboratory examination of the resulting material.
Staphylococcus aureus in the intestines, in feces
The presence of a pathogen in the human intestine is normal, so there is no particular reason to panic.
IMPORTANT: If the concentration of bacteria exceeds the permissible limits (above 104 IU), immediate action must be taken.
Symptoms of staphylococcus localization in the intestines:
- colic
- intestinal disorders
- bloody stool
- mucus in stool
- elevated body temperature
The incubation period is almost a day, so the first signs of infection will appear within a few hours after infection.
If diagnosed in time and correctly, this disease can be cured quickly and without consequences.

Colic and intestinal disorders are the main signs of the localization of Staphylococcus aureus in the intestines
If, as a result of an analysis of the child’s stool, Staphylococcus aureus is detected, but no pronounced clinical symptoms are observed, then the baby’s body gets along well with these bacteria and there is no need to go to war against them.
Etiological factors
The occurrence of Staphylococcus aureus in the feces of a child and an adult differs in its course, frequency of occurrence, and treatment process. Adults suffer from infection very rarely, but endure the entire period of the disease much more severely. The causes and contributing factors for the appearance of bacteria in feces also differ.

Signs of staphylococcus in children (colic)
Causes in children
The pathogenic activity of Staphylococcus aureus bacteria in a child is often caused by contact with carriers of the infection. Breasts become infected from the mother through breast milk or during the birth process. The main reasons for the appearance of Staphylococcus aureus in the feces of infants include:
- non-compliance with personal hygiene of a pregnant or lactating woman;
- deep prematurity;
- hospital infections (during long-term hospital stay);
- difficult labor process;
- long anhydrous period during childbirth;
- pathological pregnancy and weakness of the child’s body.
Staphylococcus aureus enters the umbilical wound, from where it spreads throughout the body through the blood. Infection is also possible during lactation, when a woman is a carrier of the infection. Unsterile feeding bottles, toys, contact with sick children - all this can provoke infection of a newborn baby.
Causes in adults
Infection in adult patients occurs due to contact with carriers on damaged skin and mucous membranes. The routes of infection with Staphylococcus aureus can be external and internal, and carriers of staphylococcus can be temporary or permanent. A chronic carrier of the bacteria may never develop a staph infection, but poses a potential danger to other people with weakened immune systems. The following routes of transmission of infection are especially noted:
- contact-household (ingress of bacteria through household items, personal belongings);
- airborne (inhalation of contaminated air, sneezing, coughing);
- airborne dust (dust can be household or street);
- fecal-oral or nutritional (vomit, feces, dirty hands);
- artificial way (insufficient processing of medical instruments during surgical procedures of any complexity).
In addition to the routes of transmission of infection, there are a number of provoking factors that can provoke the development of pathogenic activity of Staphylococcus aureus. The following are distinguished:
- diabetes mellitus (including decompensated);
- bad habits;
- decreased immunity of any origin;
- hypothermia, colds;
- chronic diseases of organs or systems;
- immunodeficiency virus (AIDS);
- burdened allergy history.
Important! A common cause of infection is poor hand hygiene and reduced immunity. If normally all healthy people have staphylococcus in the feces or on the skin, then when the immune system is weakened as a result of a common cold, pathological processes and symptoms of the activity of the bacterial environment can begin.
Staphylococcus aureus in adults
Adults, although less often than children, also suffer if the body becomes infected with Staphylococcus aureus bacteria.
There are two ways of developing the disease:
- infection
- intoxication
The development of the latter is possible only when golden bacteria settle in the body, producing toxins that purposefully penetrate the patient’s blood.
When the concentration of bacteria is extremely high, a very serious disease occurs - toxic shock. It occurs rarely and only in women, as it is associated with the use of tampons during “critical days.”
Almost all women have staphylococcus bacteria in the vagina, and during menstruation the outgoing blood should wash them away, but the tampon clogs the exit, and the accumulating bacteria begin to form toxins that are absorbed by the vessels.
As a result, a characteristic clinic can be traced:
- slight fever
- rash accompanied by peeling
- headache
- nausea
- lowering blood pressure

A toxic food infection that develops as a result of eating stale dairy, meat and confectionery products is also a common occurrence.
Reasons for the appearance of staphylococcal bacteria in the feces of a newborn
It is necessary to know the reasons for the proliferation of Staphylococcus aureus bacteria in the intestines of infants to treat symptoms. Most often, the infection develops in infants who are at risk for reasons such as:
- Pathological course of pregnancy;
- Premature birth;
- Long anhydrous period during childbirth;
- Hypotrophy, prematurity;
- Weakened immunity of the child;
- Failure to comply with hygiene rules for mother and newborn;
- The presence of Staphylococcus aureus bacteria in the mother;
- Long stay in the maternity ward (nosocomial infection).
It is important to know that there are certain ways that bacteria can enter a newborn's intestines. The causes of infection with Staphylococcus aureus in children who are not at risk are most often associated with the route of transmission of the bacterium.
Staphylococcus aureus is transmitted through:
- Blood during cord cutting;
- Cracked nipples during feeding;
- Toys, bottle, pacifier, pacifier (with insufficient hygiene rules);
- Medical equipment, instruments;
- Contact with a person infected with Staphylococcus aureus.
Let us emphasize once again that the mere fact of the presence of staphylococcus is not a sufficient condition for the occurrence of infection. Staphylococcus aureus in the intestines of infants causes infection only in cases where the child’s immunity is weakened and depressed.
Staphylococcus aureus during pregnancy
The presence of staphylococcus bacteria in the body of the expectant mother, exceeding the norm, can harm both the woman herself and her unborn baby:
- If the pathogen is on the skin, it can penetrate the mammary glands and cause purulent mastitis
- When the pathogen overcomes the fetal membrane and infects the unborn newborn, he develops numerous, quite painful, purulent skin blisters
- There are cases of staphylococcal bacteria entering the blood of a pregnant woman, resulting in, in addition to sepsis, inflammation of the heart membrane, which can lead to death.

