Acute intestinal colitis can create a serious imbalance in the normal life of any person. With a timely approach, the pathology is completely cured. However, for this you must follow your doctor's recommendations.
Acute colitis affects the large intestine and disrupts the functions of the organ. Pathology can develop at any age. Most often, men and women aged 15 to 40 suffer from colitis. The second peak of possible infection occurs between 60 and 80 years of age. The disease affects men and women with equal frequency.
Most often the disease is infectious. However, it is possible to develop colitis while taking medications. The disease is highly treatable. With timely treatment, the patient recovers completely. In rare cases, intestinal pathology can become chronic.
Symptoms of bowel disease
Colitis is accompanied by a feeling of severe discomfort and pain. This disease is difficult to ignore. Sometimes it brings significant disruption to a person’s usual way of life. It prevents you from fully working and resting. It is severe pain in the intestinal area that becomes the main reason for visiting a doctor.
The disease always begins quickly. Severe pain appears in the lower abdomen. Most often they are localized in the left lower abdomen. The pain is cramping in nature. They may appear and disappear. Particularly severe pain is observed with the urge to defecate.
Following the pain, the patient has problems with stool. Fecal masses acquire a liquid consistency. In this case, the urge to defecate may occur more than 6 times a day. In severe cases, attacks of diarrhea can bother a person up to 20 or more times a day. Often the urge occurs at night.
Stool in acute colitis has a specific appearance:
- it becomes thin and watery. This indicates a violation of water absorption functions;
- admixtures of mucus and blood may be observed in the masses;
- feces acquire a foul odor.
In addition to the above, colitis may be accompanied by a number of additional symptoms:
- nausea;
- vomiting;
- increased gas formation;
- bloating;
- weakness;
- drowsiness;
- digestive problems;
- increased body temperature;
- dehydration;
- headaches;
- coating on the tongue;
- joint pain.
Photo: UV70 / Shutterstock.com
When making a diagnosis, it is very important not to confuse colitis with similar pathologies.
That is why patients are prescribed additional examinations. This may include taking tests and undergoing an ultrasound.
What is diversion colitis
Full text of the article:
Diversionary
[Oe1]
colitis
M.S. Anikina, endoscopist, GBUZ NSO "State Novosibirsk Regional Clinical Hospital", Novosibirsk, 2018
Annotation.
In the disconnected segments of the colon after surgical interventions with the application of various types of stomas, nonspecific inflammation develops, which is called diversion colitis, or colitis of the disconnected colon. Performing colonoscopy in this group of patients is an integral part of the routine practice of the endoscopist. The review examines issues of epidemiology, pathogenesis, endoscopic semiotics of diversion colitis, as well as preparation for colonoscopy of patients who have undergone surgery on the colon and rectum.
Introduction.
Today, multi-stage interventions are widely used in surgical practice, which improve immediate treatment results and lead to a reduction in the number of complications and postoperative mortality. Indications for such interventions may include malignant neoplasms, diverticular disease, abnormalities of the colon, and others. However, as a result of a colostomy or ileostomy, nonspecific inflammation develops in the disconnected segments of the colon, called diversion colitis, or colitis of the disconnected colon [1]. This pathological condition was first described by V. Morson in 1974, but the term “diversion colitis” was introduced by D. Glotzer in 1981 [1, 3, 8, 9].
Epidemiology.
The prevalence of diversion colitis in ostomy patients is extremely high and amounts to 74–91% [1, 3, 9]. Patients with pre-existing chronic inflammatory bowel disease (CIBD) are thought to have a higher incidence of diversion colitis, but in Son et al's study of diversion colitis in patients undergoing surgery for rectal cancer, the incidence was 100% [7, 8]. ]. There is no connection between diversion colitis, age, gender, type of stoma or method of surgical intervention performed [3, 9].
Pathogenesis.
The underlying mechanisms underlying diversion colitis are still not fully understood. The main link in the pathogenesis of this disease is a bacterial imbalance that develops as a result of disruption of the normal passage of feces, which leads to disruption of the protective function of the mucous membrane and a decrease in the amount of short-chain fatty acids (SCFA). SCFAs are involved in the metabolism of colonocytes, covering about 70% of their energy needs, and the lack of these acids leads to disruption of energy metabolism in the colon epithelium [1]. On the other hand, SCFAs relax vascular smooth muscle - and their deficiency can cause an increase in vascular tone, which leads to relative ischemia of the mucosa and wall of the colon (ischemic theory) [9]. The main theories of the pathogenesis of diversion colitis are presented in Fig. 1.
