Resection of the rectum is the excision of its affected part. The rectum continues the colon and is located from the sigmoid to the anus. This is the final part of the digestive tract, the length of which is 13–15 cm. Feces accumulate in it and are subsequently excreted. It got its name because it has no bends. The main ailments of the rectum are: various processes of inflammation, Crohn's disease, obstruction, ischemia, cancer. The main treatment for such diseases is surgery.
Types of operations
To eliminate rectal cancer, the best treatment is surgery. In medical practice, depending on the location of the tumor and its size, there are several methods of excision:
- Polypectomy is the simplest operation to remove polyps and minor tumors. During this procedure, nearby tissues are minimally damaged. Surgery is performed using an endoscope if the tumor is located near the anus.
- Anterior resection of the rectum - is done by removing its upper part and the lower end of the sigmoid colon. The remaining part of it is connected to the sigmoid colon. At the same time, the nervous apparatus and anus are preserved. For quick healing, a temporary colostomy is sometimes placed, which is removed after a second operation after about two months.
- Low anterior resection – is performed to remove pathology in the middle part of the rectum. In this case, the damaged part of the sigmoid and the entire rectum, except the anus, are excised. The reservoir function of the intestine is lost. The place for the accumulation of feces is formed from the lowered intestine, which is located above. The sigmoid colon is connected to the rectum by anamostosis. In almost all cases, an ostomy is performed to relieve the load over a period of several months.
- Abdominal-anal resection – performed from the abdominal cavity and anus. Resection of the rectum is done when the pathology is located close to the anus, but does not affect it. The part of the sigmoid colon that is completely straight with the anal sphincter portion is subject to removal. The remaining sigmoid colon is used to form an anastomosis with part of the anal sphincter.
- Abdominal-intermediate extirpation - through two incisions, one of which is on the abdomen, and the other around the anal canal. In this case, the rectum, anal canal and anal sphincter muscles are subject to resection. Feces are drained through the formed stoma.
Indications for surgery

Extirpation of the rectum is performed:
- in advanced cases of colorectal cancer;
- with tissue necrosis;
- with non-reducible areas of the prolapsed rectum.
The choice of type of operation is determined by the distance of the tumor from the anus. If it does not exceed 6-7 cm, BPE (abdominoperineal extirpation of the rectum) is used. It is also called the Quenu-Miles operation.
If the tumor is located higher (but not higher than 10 cm), this makes it possible to perform sphincter-sparing surgery - BPE with sigma reduction.
Well, if the tumor is 10-12 cm above the anus, another type of operation is performed with preservation of the sphincter (sphincter) - anterior and lower resection, Hartmann's operation, etc.
Resection technique
Surgery to remove part of the rectum can be performed in two ways: using laparotomy or laparoscopy. During a laparotomy, an incision is made along the lower abdomen. The surgeon receives a good overview of all procedures performed. The laparoscopic method involves several small holes for inserting surgical instruments into the abdominal cavity. The technique of open rectal resection is as follows:

When moving from one stage of the operation to another, the surgeon changes instruments to avoid infection with intestinal contents.
Small bowel resection
Diseases of the small intestine are quite rare, despite the fact that the length of the small intestine is nine times longer than the large intestine.
Inflammatory and ulcerative processes of the duodenum - the initial part of the small intestine, small ileal polyps that do not require resection, and appendicitis are mainly diagnosed. Of the malignant processes, and they account for barely 5% of all neoplasms of the gastrointestinal tract, adenocarcinomas and neuroendocrine neoplasms are diagnosed - carcinoids, in a ratio of 50% to 40%, and slightly less than 10% are malignant lymphomas.
Benign diseases are cured by economical (simple) resection; in malignant diseases, the volume of the resected area is large, since it includes the mesentery with several groups of lymph nodes. Diagnosis of the pathology of the jejunum, where carcinoid tumors are predominantly localized, is complex and imperfect, so resection is possible only in seven out of ten patients.
Laparoscopic anterior rectal resection
As mentioned earlier, resection can be performed not only openly, but also using laparoscopy. In this case, several holes are made into which laparoscopic instruments are inserted. The proven technique for carrying out such operations is becoming increasingly popular due to the low level of trauma to the patient and a number of other advantages. The operation of anterior resection of the rectum in the upper sections begins with the intersection of the vessels. Then the affected part of the intestine is isolated and brought out through a small hole in the anterior abdominal wall, where resection is performed and the ends of the intestine are sutured.