Staphylococcus aureus during pregnancy
Disease prevention measures
It is, of course, extremely difficult to protect yourself from the disease, since staphylococcus bacteria are found everywhere. However, if you follow preventive rules and regulations, you can reduce the risk of infection. When caring for a newborn you should:
- maintain personal hygiene of mother and child;
- strengthen immunity;
- monitor the cleanliness of items that are used for feeding or playing with the baby (boil bottles, pacifiers after each use, wash toys with baby soap);
- keep the umbilical wound clean.
Daily washing, changing clothes to clean and ironed ones will not only help protect the baby from contracting various diseases, but will also teach him to be neat in the future. Older children should be taught to take care of themselves, explaining the importance of hygiene procedures.
The moment a baby is born is always wonderful and exciting. After all, it is from birth that a child begins to actively explore the world around him. However, from the first days of life, the baby is haunted by various dangerous microbes and bacteria. In this regard, a young mother, even before giving birth, should become familiar with the most common diseases that can be avoided by following preventive measures. One of the most common infections is Staphylococcus aureus in the intestines of infants.
Staphylococcus aureus in the stool of a healthy child is not uncommon and does not at all mean a disease. Even if staphylococcus is found in the intestines of a baby, this is not a cause for concern if there are no symptoms. You definitely need to look at the number of these microorganisms.
Staphylococcus aureus degree
stage 4 Staphylococcus aureus bacteria But occasionally, asymptomatic presence of these bacteria in the body occurs.
IMPORTANT: Often the presence of grade 4 staphylococcus is accompanied by skin inflammatory processes, as a result of which the epidermis dries out and peels off.
Sometimes the functioning of the respiratory tract is disrupted, and pathology is observed in the tissues of the musculoskeletal system.
Staphylococcus aureus test: normal
In medicine, there are certain standards for the content of staphylococcus bacteria in the body.

Analysis for Staphylococcus aureus
If the analysis shows the presence of a staphylococcal infection of the fourth degree, it is worth thinking about how to strengthen the immune system and maximally fortify the body so as not to create a favorable environment for the proliferation of bacteria.
Reviews from women who have had this disease
Natalia, 33 years old:
“I have suffered from colds very often for as long as I can remember. A runny nose and sore throat could occur almost every month. I never took it seriously, I just treated it like a common cold. This continued until I became pregnant.
When registering, they prescribed a bunch of tests. Including a swab of flora from the nose and throat. Staphylococcus aureus was cultured. It was he who was the cause of my endless pain. Treatment was prescribed, but it was not possible to completely get rid of the parasite, although I began to get sick much less often. Fortunately, there were no complications during pregnancy and childbirth. The baby was born absolutely healthy.”
Is Staphylococcus aureus contagious and how is it transmitted?
The most unpleasant thing is that it is very easy to catch these “cute” golden-colored bacteria (hence the name), since their distributor in 96% of cases is a person.
Of this number, up to 40% are asymptomatic carriers of staphylococcus strains, that is, it turns out that you can become infected from an absolutely healthy person.
IMPORTANT: The easiest way for the pathogen to enter the body is through scratches, abrasions, wounds, as well as the mucous membrane of the respiratory tract.
If a person leads a correct and healthy lifestyle, his immunity is strong enough to resist the pathogen present in the body in small concentrations.

A healthy lifestyle will save you from infection with Staphylococcus aureus
But if the motto “plow and fall” is the norm of life, then such an organism becomes an easy victim for bacteria and a favorable place for their reproduction.
No less significant factors for the development of infection are:
- taking antibiotics
- chronic diseases
- the body of young children and elderly people whose immune systems are very unstable

The fragile body of a small child is an excellent target for Staphylococcus aureus
Staphylococcus in the feces of an adult: discovered, photo, found and how to treat
Staphylococcus aureus is a very common and very dangerous opportunistic bacterium that can affect anyone, regardless of gender and age. These microorganisms are widespread in rooms where there are many people.
The source of infection is an infected adult or child. Pathogenic microorganisms are activated in those who have a sharp decrease in immunity or a deterioration in their general condition.
One of the most difficult types of staphylococcus is considered golden. It is this that causes various throat diseases. And if it multiplies excessively, a person can even get a purulent sore throat.
Despite the fact that the microorganism itself has been sufficiently studied, the staphylococcal infection it causes remains one of the most serious diseases in terms of treatment.
This interesting fact is due to the high variability of staphylococcus and its ability to quickly develop resistance to various antibiotics (especially if the patient does not comply with the dose, frequency of medication and duration of the course).
Staphylococcus aureus: what is it?
Staphylococcus aureus is a bacterium that resembles a ball in appearance. The disease is very common. According to data, 20% of the world's population are already direct carriers of staphylococcus.
It is found everywhere: on the skin, in the nose, in the intestines, throat and even on the genitals. This prevalence also affects the number of diseases that the bacterium can accompany and cause.
Among the main reasons contributing to the development of staphylococcal infection are:
- Presence of chronic diseases;
- Decreased immunity due to stress, vitamin deficiencies, taking antibiotics, poor nutrition and taking drugs that suppress the immune system;
- Interaction with a potential carrier of infection (for example, tonsillitis, which is transmitted by airborne droplets);
- Failure to comply with sanitary standards for cuts, abrasions, and open wounds on the body. Infection of a wound with staphylococcus can lead to its suppuration and ultimately lead to blood poisoning;
- Eating unwashed fruits, vegetables and other bacteria-contaminated foods.
Often, Staphylococcus aureus infection also affects children. The risk factors in this case are:
- Pathological pregnancy;
- Long anhydrous period during childbirth;
- Preeclampsia during pregnancy;
- Hypotrophy of the newborn;
- The birth of a premature baby;
- Failure to comply with the child's personal hygiene.
The biggest problem when fighting staph is that it has amazing vitality. Neither cold, nor direct sunlight, nor lack of moisture can affect this microorganism. Even practically dried staphylococcus bacteria retain their properties.
What is Staphylococcus epidermidis
Staphylococcus epidermidis is an infectious agent that causes inflammatory changes in various organs and tissues. It is characterized by damage to the skin and mucous membranes, which is accompanied by disruption of the functions of the human body.
Staphylococci are spherical bacteria that occur in pairs. Most often, a patient encounters an infection in a hospital setting.
Infection occurs through contact with the secretions of an affected person (blood, feces, saliva); there are cases of transmission of epidermal staphylococcus through the use of common personal hygiene products, dishes and other household appliances.
Factors that increase the likelihood of developing the disease:
- hypothermia;
- weak immunity;
- previous surgery or injury;
- course of radiation therapy;
- taking antibiotics and glucocorticosteroids.
How is Staphylococcus aureus transmitted?
In most cases, infection occurs in medical institutions. Staphylococcus aureus is transmitted both by airborne droplets and through food (contaminated meat, eggs, dairy products, cakes, cream pies) or household items.
The infection can also enter the child’s body through microtraumas of the skin or mucous membranes of the respiratory tract.
Premature babies and children with weakened immune systems are at greatest risk of infection. During childbirth, through wounds or scratches, or through breast milk, a mother can infect her baby.
If bacteria enter the mother's body through cracks in the nipples, this can lead to purulent mastitis in her.
Staphylococcus aureus in children and newborns
One of the toxins produced by Staphylococcus aureus, exfoliatin, has the property of severely affecting newborns. The released poison penetrates the pores of the skin and provokes the appearance of blisters, which are similar in appearance to burns and because of this are called “scalded baby” syndrome.
This disease rarely affects newborns since they are protected for 6 months by the immunity received from mother’s milk; in parallel, additional immunity is developed from the baby’s contact with bacteria, which continues to protect him. To prevent diseases in a child, it is necessary to carefully monitor his hygiene and nutrition.
How dangerous is this bacterium?
When the body's defenses are weakened, the infection awakens and causes various diseases, including blood poisoning or sepsis. The high pathogenicity of Staphylococcus aureus is associated with three factors.
- Firstly, the microorganism is highly resistant to antiseptics and environmental factors (withstands boiling for 10 minutes, drying, freezing, ethyl alcohol, hydrogen peroxide, with the exception of brilliant green).
- Secondly, Staphylococcus aureus produces the enzymes penicillinase and lidase, which makes it protected from almost all penicillin antibiotics and helps melt the skin, including sweat glands, and penetrate deep into the body.
- And thirdly, the microbe produces endotoxin, which leads to both food poisoning and a syndrome of general intoxication of the body, up to the development of infectious-toxic shock.
And, of course, it should be noted that there is no immunity to the disease, so an adult or child who managed to cure Staphylococcus aureus can become infected again.
Staphylococcus aureus on the skin, on the face
When the pathogen gets on the skin and, under a favorable environment, begins to actively reproduce and multiply, most of the epidermis (neck, armpits, buttocks, inner thighs) of the infected person becomes covered with purulent boils , causing unpleasant pain.
IMPORTANT: This skin inflammation may be accompanied by general weakness, fever, and increased temperature.