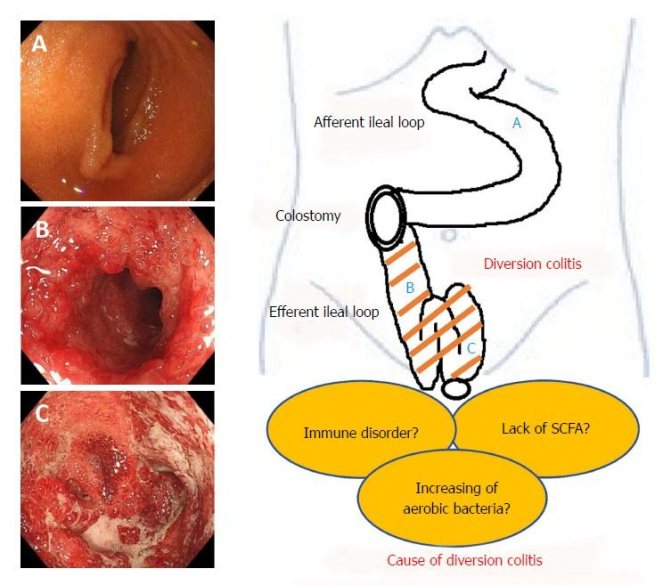
Rice. 1.
Basic theories of the pathogenesis of diversion colitis [9].
Clinical picture.
Clinical manifestations occur in approximately 30% of patients without CIBD, but in patients with Crohn's disease they occur in 33% of cases, and in ulcerative colitis - 87%. [Oe2] Symptoms of diversion colitis occur within 1–36 months after colostomy [3, 9]. Patients with diversion colitis complain of mucus and/or blood discharge, tenesmus, abdominal pain, a feeling of heaviness or pain in the rectum [1, 7]. Pathological discharge from the rectum is the most common symptom (40%), followed by abdominal pain and tenesmus (15%) [9]. The most informative diagnostic method in this case is sigmoidoscopy and colonoscopy with histological examination of mucosal biopsy and removed surgical specimens from disconnected sections of the colon and rectum [1].
Endoscopic picture.
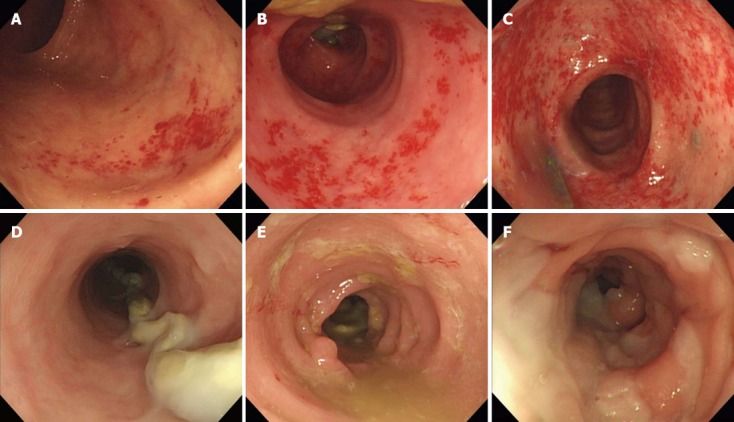
Macroscopic changes in the disconnected colon can be either continuous or segmental [9]. Diversion colitis is represented by edema, granulation, petechial hemorrhages, contact bleeding of the mucosa, blurred vascular pattern and resembles the endoscopic picture of ulcerative colitis with a moderate degree of activity [1].
Mucus deposits are noted at the walls. Son et al. in their work assessed the severity of edema (0–3 points), intramucosal hemorrhages (0–3 points) and contact bleeding (0–1 point) based on the endoscopic picture separately. The scores were subsequently summed (0–7 points). According to the total score, diversion colitis was divided into mild (0–2 points), moderate (3–5 points) and severe (6–7 points) (Fig. 2) [8].
Figure 2.
Endoscopic manifestations of diversion colitis [8].
An example of the main endoscopic findings in diversion colitis depending on the relative severity.
A, B, C.
Petechial hemorrhages (A - 1 point; B - 2 points; C - 3 points).
D, E, F.
Edema (D - 1 point; E - 2 points; F - 3 points).
Preparation for colonoscopy of patients who have undergone colon surgery.
I found a small number of resources devoted to the problem of preparing this group of patients. In the domestic literature, this problem is covered extremely poorly.