On the face, Staphylococcus aureus indicates its presence with acne and pimples.
IMPORTANT: Even with good general skin condition, staphylococcus will find a way to “show itself.” He can turn any, even the most harmless wound or scratch, into a huge inflamed purulent wound in a short time.

Purulent wound with Staphylococcus aureus
Staphylococcus aureus in milk
If it suddenly happens that staphylococcus is found in breast milk, the most important thing for a nursing mother is not to panic and not immediately stop breastfeeding her child.
However, you cannot ignore the symptoms either, since you can easily find yourself under the surgeon’s scalpel.
IMPORTANT: In this situation, you need to focus on the baby’s behavior: the baby eats, sleeps, poops regularly and normally, does not show obvious signs of anxiety, which means everything is fine and you need to continue feeding, since it is with breast milk that the baby receives the necessary antibodies to form his immune system systems.

If the child is restless and capricious, and the culture showed the presence of dysbacteriosis with a high concentration of staphylococcus bacteria, it is possible, without giving up breastfeeding, to treat the baby with a variety of bacteriophages.

An infant’s anxiety with a confirmed staphylococcus infection is a reason for treatment
What is staphylococcal bacteria
Staphylococcus aureus is a pathogenic microorganism that is one of the most common pathogens of infectious diseases worldwide. The bacterium got its name because of its golden hue, which can be seen under a microscope.
The most common infections with Staphylococcus aureus are:
- Premature or weakened babies born during difficult childbirth;
- Infants who are bottle-fed;
- In maternity hospitals and hospitals where certain hygiene conditions are not maintained;
- Babies whose mothers took antibiotics during pregnancy or suffered from acute viral infections.
Despite the fact that staphylococcus often enters the body, it can cause disease only under certain conditions (usually when the child’s body is weakened). Therefore, it is necessary to distinguish between situations when the presence of Staphylococcus aureus in the intestines and staphylococcal infection are detected. These are fundamentally different things.
There is no need to treat Staphylococcus aureus in a healthy child who has no complaints, since this microorganism is considered a normal inhabitant of the intestines. It is constantly present in approximately 80% of the population. It is found on the skin in 100% of the population.
Staphylococcus aureus treatment drugs and antibiotics
Since Staphylococcus aureus bacteria are uniquely resistant to antibiotics, it makes no sense to use them to treat diseases that are not accompanied by serious pathology, because their presence will only aggravate the condition of the infected person, in whose body dysbiosis is already progressing.
IMPORTANT: Staphylococcus bacteria are actively mutating, quickly adapting to new medical discoveries in the fight against this infection.

If the pathogen worked too actively and brought the body to sepsis, pneumonia, facial furunculitis, the use of antibiotics is not only justified, but necessary, since subsequent complications can even lead to death.
You can use drugs such as:
- methicillin
- oxacillin
- vancomycin
You can take antibiotics to treat Staphylococcus aureus only under the strict guidance of a doctor.
Drug for the treatment of Staphylococcus aureus
Bacterial lysates are often used to treat staphylococcal infections
- IRS 19
- imudon
- broncho-munal
- broncho waxing
They encourage the body to produce antibodies.

Broncho-Vaxom is used in the treatment of Staphylococcus aureus
No less popular is staphylococcal toxoid . As an option, you can use a staphylococcal vaccine, which is a solution for subcutaneous injection .
Bacteriophages occupy an important place in staphylococcal therapy .
IMPORTANT: There are many other drugs, but self-medication in this case is unacceptable; you need to contact a specialist who, after studying the test results and symptoms, will prescribe the correct treatment.
A scary tale about stool and staphylococcus in a child
Moderators, sorry if I put it in the wrong category! A very interesting article about baby stool, dysbacteriosis and staphylococcus.
A scary tale about staphylococcus. Returning to the same topic.
No matter how much I answer, no matter how much I say that the presence of staphylococcus and the clinical picture of staphylococcal infection are not the same thing, the flow of questions does not decrease. Many of our local doctors, either out of reluctance to look for the true cause, or because of ignorance of the concepts of microbiology, write off rashes, allergies, dermatitis, loose and/or green stools, constipation, diarrhea, hiccups, vomiting, sleep disorders, appetite, behavior, development ( Underline what is necessary from what is presented) - the mysterious and at the same time comprehensive diagnosis “DYSBACTERIOSIS”. And they begin to stuff the unfortunate little creatures with tons of drugs, ranging from probiotics to intestinal antiseptics. At best, there is no point; at worst, new misfortunes are added. And oh my god!!!! Staphylococcus was cultured in the stool!!!
Questions are immediately posted on the forum: “We have staphylococcus in our nose, throat, butt (choose the one you need)! what do we do!?". And mothers roll their eyes and twist their heads when I tell them, “so what? Nothing to do". You will ask why? Yes, because staphylococcus itself does not pose any danger to your baby. This is especially true for those children whose mothers are breastfeeding. I'll explain it popularly.
During intrauterine development, the gastrointestinal tract (GIT) of the fetus is sterile. There are no bacteria or other microorganisms there. When a baby is born, the gastrointestinal tract is colonized, or colonized, by bacteria that enter the baby's mouth as it passes through the mother's birth canal. The bacteria can also be passed on to the baby from the mother's stool during birth. This is how normal and healthy intestinal microflora is created. After birth, the baby’s gastrointestinal tract is colonized by bacteria that are found in the environment, in the mouth and on the mother’s skin. This happens during breastfeeding, when kissing and touching the baby.
Staphylococci are very common microbes, and we are introduced to them literally from birth. Staphylococci (especially S. epidermidis) are representatives of the normal microflora of the human skin, respiratory tract and digestive tract; they are also regularly found in the air and environment.
A healthy mother means a healthy baby. When the baby is born, bacteria begin to penetrate into the newborn’s body: into the intestines, stomach, and onto the skin. This is a normal process—the baby adapts to the environment. If the mother herself is healthy, pregnancy and childbirth went smoothly, then the baby’s flora will be normal. Accordingly, at the very first contact of a child with the environment, his body (including the intestines and nasopharynx - from where they are later sown by comrades who especially want to be treated) begins to get acquainted with this microbe. Accordingly, the immune system produces antibodies that prevent the proliferation of staphylococcus and inhibits its activation. And if the child is an infant, then he is doubly protected, because the antibodies that the mother has developed rush to the aid of her own antibodies and pass on to the baby with her milk. This begs the conclusion, huh??? The best way to combat and prevent staphylococcal infections is breastfeeding. In principle, artificial ones can calmly coexist with staphylococci, provided they have properly organized nutrition and care. Because the child’s immune system begins to work from birth and constantly fights all opportunistic microbes.
So they live peacefully and amicably - staphylococcus and the body - and will continue to live if they are not disturbed with their supposedly therapeutic measures and picking in the poop of an absolutely normal child.
They treat the staph infection, not the staph infection (in particular). It is very (!) important that you should always distinguish between concepts such as staphylococcus and staphylococcal infection (we will discuss it at the end of my story). Detection of staphylococcus in the absence of real symptoms of the disease is not at all a reason to immediately swallow medications.
My dear parents - staphylococcal infection is very different in the clinic from what you treat. The presence of a piece of paper with staphylococci written on it to some extent and green poop in a baby’s diaper is not a reason for active hostilities. There are many factors influencing a baby’s stool and its changes.
Many microorganisms (including Staphylococcus aureus) normally live in various parts of the human body (including a small child). These are the intestines, skin, mouth, nose, pharynx, ears, mucous membranes of the eyes. And they do not cause infections. They are called normal microflora. But if placed in inappropriate conditions, they can cause disease. Staphylococcus, for example, getting into a wound, can cause suppuration. Therefore, these microorganisms are called opportunistic. These microbes do not normally cause harm, since they live in a community of other microorganisms and there they all mutually restrain each other.
Staphylococcus in stool? Do not panic!
Staphylococcus in the intestines is normal if there are no clinical alarming manifestations (fever, ulcers on the skin, bloody stools). The baby suckles well, has normal bowel movements, and gains weight well, in which case there is no need to interfere with the natural process! The individual level of gastrointestinal flora is different for each person.
Carriage of staphylococcus is a completely common occurrence and is not an indication for any treatment. Cultures from the mucous membrane of the nose and pharynx with subsequent determination of the sensitivity of microflora to antibiotics most often lead to the unreasonable prescription of antibiotics and other drugs. Sanitation for carriage of Staphylococcus aureus is not indicated.
Carriage of staphylococcus on the mucous membranes cannot cause fever, headaches, nausea and vomiting, constipation, bloating and colic, and, accordingly, a crying child. Therefore, you need to look for the cause, and not treat the unfortunate, innocent staphylococcus.
What then is considered normal stool? There are such horrors in diapers!!!
So let’s look at your main horrors (although I have already devoted an entire article to stool standards, “Child’s stool.” But apparently not everyone has read it.
So I’ll explain it popularly.
A breastfeeding child has the right to any chair. This means that the color of poop should be the last thing the mother worries about if the baby is calm, cheerful, develops and grows normally, and gains more than 500 g in weight in the first months.
By the way, the stool of an infant changes greatly in the first months of life (please note that for now we are only talking about the stool of a child who is completely on breastfeeding. On the breastfeeding, and even more so on IV, everything is different, because even supplementing with water can affect the stool) .
From birth to 2-3 days, meconium (original feces), thick, black-green, is released 2 to 4 times a day. But this usually happens in the maternity hospital and mothers do not worry about this - they are not yet in the mood for digging in the baby’s poop, and the euphoria of giving birth and meeting the long-awaited child has not yet passed (well, at least that’s how it was for me!).
In the first three days after birth, the number of bowel movements should correspond to the age of the child - on the first day the child should have one bowel movement, on the second day - two, on the third - three. After the milk comes in, the infant has bowel movements at least 3-4 times a day, and the amount of stool is quite significant. Most infants have bowel movements much more frequently, often after each feeding. Even an inexperienced mother can easily recognize the joyful volley of a baby going to the toilet - it is impossible not to hear and miss it.
From 2-3 days to 4-6 weeks, the child can walk more than 4 times a day, each time - a little more than a spoon, usually the consistency is soft or liquid, mustard color, the smell is usually sweet, milky, but can be sour, inclusions of curdled milk are possible , which indicates that the baby is getting enough milk. And even with an excess, which is removed in the form of curdled crumbs. Farting with water and heterogeneity in the poop itself are allowed.
As they grow older, around 6 weeks of birth or a little earlier, many infants switch to a more infrequent bowel movement - from once every few days to once a week or even less often. In this case, there are no signs of constipation (that is, dry, hard stools) - the child’s stool is still unformed and puree-like. Therefore, there is no need to go to the child with enemas and other means of “help”.