For patients with unloading ileostomies, oral bowel cleansing medications are not indicated. Such patients undergo colonic lavage through an ileostomy, which can be supplemented with cleansing enemas; this usually requires hospitalization in the surgical department [12]. The website gnck.ru clarifies that special preparation for patients with unloading ileostomy is not indicated [13]. However, in our practice, we quite often observe inadequate preparation of the colon for examination, even after cleansing enemas. For patients with a loop colostomy, standard preparation with oral bowel cleansing agents in combination with lavage of the obstructed sections through the colostomy is recommended. Patients with end colostomies (following Hartmann-type operations) should undergo standard preparation with oral bowel cleansing medications in combination with cleansing enemas. For patients after subtotal resection, a one-stage quick preparation followed by a cleansing enema is recommended - as for sigmoidoscopy. Non-ostomy patients after various types of colon and rectum resection and abdominal-anal resection are shown standard oral preparation [12].
Today, two-stage preparation or one-stage preparation with a full volume of polyethylene glycol on the day of the study is considered standard. A study by Liu et al showed that reducing the standard PEG volume from 4 L to 2 L in split mode in patients with colon surgery resulted in a decrease in the quality of preparation (89.4% vs. 66.7%, P < 0.001) [6] .
An effective alternative to full-volume PEG preparations is the use of a low-volume PEG preparation with an ascorbate complex (“MOVIPREP®”). The use of MOVIPREP® is preferable for outpatients and is associated with fewer adverse events such as nausea and vomiting, as well as greater patient compliance [2, 4, 5, 10, 11]. A multicenter randomized clinical trial conducted in Russia to evaluate the preparation of patients using the morning and two-stage regimen of using the drug MOVIPREP® showed that in both regimens, effective bowel preparation was observed in almost 100% of cases, including the right side [14].
Histological picture.
Histological changes in the disconnected bowel are present in all ostomy patients [1, 8, 9]. Mucosal biopsies in diversion colitis reveal signs of acute or chronic inflammation, eosinophilic infiltration, disturbance of crypt architecture, follicular lymphoid hyperplasia and crypt abscesses [1, 8, 9]. Son et al [8] also used a scale to assess the severity of diversion colitis, assessing these signs separately: acute inflammation (0–1 point); chronic inflammation (0–2 points); eosinophilic infiltration (0–2 points); violation of the architectonics of the crypts (0–1 point); follicular hyperplasia (0–1 point); crypt abscesses (0–1 point) - with a possible total score from 0 to 8. According to the total score, diversion colitis was divided into mild (1–3 points), moderate (4–6 points) and severe (7–8 points ) (see Fig. 3).
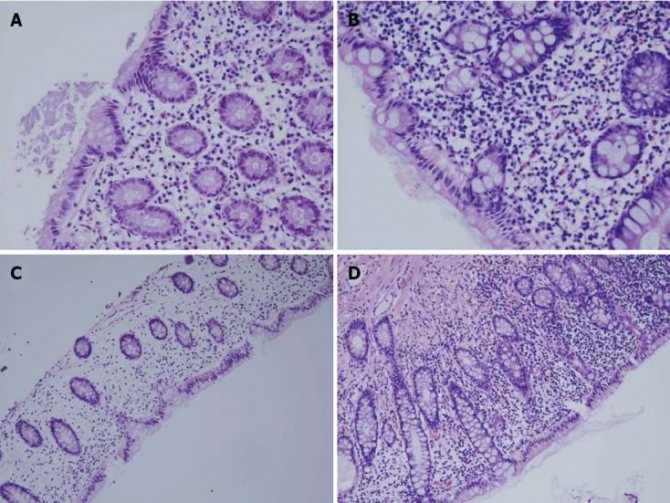
Figure 3.
Histological picture of diversion colitis [8].
An example of the main histological findings in diversion colitis depending on the relative severity.
A, B.
Eosinophilic infiltration (A - 1 point; B - 2 points; hematoxylin and eosin staining, magnification 400x).
C, D.
Chronic inflammation with mononuclear macrophages, lymphocytes and plasma cells (C - 1 point; D - 2 points; hematoxylin and eosin staining, magnification 200x).
Treatment.
The goal of treatment is to reduce or eliminate symptoms [3, 9]. Elimination of a colostomy or ileostomy leads to a cure, but Son et al indicate that diarrhea may occur in patients with severe diversion colitis after elimination of the stoma [8]. Pharmacological treatments are necessary for symptomatic patients with permanent ostomies and patients in whom ostomy closure cannot be performed due to technical difficulties, poor anal sphincter function, or persistent perianal sepsis. To date, there are no uniform approaches to the treatment of diversion colitis in such patients. Preparations of SCFA, 5-aminosalicylic acid, enemas with corticosteroids or fibers are used [1, 3, 9]. There are isolated reports of the use of fecotransplantation [9] and dextrose spray [7, 9].