It is typical that newborns and infants excrete unchanged bilirubin with feces, and therefore the stool has a characteristic greenish color. Typically, the color changes when bilirubin comes into contact with air. That is, the baby pooped, and you didn’t change the diaper right away, but after a little time - then you’ll get romantic green (which horrifies many mothers) poop. If they don’t bother your child – and most often this is the case – calmly throw away the diaper and forget about it.
The reaction to bilirubin remains positive until 4-5 months of age, then, in parallel with bilirubin, stercobilin begins to be detected (it gives feces their color) as a result of the restorative effect of the normal bacterial flora of the colon. By 6-8 months of age, only stercobilin is detected in the feces - therefore, by this time, the greens with the staphylococci supposedly present in them usually disappear. And, lo and behold, my mother rejoices - we cured dysbiosis, but it didn’t exist, these are just age norms.
Green stool with foam or mucus - may be associated with changes in weather, active colonization of intestinal flora in the first weeks of life, mother's illness, mother's diet. This is not always a pathology and you should not immediately run for tests.
And foamy stools, it turns out, indicate fermentation dispersion associated with excessive consumption of carbohydrates (sugar, honey, flour products, fruits, grapes, peas, beans, cabbage, etc.), but the baby only drinks breast milk, which means that foamy stools are related to the mother’s diet and the mother needs to remove these particular foods from her diet.
The second type of foamy stool is an imbalance of foremilk and hindmilk. If your baby only receives lactose-rich foremilk, his stool may become foamy. This occurs because in the first weeks of life there is a relative lack of the enzyme lactase, which breaks down lactose (milk sugar). If there is an excess of milk sugar (when feeding on foremilk), there is not enough lactase to break down, and the sugar enters the large intestine, where it is broken down by intestinal bacteria with the formation of excess gases - therefore foam is obtained. And staphylococci and Klebsiella have nothing to do with it.
After the mother has established active lactation, the baby has “mature” stools, which will remain until complementary feeding or supplementary feeding is introduced. It is a homogeneous yellow pulp with the consistency of thin sour cream with the smell of sour milk. Such stool indicates good digestion of mother's milk. As for the normal frequency of stool, most newborns have a bowel movement almost after every feeding, that is, the number of bowel movements per day can reach 5-8, and sometimes even 10.
As a variant of the norm, a condition is considered when mother's milk is so completely digested that practically nothing remains in the intestines, and bowel movements can occur once every few days, sometimes even once a week. Such a condition can be considered normal against the background of full breastfeeding (exclusively, even water is not given, and plantexes, grass-ants too) and provided that the baby is in good health (normal behavior, absence of abdominal pain and significant straining during bowel movements). As a rule, this feature develops in some infants no earlier than 3 months of life.
By the way, a baby is quite capable of pushing, kicking his legs, grunting, blushing and even crying during defecation and this is not a pathology (well, unless, of course, his stools are like nuts or goat poop). Just the act of defecation for a baby is also work, he spends effort on it. To poop a baby, you need to create a certain pressure in the lumen of the rectum. And only this will contribute to the relaxation of the anus muscles and the victorious volley! And when the baby strains, there is no need to grab him along with the poop and rush to hand it over. This is normal behavior!
Lure. Introducing any food other than breast milk will cause changes in the consistency, color and odor of the infant's stool. If you have started introducing complementary foods, your stool will begin to become more formed and you will notice bits of food in your stool that you give to your baby. And by the way, the color also depends on what kind of food the child eats - in principle, what is eaten is what comes out. It’s too early to say until the baby’s food is completely digested. So the puree introduced by mom may come out in an almost unchanged pile, and this is not scary.
By the way, the norms of breastfed children differ significantly from those of mixed and bottle-fed children. For example, the intestinal flora of a bottle-fed baby at 2 weeks is almost no different from that of an adult. Formula-fed children have less frequent bowel movements, as well as more formed stools with a noticeable, typical odor.
With artificial feeding, the stool may be the same as with natural feeding, or have a thicker consistency and a darker, brownish color. Defecation must occur at least once a day (well, maximum once every two days), everything else is considered constipation. The number of bowel movements during the first half of the year is usually 3-4 times a day, and in the second half of the year - 1-2 times a day. The amount of feces is 30-40 g per day. With artificial and mixed feeding, due to the predominance of putrefaction processes in the feces, there is a lot of E. coli, fermentative flora (bifidoflora, lactic acid bacilli) is present in smaller quantities. A small amount of mucus should not be given any importance, as well as small whitish crumbs, which only indicate that the milk contains excess fat that the child does not have time to digest.
Diaper contents to pay attention to.
Deviations from the norm in the frequency and appearance of stools do not always mean that the child is necessarily sick with something. However, a baby's stool can be a useful sign of adequate nutrition or a symptom of an allergy. In such cases, changing the feeding method or eliminating the allergen is all that is required to solve the problem.
Frequent, watery, green and/or foamy stools and mucus may be a sign of malnutrition. Often such stool occurs in combination with slow weight gain. This condition is sometimes called foremilk and hindmilk imbalance. The baby sucks a lot of low-fat foremilk, which passes through the digestive system too quickly and causes the above symptoms. This is usually easily resolved by changing behavior during feedings, namely increasing the duration of sucking on one breast. This allows the baby to suckle on the fatty hindmilk, which is digested more slowly.
If your baby constantly has green and watery stools, this may be a sign of an allergy. In addition, the child may have vomiting, mucus or blood in the stool, as well as irritability and skin rashes. In this case, it is especially important to continue breastfeeding, because... Weaning is associated with an increased risk of allergies.
If your baby soils more than 12-16 diapers per day, and the stool smells bad and is watery, this is diarrhea. Usually, diarrhea in infants quickly goes away on its own and without any complications. The cause of diarrhea can be infection, treatment with antibiotics, introduction of complementary foods, or excessive consumption of fruit juices. In case of acute diarrhea or diarrhea while taking antibiotics, the child should be breastfed as much as possible. Breast milk contains everything needed to prevent dehydration, as well as antibodies that help the baby cope with infection, and also factors that help restore normal intestinal flora. If the cause of diarrhea was the introduction of complementary foods or juices, you may need to postpone the introduction of complementary foods for some time.
Well, I’m returning again to our favorite topic - dysbiosis! Familiar word? A Russian parent who has not heard it from his pediatrician can send his portrait to the “Happiest Parent of the Year” competition. A terrible illness that has affected all our children, has reached adults, is painful and indecent, but can be easily cured by regularly eating something, drinking something in the morning, in general, by regularly transferring money to someone’s account, has come into our world.
Faced with the most enormous deception of modern pediatrics, I consider it my duty to dot the i's so as not to repeat the same thing countless times in every second forum topic.
It is difficult to identify the symptoms of dysbiosis, or rather impossible to say, since this condition is not a disease
according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), a document of the World Health Organization that is the generally accepted international diagnostic classification in healthcare. That is, in the world, and in Russia, by the way, too (we, pediatricians, use ICD-10 to make diagnoses, like all doctors in the world), such a condition does not exist. But why then are they persistently treating him? How can you treat something that doesn't exist?
Typically, the indication for testing for dysbacteriosis is diarrhea that does not go away within two or three days. In adults and bottle-fed children, diarrhea is defined as frequent and loose stools. As mentioned above, for infants, frequent, unformed, loose stools are normal, and therefore cannot be an indication for testing. Other symptoms that serve as a reason for laboratory tests for dysbacteriosis may include greenish stools, stools with mucus, constipation (rare stools in infants are often mistaken for constipation), foamy stools, and particles of undigested food. All these symptoms in older age actually accompany diarrhea, which is often caused by pathogenic bacteria and requires treatment with antibiotics. In children under one year old, each of the listed signs may be a variation of the norm.
So, what you need to know about intestinal dysbiosis:
1. The main thing is that dysbiosis... does not exist! There is no disease or condition that could be related to the concept, no need to look for it, no need to treat it. Read more…
2. The lumen of the intestinal tube in a born child is sterile (just as the child himself is sterile). Within a short period of time, it, as it communicates with the external environment, is colonized by microorganisms that live in it throughout a person’s life.
3. These microorganisms can be beneficial, taking part in the digestive process; neutral, of which the majority (they live and live - someone must live in the intestinal lumen) and harmful, causing intestinal diseases.
4. The number of microorganisms in the intestines, as well as their ratio, is different for each person and depends on countless factors - whether a person lives in a city or a village, what he eats, how carefully he observes the rules of hygiene, whether he is healthy or sick at the moment, and etc. There are no uniform standards for the content of microbes in the intestinal lumen. This is the first thing you need to understand. A person has the right to an individual microflora.
5. The lack of standards and large-scale research in this direction is primarily due to the fact that such research is not needed by clinical medicine and does not carry any meaning! Nothing depends on the number and composition of microbial colonies. And this is the second conclusion of our conversation.
6. Next, one should distinguish between the content of microorganisms in feces - in the intestinal lumen (which other doctors are so actively studying) and their content in the intestines themselves, i.e. on the intestinal wall - where they may have at least some hypothetical significance. There is no convincing evidence that the number of microorganisms in the stool in any way corresponds to their ratio in the intestine. Thus, what we define is absolutely unclear. Let’s remember the third rule: “No, there has not been and cannot be an analysis for dysbacteriosis.” Any study that you are offered to undergo in this regard is meaningless, uninformative and aimed only at simulating treatment.
So why is this same dysbacteriosis not treated only by the lazy?!!!
But there is no answer to this question. Partly because it is easiest to treat a non-existent disease - what did not exist will definitely pass. Partly because for some colleagues, reading an advertising brochure from another manufacturer is easier than reading a serious textbook (it also costs money, and is often written in English)... In some cases, because it is easier to attribute incomprehensible symptoms to some mythical but well-known problem - after all, what we are writing today does not exclude the existence of many diseases of the gastrointestinal tract, each of which has its own clinic, its own set of tests and its own treatment. But these are diseases. Healthy children do not need to be treated.
The level of deception has reached the point that in addition to meaningless medicines to treat a non-existent disease, we are even offered to buy food!!! “Buy from us constantly and you will not have dysbacteriosis!!!” We hope that after reading these words, you will always be skeptical of such advertising, no matter how convincing it is.
What about antibiotics? Why, then, when taking them does the stomach often become upset?
A routine mistake, however, and a common honest misconception is the opinion that when antibiotics are prescribed, a disturbance in the microbial balance in the large intestine necessarily occurs. As a rule, and in most cases, the use of antibiotics does not entail any disorders and does not require additional correction of the microbial balance.
But. For some drugs, temporary diarrhea is a side effect of use. For example, the popular antibiotic amoxiclav causes diarrhea in approximately 7-10% of cases. Thus, a temporary increase in frequency and thinning of stools should be considered not as an independent problem requiring correction, but as one of the effects of the drug.
So how can you support your child’s body? What actions should I take? Maybe among the hundreds of products that are offered to us, there is something really useful?.. So that only beneficial microbes live in my child’s intestines???
There is no need to do anything, absolutely nothing extraordinary. Feed your children tasty and varied food. Teach them to wash fruits and hands before eating. Teach basic hygiene rules and consider that your mission is completed.
How indicative are tests for dysbacteriosis in healthy infants? The study of the composition of the intestinal flora in a healthy infant, that is, a child without visible symptoms of a disease, in this case diarrhea, is of interest to scientists, but not to parents or medical practitioners. Numerous studies have shown that breast milk protects children from disease, even if the intestines are colonized by pathogens. For example, breast milk contains antibodies and factors against E. coli, Vibrio cholerae, Salmonella, Staphylococcus, Klebsiella, Shigella, rotavirus and Giardia. This means that a pathological microorganism can be sown in the stool, but the child does not show any symptoms of the disease.
And again I will return to staphylococcus. We figured out when it doesn't need to be treated. When there is an analysis (a piece of paper with a certain number of microbial CFU 10 to some extent) and the child does not make any complaints.
Another thing is a staphylococcal infection. And you need to know about it too.
Pathogenic staphylococcus has been a problem in maternity hospitals for centuries. In maternity hospitals there is a strict sanitary and epidemiological regime, almost everything is regularly wiped with disinfectants, killing all microflora on surfaces (pathogenic and non-pathogenic, indiscriminately). The first to quickly occupy the “vacant apartment” is Staphylococcus aureus (spreading from the skin and mucous membranes of people). And since there is no competition for him there (they are still killed), he begins to multiply uncontrollably and then, through the air or hands, gets to both women and newborn children.
Newborn children, not having time to be colonized by the normal human microflora of the mother’s skin, including her Staphylococcus aureus in the company of other microorganisms (which is ensured by early attachment and staying together), are affected by hospital-acquired Staphylococcus aureus, which causes various diseases (mainly skin, but sometimes which is more serious). They haven’t yet had time to develop antibodies against it. But mom didn’t have time to pass them along with the milk.
A woman with a bleeding uterus and breast milk after childbirth (this is an excellent environment for the proliferation of microbes) also has a risk of getting a hospital infection.
This happens all over the world.
STAPHYLOCOCCAL INFECTION. Staphylococcal diseases primarily affect young children or children weakened by other diseases.
The clinical course of staphylococcal infection is characterized by diversity - from the most severe, generalized forms to mild ones: sepsis, pneumonia, meningitis, abscesses of internal organs, enterocolitis, endocarditis, gynecological diseases, staphylococcal infection with scarlet-like syndrome, purulent-inflammatory diseases of the skin and soft tissues, etc. Moreover, note about green stools with farts, constipation and other treatment problems - there are no words here. Staphylococcal infection, if present, is a serious disease. And most often it is treated inpatiently with massive antibiotics, and not with bacteriophages, enemas and all sorts of biological preparations.
The main activities that are being carried out around the world to reduce risk:
— maternity hospitals should not be too closed from visitors and should not excessively disinfect surfaces so that the normal microflora of the surrounding world is preserved there, and not hospital staphylococcus.
- early attachment and stay with the mother.
- a short period of stay for the mother and child in the maternity hospital after a normal birth (a couple of days - and then go home to the usual microflora), so that there is less risk of contamination with hospital microflora.
— standard infection control measures.
Your child has Staphylococcus aureus in his intestines, like all other people on earth. In general, many people live normally in their intestines. It may also be the causative agent of tetanus. And this is also the norm.
Staphylococcus aureus: alternative treatment
Some people prefer to use “recipes from grandma’s notebook” instead of traditional treatment. Here are a few recipes for effective remedies, according to users:
Recipe No. 1: Grind the roots of parsley and celery in a 2:1 ratio and squeeze out the juice, drinking it in the morning on an empty stomach 40 minutes before meals.