conclusions
Diversion colitis is a nonspecific inflammation that occurs in the disconnected intestine after a stoma is applied. This condition develops in all ostomy patients, but symptoms (discharge of mucus and/or blood, tenesmus, abdominal pain, feeling of heaviness or pain in the rectum) occur in only 30% of people. Diagnosis of diversion colitis is based on colonoscopy data with histological examination of the biopsy specimen. Endoscopic signs of diversion colitis: swelling, granularity, petechial hemorrhages, contact bleeding of the mucous membrane, blurred vascular pattern. The histological picture is represented by signs of acute or chronic inflammation, eosinophilic infiltration, disruption of crypt architecture, follicular lymphoid hyperplasia and crypt abscesses. The main method of treatment for diversion colitis is the elimination of the stoma. There are currently no uniform approaches to drug treatment.
Bibliography
1. Vorobyov G.I., Zhuchenko A.P., Filon A.F., Kitchieva G.M. Colitis of the disconnected colon (literature review) // RZHGGK. - 2008. - T. 18. - No. 5. — P. 65–70.
2. Hassan C., Bretthauer M., Kaminski MF, Polkowski M., Rembacken B., Saunders B., Benamouzig R., Holme O., Green S., Kuiper T., Marmo R., Omar M., Petruzziello L., Spada C., Zullo A., Dumonceau JM; European Society of Gastrointestinal Endoscopy. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013. 45 (2): 142–150. Epub 2013 Jan 18. PMID: 23335011. DOI: 10.1055/s-0032-1326186.
3. Kabir SI, Kabir SA, Richards R., Ahmed J., MacFie J. Pathophysiology, clinical presentation and management of diversion colitis: a review of current literature. Int J Surg. 2014 Oct; 12 (10): 1088–1092. Epub 2014 Aug 20. PMID: 25150021. DOI: 10.1016/j.ijsu.2014.08.350.
4. Kim ES, Kim KO, Jang BI, Kim EY, Lee YJ, Lee HS, Jeon SW, Kim HJ, Kim SK; Crohn's and Colitis Association in Daegu-Gyeongbuk (CCAiD). Comparison of 4-L Polyethylene Glycol and 2-L Polyethylene Glycol Plus Ascorbic Acid in Patients with Inactive Ulcerative Colitis. Dig Dis Sci. 2020. Sep; 62(9):2489–2497. Epub 2020 Jun 21. PMID: 28639128. DOI: 10.1007/s10620-017-4634-7.
5. Kojecky V., Dastych M., Zadorova Z., Varga M., Hajer J., Kment M., Kroupa R., Kunovska M., Matous J., Misurec M., Hep A., Kianicka B., Latta J. . Vnitr Lek. 2020. Apr; 62(4):249–254. PMID: 27250601.
6. Liu Z., Li YY, Luo XT, Guo CG, Zhang MM, Li Z., Li LX, Zhang Y., Li YQ Split-dose 4-L polyethylene glycol regimen for patients with previous colorectal surgery in bowel preparation before colonoscopy: A randomized, controlled, single-blind study. J Dig Dis. 2020. Jun; 19 (6): 359–368. DOI: 10.1111/1751-2980.12608.
7. Nyabanga CT, Shen B. Endoscopic Treatment of Bleeding Diversion Pouchitis with High-Concentration Dextrose Spray. ACG Case Rep J. 2020. Mar 29; 4: e51. eCollection 2020. PMID: 28377939. PMCID: PMC5371723. DOI: 10.14309/crj.2017.51.
8. Son DN, Choi DJ, Woo SU, Kim J., Keom BR, Kim CH, Baek SJ, Kim SH Relationship between diversion colitis and quality of life in rectal cancer. World J Gastroenterol. 2013. Jan 28; 19(4):542–549. PMID: 23382634. PMCID: PMC3558579. DOI: 10.3748/wjg.v19.i4.542.
9. Tominaga K., Kamimura K., Takahashi K., Yokoyama J., Yamagiwa S., Terai S. Diversion colitis and pouchitis: A mini-review. World J Gastroenterol. 2020. Apr 28; 24 (16): 1734–1747. PMID: 29713128. PMCID: PMC5922993. DOI: 10.3748/wjg.v24.i16.1734.
10. Xie Q., Chen L., Zhao F., Zhou X., Huang P., et al. A Meta-Analysis of Randomized Controlled Trials of Low-Volume Polyethylene Glycol plus Ascorbic Acid versus Standard-Volume Polyethylene Glycol Solution as Bowel Preparations for Colonoscopy. PLoS One. 2014. Jun 5; 9(6):e99092. DOI:10.1371/journal.pone.0099092.