Parsley root against Staphylococcus aureus
Recipe No. 2: 300 g of cranberries are mixed with 150 g of uncandied honey, ½ of the resulting mass is eaten in the morning half an hour before meals, the rest is consumed during the day between meals. This procedure must be carried out for at least a month.

Cranberries will defeat Staphylococcus aureus
Recipe No. 3: Progressive furunculosis can be cured as follows: pour 100 g of crushed garlic into 300 ml of warm water, leave for two hours, strain, soak a gauze swab in the resulting liquid and apply to the site of infection twice a day for two weeks.

Garlic helps get rid of furunculosis with Staphylococcus aureus
Recipe No. 4: You can use this “panacea” for all manifestations of staphylococcal infection: a universal herbal mixture. For this, yarrow (0.3 kg), lupine and burdock leaves (0.25 kg each), nettle, plantain, oregano, St. John's wort, sweet clover, coltsfoot (0.15 kg each), cinquefoil roots and rose hips ( 0.1 kg each), calendula flowers, chamomile, dandelion roots and horsetail (0.05 kg each) are thoroughly mixed and half a glass of this mixture of herbs is poured into a liter of water and boiled for no more than 5 minutes. Then leave for 1 hour, filter and take half a glass every hour for the first two days before meals. The following days, the decoction is taken in the same dosage 4 times a day for two months.

Nettle against Staphylococcus aureus
Diseases caused by Staphylococcus aureus
What diseases can a person get if Staphylococcus aureus keeps pace with him?
Among the most common:
- Various diseases of both the upper layer of skin and subcutaneous tissue
- Inflammation of the respiratory tract , manifested as sore throat and pneumonia
- Diseases of the nasal and oral mucosa, otitis, conjunctivitis
- Pathology of the nervous system , smoothly turning into meningitis
- Disorders of the digestive and gastrointestinal tract
- Inflammations of the genitourinary system: cystitis, urethritis