11. Zorzi M., Valiante F., Germana B., Baldassarre G., Coria B., Rinaldi M., Heras Salvat H., Carta A., Bortoluzzi F., Cervellin E., Polo M.L., Bulighin G., Azzurro M., Di Piramo D., Turrin A., Monica F.; TriVeP Working Group. Comparison between different colon cleansing products for screening colonoscopy. A noninferiority trial in population-based screening programs in Italy. Endoscopy 2016.Mar; 48(3):223–231. Epub 2020 Jan 13. DOI: 10.1055/s-0035-1569574.
12. Bowel Prep Protocol | Colonoscopy | Gastroenterology // 11/16/2018.
13. gnck.ru›rehabilitation.shtml // 11/16/2018.
14. Veselov V.V., Sidorov A.V., Vasilyuk V.B., Gordienko A.V., Menshikova I.L., Simanenkov V.I., Shcherbakov P.L. Low-volume PEG solution with ascorbic acid for preparation for colonoscopy using a single-stage morning or standard two-stage (split) regimen: a multicenter, single-blind, randomized, controlled trial in parallel groups. Coloproctology. No. 2 (60). 2020. - pp. 5-18
[Oe2] CIBD is represented by Crohn's disease and ulcerative colitis. Patients with these diseases have clinical manifestations more often than patients with other pathologies.
Causes of development of acute intestinal colitis
The disease develops against the background of damage to the intestinal mucosa. The infection can enter the body through water, dirty fruits and vegetables. Failure to comply with hygiene rules can also become the basis for infection.
Acute colitis can develop against the background of concomitant diseases. These include:
- salmonellosis;
- dysentery;
- food poisoning, etc.
Violation of intestinal microflora and dysbiosis can also trigger the development of inflammation.
In addition to the above, among the causes of intestinal inflammation are:
- exposure to viruses, fungi and parasites. They can enter the body through unwashed hands, spoiled food or dirty water;
- poisons and chemicals. For example, colitis often develops against the background of radiation exposure during oncology therapy;
- taking certain medications. Some medications can destroy the natural intestinal microflora. As a result, a favorable environment is created for the development of the inflammatory process. Very often, the root cause of colitis is antibiotics;
- abuse of laxatives. In this case, the natural intestinal microflora is also disrupted.
Poor blood circulation in the abdominal organs can also cause acute colitis. In severe cases, the inflammatory process easily spreads to neighboring organs.
Causes
Erosive intestinal colitis can be caused by various factors, both individual, such as genetics, and common. The root cause of the pathology is identified by the doctor. Based on the data obtained and the picture of the disease, he draws up a treatment regimen.
Possible causes of erosive colitis:
- violation of the diet, abuse of fried, fatty, spicy and smoked foods;
- heredity;
- long-term treatment with medications that disrupt the intestinal microflora, which increases the vulnerability of its mucosa to external and internal negative factors;
- excessive consumption of alcoholic beverages;
- sluggish allergic reaction;
- intoxication of the body with chemicals, poisons, food toxins;
- bacterial or viral infection in the digestive tract;
- disruption of blood supply to internal organs;
- radioactive exposure;
- concomitant diseases of the digestive system: gastritis, pancreatitis, cholecystitis, etc.;
- helminthic infestations, parasitic pathogens;
- stress, overwork, sleep problems.
Diagnostics
Diagnosis of acute colitis includes the following steps:
- anamnesis collection. The doctor asks the patient a series of questions. All data received is recorded in the patient’s personal record;
- palpation and external examination. The doctor palpates the abdominal area. This allows you to identify the source of inflammation and the places of greatest pain;
- instrumental examination. To diagnose acute colitis, they resort to the endoscopy method. This method allows you to detect not only the source of inflammation itself, but also possible erosions and ulcers;
- laboratory research of biomaterial. The patient's blood and feces are taken for examination. Blood counts can detect the presence of inflammation in the body. Stool analysis will help determine the type of causative agent of the inflammatory process.

Timely diagnosis allows you to detect the disease at an early stage.
How does intestinal inflammation develop?
Erosive colitis is inherently one of the initial stages of the inflammatory process in the intestines. Read more about intestinal inflammation →
Initially, a person develops a superficial form of colitis, that is, inflammation affects the superficial layers of the intestinal mucosa. If treatment and diet are absent, the disease will quickly move into the next phase - the inflammatory process will be aggravated by the development of erosive lesions on the mucosa. This stage can last quite a long time, but its exact timing directly depends on the lifestyle the patient leads.
If a person continues to neglect his diet, abuse alcohol and does not treat concomitant pathologies, then soon the resulting erosions will transform into ulcerative defects.