The main thing, if you suspect a staphylococcal infection, is not to remain indifferent to your health, do not self-medicate, but seek help from a specialist.
The danger of staphylococcal dysbiosis
Staphylococcus aureus is the most dangerous microorganism for humans. An intestinal infectious agent can provoke further development of sepsis. The bacterium actively spreads in the blood and affects vital organs. Acute forms of inflammatory processes develop:
In the colon of a healthy person, the microorganisms that form the basis of the microflora are represented by anaerobes: bifidobacteria and lactobacilli, as well as aerobes - Escherichia coli (E. coli) with normal enzymatic properties. These microorganisms ensure the stability of normal microflora and prevent the colonization of the large intestine by foreign microorganisms.
Opportunistic microorganisms that live in the intestines, representatives of the Enterobacteriaceae family: Klebsiella, Enterobacter, Proteus, Citrobacter, Pseudomonas aeruginosa, Staphylococcus, etc., make up a significant part of the normal aerobic (needing an oxygen supply for development) intestinal flora and usually do not cause diseases, but on the contrary, they participate in ensuring its normal functioning. But when their quantity exceeds the norm, it can cause intestinal disorders.
Composition of intestinal microflora in healthy children (fu/g feces)
| Microflora | Normal in children | |
| Less than a year old | Over a year old | |
| Pathogenic enterobacteria | 0 | 0 |
| Total E. coli count | 300 - 400 million/year | 400 -1 billion/year |
| Escherichia coli with normal enzymatic activity. | 10 7 –10 8 | 10 7 –10 8 |
| Escherichia coli with weak enzymatic properties | 10 –10 11 | 10 9 –10 10 |
| Lactobacilli | 10 6 –10 7 | 10 7 –10 8 |
| Bacteroides | 10 7 –10 8 | 10 9 –10 10 |
| Enterococci | 10 5 –10 7 | 10 5 –10 8 |
| Eubacteria | 10 6 –10 7 | 10 9 –10 10 |
| Peptostreptococci | 5 | 10 9 –10 10 |
| Clostridia | 3 | 5 |
| Staphylococcus aureus (S. aureus) | 0 | 0 |
| Staphylococcus (saprophytic epidermal) | 4 | 4 |
| Yeast-like fungi of the genus Candida | 3 | 4 |
| Other opportunistic enterobacteriaceae | ||
| Klebsiella | 4 | 4 |
| Enterobacter | 4 | 4 |
| Graphnia (Hafnia) | 4 | 4 |
| Serratia | 4 | 4 |
| Proteus | 4 | 4 |
| Morganella | 4 | 4 |
| Providecia | 4 | 4 |
| Citrobacter | 4 | 4 |
| Non-fermenting bacteria | ||
| Pseudomonas | 3 | 4 |
| Acinetobacter | 3 | 4 |
Pathogenic enterobacteria are the cause of a large number of different human diseases. These include bacteria that cause acute intestinal infection (AI): salmonella, shigella - the causative agents of dysentery. The detection of these microorganisms is an indicator of a serious intestinal infection. Escherichia coli (Escherichia coli, abbreviated e. coli) is part of the normal microflora of the human gastrointestinal tract.
A decrease in the total amount of E. coli may be a sign of the presence of parasites such as worms in the intestines.
E. coli with reduced enzymatic activity is an inferior E. coli, which does no harm or benefit. However, the presence of an indicator higher than normal is a sign of incipient dysbiosis.
In the feces of a healthy child, E. coli (typical) are detected in an amount of 10 7 -10 8 CFU/g, while the number of lactose-negative E. coli should not exceed 10 5 CFU/g, and hemolytic (hemolyzing) E. coli should be absent.
Hemolytic (hemolyzing) E. coli are capable of producing toxins that act on the nervous system and intestines, can cause allergic and intestinal problems, but should normally be absent
Lactose-negative enterobacteria are a group of opportunistic bacteria that interfere with normal digestion and cause dyspeptic symptoms in a child, that is, heartburn, belching, a feeling of pressure or bloating in the abdomen. Their number should not exceed 5% (or in titers: 10 4 – 10 5 – moderate increase).
Lactobacilli are one of the most important in the group of lactic acid bacteria; they break down lactose (milk sugar) and prevent the development of lactase deficiency, maintaining the acidity of the colon at a level of 5.5–5.6 pH. Lactobacilli activate phagocytosis (a process in which special cells of the blood and body tissues (phagocytes) capture and digest pathogens of infectious diseases and dead cells). Lactobacilli are part of mother's milk.
Bifidobacteria are the most important representative of the microflora of the human body; In the colon of children, they make up about 95% of the bacterial population. Bifidobacteria inhibit the growth of pathogenic bacteria, inhibit their growth and reproduction, so deficiency of bifidobacteria is one of the pathogenetic factors of long-term intestinal disorders in children. Various strains of bifidobacteria and bacteroides appear in the gastrointestinal tract 10 days after birth. Babies born by caesarean section have significantly lower bacteria levels than those born naturally. A significant decrease in the number of bifidobacteria is a sign of severe dysbacteriosis.
Enterococci are part of the normal microflora of the human gastrointestinal tract, but they are also causative agents of urinary tract infections and infections of the pelvic organs. In case of excessive growth of enterococci, the use of bacteriophages is recommended. Enterococci are present in the intestines in quantities of 10 5 – 10 8 CFU/g of feces and normally should not exceed the total number of E. coli.
Clostridia are part of the normal flora of the gastrointestinal tract.
Proteus is a representative of normal, opportunistic intestinal microflora. Proteas are considered sanitary indicator bacteria. The number of detected proteas is considered an indicator of contamination. The modes of transmission are nosocomial infection, as well as infection due to non-compliance with personal hygiene rules.
Klebsiella is an opportunistic bacterium of the Enterobacteriaceae family, which is part of the normal microflora of the gastrointestinal tract, but can cause a number of gastroenterological diseases. Klebsiellosis is one of the common nosocomial infections. At high titers, treatment is carried out with bacteriophages.
Citrobacter, Enterobacter, Proteus, Klebsiella and others, with a decrease in the body's immunity, can lead to changes in intestinal function and the formation of inflammatory processes in various organs.
Bacteroides are opportunistic bacteria, representatives of the normal human microflora. Colonization of the intestine by bacteroids occurs gradually. They are usually not recorded in fecal bacterial maps in children in the first six months of life; in children aged from 7 months to 1 - 2 years, the content of bacteroids does not exceed 10 8 CFU/g. The role of bacteroids is not fully understood, but it has been established that they take part in digestion, break down bile acids, and participate in lipid metabolism.
Staphylococci - non-hemolytic (epidermal, saprophytic) - are part of the group of saprophytic microflora that enter the body from environmental objects. Their quantity should not exceed 10 4 CFU/g of feces.
Staphylococcus aureus can be transmitted to infants through breast milk. Even small amounts of it can cause pronounced clinical manifestations (severe diarrhea, vomiting, abdominal pain), especially in children in the first months of life. Therefore, the standards given in the analysis form indicate that it should not exist. The pathogenicity of Staphylococcus aureus directly depends on the state of the normal flora: the more bifidobacteria, lactobacilli and normal Escherichia coli, the less harm from staphylococcus.
The clinical picture of intestinal dysbiosis caused by staphylococcus includes symptoms associated with intoxication and the inflammatory process developing in the intestines: fever (up to 39 ° C) with chills and sweating, headache, weakness, poor appetite, sleep disturbance, constant or cramping abdominal pain, loose, profuse stools with blood and mucus. The frequency of stools is up to 7–10 times a day. Abdominal bloating, prolonged pain along the large intestine, and spasm are recorded. Changes in the blood are characterized by an increase in the number of leukocytes, a shift in the leukocyte formula to the left and an increase in ESR, a decrease in albumin and an increase in globulin fractions, and in severe cases - a decrease in the content of total protein (up to 6.1 g/l).
Yeast-like fungi of the genus Candida - an increase in titers may occur after the use of antibiotics. If the number of fungi is increased, and the amount of normal intestinal flora is sharply reduced, and candidiasis (thrush) of the visible mucous membranes (oral cavity, genitals) is noted - these are manifestations of systemic candidiasis, that is, there is an infection with intestinal fungi.
When yeast-like fungi of the genus Candida are detected in crops up to 10 7 CFU/g of feces, the situation is assessed as intestinal dysbiosis. If more than 10 7 CFU/g of feces is detected in cultures and the clinical picture indicates a generalization of the process (damage to the skin, mucous membranes and internal organs), such cases are considered as candidomycosis or candidomycosis sepsis.
With candidomycosis in children, the pain is localized in the navel area, and there is a feeling of bloating and heaviness in the abdomen. The stool is liquid or pasty with mucus, sometimes with blood or foam, with the presence of whitish-gray or grayish-green mycotic lumps or films up to 6 times or more per day.
Dysbacteriosis is a common disorder of the gastrointestinal tract, which is associated with disturbances of the normal intestinal microflora. This condition may be a consequence of the appearance of pathogenic microorganisms or the activation of opportunistic bacteria.
The second category of disease is currently considered more dangerous. For example, staphylococcus is dangerous due to the fact that it is present in the body of almost every person and most often has some antibiotic resistance. For these reasons, sometimes the treatment of this class of dysbiosis can be delayed for many months.