As a result, the disease will move to a new, more severe stage. To prevent this, it is important to consult a doctor if any signs of trouble with the digestive organs appear.
Possible complications
Among the complications of acute colitis, the greatest danger is:
- perforation of the intestinal walls. Most often, this condition develops against the background of severe intoxication. Because of this, it can be very difficult to notice. With perforation, the patient’s well-being rapidly deteriorates;
- expansion of the colon. In this case, the organ loses its functionality. Problems with defecation develop. In the future, the pathology can lead to perforation of the organ. As a result of this complication, the risk of death increases;
- intestinal bleeding. They can have different intensities. If the bleeding is severe and the blood loss is large, surgical intervention cannot be avoided.

Photo: LightField Studios / Shutterstock.com
What causes the disease
Spastic colitis is a disease characterized by inflammation of the mucous membranes of the large intestine, most often having a chronic form. In most cases, the disease occurs at a young age. Men suffer from this type of colitis much less frequently than women.
There are quite a few factors that influence colon irritation. To date, the specific cause of this disease has not yet been identified. But doctors confidently say that the following can lead to the appearance of colitis:
Recipes, menus and diet products
- hormonal disorders;
- presence of parasites;
- allergic reaction;
- long-term treatment with certain medications;
- chronic diseases;
- improper and unbalanced nutrition that continues for a long time;
- stress;
- physical or psychological fatigue;
- poisoning with toxic substances (with prolonged exposure);
- undergone surgery.
In addition, spastic colitis with constipation often manifests itself against the background of diseases of the gastrointestinal tract, such as dysbiosis, pancreatitis, gastritis, enteritis, etc. The causes of irregular, spastic stools also include congenital intestinal pathologies. All these ailments lead to the fact that food, being insufficiently digested, penetrates the large intestine and irritates its lining, which is accompanied by an inflammatory process.
The main reason for the development of spastic constipation in colitis is poor nutrition. With a large consumption of spicy, fried and heavy foods, the intestines cannot cope with their function, which causes problems with bowel movements. Alcoholic drinks also affect the quality of stool, especially when consumed regularly and in large quantities.
In the presence of spastic colitis, the appearance of constipation is affected by the lack of fiber in the diet. In addition, frequent suppression of the urge to defecate can affect stool disorder.

Recipes, menus and diet products
Use of Pharmaceuticals
Drug therapy for intestinal colitis plays an important role in the treatment of the disease. The choice of medications is made individually. It all depends on the severity of the pathology and symptoms. Identifying the root cause of inflammation also plays an important role. For example, if colitis was caused by bacteria, antibiotics are used to treat it. Regardless of the root cause, all patients are prescribed medications to normalize and maintain microflora:
- Linux;
- Bifiform;
- Enteroseptol;
- Bactisubtil.
To alleviate the symptoms of intoxication, patients are prescribed sorbents:
- Smecta;
- Enterosgel;
- Activated carbon, etc.
For ulcerative intestinal colitis, patients are prescribed Sulfasalazine or Mesalazine. Both drugs have a similar principle of action. However, the second one is much easier to tolerate by patients.
To get rid of pain, people are prescribed antispasmodics. This may include:
- Papaverine;
- No-shpu;
- Atropine, etc.
If the pathology is accompanied by profuse vomiting, the patient is given antiemetics:
- Metoclopramide;
- Chlorpromazine.
To get rid of diarrhea the following is prescribed:
- Loperamide;
- Cholestyramine.
It is very important to monitor compliance with the drinking regime during the treatment phase. Excessive vomiting and diarrhea can lead to rapid dehydration. To replenish fluid balance, it is recommended to use special pharmaceutical products. These are powders intended for preparing a water-salt solution. It is drunk in small portions throughout the day. In severe cases, with severe dehydration, the patient is admitted to the hospital. There he is given IV drips with saline or glucose. Treatment of acute colitis requires an integrated approach.

Photo: Pressmaster/Shutterstock.com
How do medications work?
Sulfonamides and antibiotics are used if the symptoms of chronic colitis are bacterial in nature. Depending on the degree of sensitivity of the pathogen, the duration of the course of treatment is determined:
- If Giardia and helminths are found in patients, antiparasitic drugs are used.
- Sorbents help eliminate waste and toxins from the intestines and reduce inflammation.
- Antispasmodics help cope with cramping attacks of pain.
- Treatment using enzymes is recommended when colitis spreads to nearby organs.
- To restore the composition of favorable microflora, probiotics are used.
- Vitamin complexes are used to strengthen the immune system.

All medications can have side effects, so they must be taken in accordance with the prescribed dosage.
Nutrition for acute colitis
In the treatment of colitis, diet is important. The choice of dishes depends on the severity of the pathology and the root cause of the disease. Table No. 4 is often recommended to patients.
General nutritional recommendations include the following:
- reduction of diet in the first days after the onset of inflammation. During this period of time, patients are allowed only tea with lemon or rosehip decoction. It is best to exclude any food products completely;
- gradual inclusion in the diet of soups, cereals, lean meats, etc. Portions should be minimal. Under no circumstances should you overeat;
- enriching the diet after relieving the symptoms of inflammation. After this, the patient’s menu becomes more varied.
However, people with acute colitis need to exclude some foods from their diet for the entire period of treatment. These include:
- alcohol;
- carbonated drinks;
- strong tea and coffee;
- fried foods;
- fatty meat and offal;
- spicy seasonings;
- eggs;
- whole milk.
After recovery, you need to stick to the diet for another 2-3 weeks. This will avoid relapse and allow the mucous membrane to fully recover.
Authorized products include:
- dried white bread;
- low-fat cottage cheese;
- porridge with water;
- lean meat;
- jelly and decoctions;
- cocoa prepared with water.
It is best to boil or steam foods. The food can be chopped or pureed before eating. This will facilitate the process of digestion and absorption of nutrients.
Treatment
When choosing a treatment method, a specialist must take into account many factors, correctly identify the type of dyskinesia, determine the symptoms, and find out the reasons that caused the disease. Treatment of large intestinal dyskinesia consists of a comprehensive approach and includes the following measures:
- Conservative drug treatment;
- Correction of nutrition and lifestyle;
- Physiotherapeutic procedures;
- Psychotherapy;
- Therapeutic gymnastics.
Treatment with medications includes taking medications aimed at normalizing stool and regulating intestinal motility. Along with them, patients must take psychotropic and sedative medications. Physiotherapeutic methods of treatment are based on oxygen and pine baths, acupuncture, and paraffin baths. Along with these procedures, massage and enemas are also used.
Experts recommend that patients with large intestinal dyskinesia drink mineral water. For the hypotonic type of the disease, water with a high degree of mineralization is prescribed, for the hypertonic type - with a low one. Thus, the course of treatment includes taking antispasmodics and anticholinergics, laxatives are prescribed (vaseline or olive oil on an empty stomach).
It is recommended to take low mineralization mineral water. Drink water warm, without gas, an hour before meals. Patients are given a course of therapeutic exercises with relaxation exercises, and undergo acupressure and segmental massage.
Hydrotherapy procedures, warm radon and carbon dioxide baths, as well as rectal mud tampons are prescribed.
Physiotherapeutic measures include electrophoresis with novocaine, a diathermy procedure, and paraffin and ozokerite applications are prescribed.

Therapy for hypotonic dyskinesia of the colon is based on taking drugs that enhance intestinal peristalsis and motor functions. Laxatives are prescribed that help increase the volume of stool and facilitate bowel movements (Duphalac, Laminaride, Regulax, Kafiol). Patients are prescribed treatment with mineral waters with a high degree of mineralization. Drink cold water an hour before meals.
Patients are prescribed a general abdominal massage and intestinal lavage with cool mineral water. Hydrotherapy treatments include a circular shower and underwater shower-massage. During physical therapy exercises are performed to strengthen the abdominal and pelvic floor muscles. Physiotherapeutic methods include electrophoresis with calcium.
Diet
For large intestinal dyskinesia, a daily diet is recommended. The concept of “diet” also includes the method of cooking, quality, types of food, and diet. What are the nutritional features of patients with spastic colitis? Products must be of high quality, without preservatives, dyes and various flavoring additives. Porridges are healthy (oatmeal, buckwheat, millet, wheat), but the consumption of rice should be limited.
The daily diet should be varied with a sufficient amount of fresh fruits and vegetables rich in fiber to restore intestinal functionality. It is good for chronic intestinal constipation to drink juices (apple, carrot, beetroot, cabbage) on an empty stomach. Drink plenty of liquid per day (from 1.5 l). Steam or boil food. Eliminate fried, fatty, spicy foods from your diet. Do not consume fatty sour cream, fatty fish and meat.

Fermented milk products should be on the menu every day. Eliminate flour products, sweets, white bread, white cabbage, garlic, radishes, turnips, and mushrooms from your diet. Don't add enough salt to your food. It is useful to drink rosehip decoction, but without sugar. Doctors, as a rule, recommend eating small portions, at least 5-6 times a day. Don't overeat.
By following these simple recommendations, you will be able to achieve significant success: intestinal motility will improve, preventing the occurrence of constipation. As a result, spastic colitis does not progress, but rather the opposite: intestinal dyskinesia recedes.
For hypertensive dyskinesia of the colon, regular consumption of vegetable oil is recommended. It is expected to avoid baked goods, fatty meats, foods containing starch, canned and spicy foods, strong black coffee and tea. You should be careful when consuming foods that cause increased gas formation and contain coarse fiber.
This can cause intestinal spasms and pain. Therefore, eating raw vegetables and fruits is not recommended. It is better to steam, boil, stew or bake food; fried foods should be avoided.
For hypotonic dyskinesia of the colon, it is recommended to include vegetables and fruits and greens in the daily menu. You can eat carrots, tomatoes, cucumbers, zucchini, beets, apples, apricots, and plums. It is better to exclude vegetables with a high content of essential oils.
It is useful to include wheat bran or wholemeal bread, fermented milk products, cereals, lean meat and fish in your diet every day. Juices, cold foods and drinks will help stimulate the intestines. Fresh berries and fruits will enhance the evacuation function of the intestines.
Treatment with traditional methods
This disease can be treated with decoctions of medicinal plants and some other alternative medicine. These are effective and safe methods that can be used during pregnancy and breastfeeding.
Aloe helps with hypomotor dyskinesia. A few leaves are peeled and finely chopped. The resulting mass should be mixed with 300 g of fresh honey. The drug is infused for 24 hours and taken 1 tbsp in the morning. l. When preparing this product, honey should not be heated to too high a temperature; heat treatment contributes to the disappearance of its beneficial properties. For irritable bowel syndrome, use potato or cabbage juice. It is drunk on an empty stomach after waking up. This treatment cannot be carried out for diabetes mellitus.
Green tea helps improve the patient's condition with spastic colitis. It eliminates pain and seizures. The leaves are ground in a coffee grinder and taken 3 times a day before meals. This method can be used in the treatment of intestinal dyskinesia in children. Watermelon rinds help normalize the functions of the digestive system. They are ground into powder and used to prepare an aqueous tincture. The berries are thoroughly washed and the pulp is removed. The remaining crusts are dried in the sun or in the oven. For 0.5 liters of boiling water take 3 tbsp. l. powder. The drug is infused for 24 hours and taken 3 times a day before meals.
During an exacerbation of the disease, it is recommended to drink apple juice mixed with honey in a ratio of 1:10. The course of treatment lasts 45 days, after which there is a break for 3 months. An irritated colon can be restored by drinking an infusion of chamomile. 50 g of raw materials are poured into 1 liter of boiling water, infused for 3 hours and mixed with 100 g of honey. The drug is taken 3 times a day before meals for 8 weeks.
Fennel tincture improves the condition of the body: take 20 g of this plant per 200 ml of water. Often this treatment is combined with the use of psychotropic drugs: antidepressants, antipsychotics and tranquilizers. Since the disease often occurs against the background of mental disorders, it is advisable to use autogenic training, psychotherapeutic techniques, and meditation.
Prevention of pathology
Acute intestinal colitis is accompanied by severe pain and discomfort. The disease makes significant changes to a person’s usual way of life. That is why it is best to prevent its development. Measures to prevent acute colitis include:
- compliance with the diet. Exclusion from the diet of low-quality, spicy and heavy foods. Eating meat and fish after preliminary heat treatment;
- use only boiled water. You cannot drink tap water without pre-treatment;
- compliance with personal hygiene rules. After visiting public places or walking, you must wash your hands thoroughly. It is also necessary to wash your hands after working with meat or fish;
- regular examination by a doctor. Diseases of the gastrointestinal tract cannot be neglected. Once a year you need to undergo preventive intestinal examinations. If you are prone to intestinal pathologies, you need to visit a gastroenterologist more often;
- taking vitamins and microelements. It is necessary to maintain immunity. Especially during the period of greatest peak incidence.

Acute intestinal colitis is a disease that can create a significant imbalance in the life of any person. In the absence of timely assistance, the disease quickly becomes chronic. During pathology treatment, it is very important to follow all doctor’s recommendations.
Features of the disease
Chronic intestinal colitis occurs to the same extent in people, regardless of gender. The difference can only appear in the age category.
In women, painful symptoms appear from 20 to 60 years, in men up to 65 years. Chronic colitis occurs for various reasons:
- Stress.
- Poor quality diet.
- Lack of personal hygiene.
There are internal and external symptoms of chronic colitis, so diagnosing the disease is not difficult. Therapeutic measures are taken comprehensively; it is important to follow the diet developed by the attending physician.