The same steps are followed for resection of the lower colon. Anastomosis (connection of two parts of the intestine) is carried out based on anatomical conditions. If the loop is long enough, the area with the tumor is brought out through the hole, it is excised, and the ends are sutured. Otherwise, when the length of the intestine does not allow it to be brought out, resection and joining of the ends is performed in the abdominal cavity, using a special circular stapler.
Research methods
A comprehensive examination will help avoid mistakes when making a diagnosis.
X-ray, ultrasound and instrumental methods are used to examine the intestines.
X-ray examination includes a survey of the abdominal organs, a contrast study with the introduction of a barium sulfate suspension, and a computerized tomographic scan - virtual colonoscopy.
Modern ultrasound examination is carried out in 3D format, Doppler ultrasound is also performed, which provides information about the structure of the organ, its vessels, and blood circulation.
The most common instrumental methods include rectoscopy (examination of the rectum), intestinal colonoscopy, when, after special preparation (cleaning), an endoscope equipped with a miniature camera, a system of magnifying lenses and lighting is inserted. In this way, the rectum, sigmoid, and colon sections are examined to the ileocecal angle - the place where the ileum enters the cecum.
The thin section is difficult to access due to its anatomical features - tortuosity, many loops. Capsule endoscopy is used for this purpose. The patient swallows a small capsule (PillCam) containing a video camera-scanner, and it, moving gradually from the stomach along the entire digestive tract, scans and transmits the image to the computer screen.
Advantages of laparoscopic surgery
It has been experimentally established that the results of operations performed using the laparoscopic method are not inferior in quality to the results of rectal resection performed using laparotomy (open access). In addition, they have the following advantages:
Complications
After surgery, the patient may develop complications. In particular, this is the development of bleeding when tissues heal poorly and any stress leads to their damage. If the bleeding is internal, the patient experiences pain at the site of injury and anemia develops. With improper care or a carelessly performed operation, the patient's sutures may fester. In this case, you need to notify your doctor about this, as a serious complication may develop with the addition of a bacterial infection. Less often, during intervention, the patient may be damaged by the nerves that pass through the organ, and neighboring organs may be damaged.
Disadvantages of laparoscopy
The disadvantages include:

In some cases, during the operation, which began using laparoscopy, they switch to laparotomy.
What will happen after the operation?
After rectal resection, the patient is transferred to the intensive care unit, where he will recover from anesthesia. The patient is then admitted to the surgical ward for further rehabilitation. During the first time after the surgical period, nutrition is administered to the patient intravenously using a dropper. After seven days, you are allowed to switch to eating regular food, prepared in liquid form. Gradually the transition to solid food is carried out. For a quick recovery, physical activity has a great influence, so the patient is recommended to walk and perform exercises for the respiratory system. Approximately ten days after the operation, the patient is discharged, but treatment will continue in the oncology department.
Resection for polyps
Rectal polyps are tumor-like formations, mostly benign in nature. But sometimes their nature changes and they become malignant tumors. In this case, the radical treatment method is resection of rectal cancer.
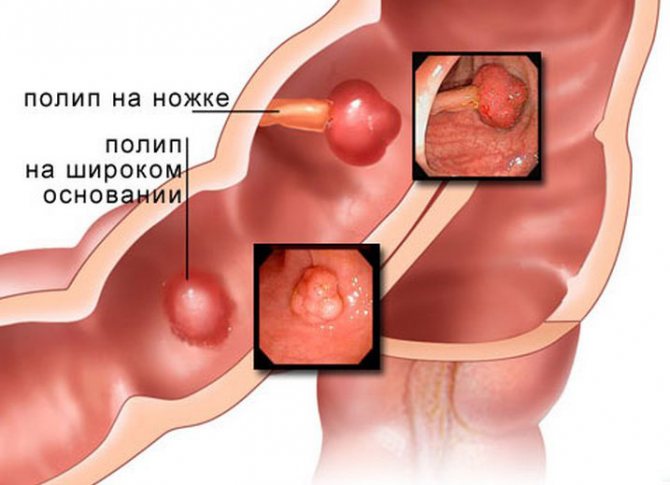
If there are polyps with symptoms of malignancy, part of the rectum is excised or it is completely removed. The length of the area to be removed depends on the degree of damage to the polyp. If the cancer process spreads to nearby areas of the rectum, the entire affected part is removed. And if metastases appear, then the lymph nodes must also be excised.
Types of intestinal connections after resection
After removing the abnormal section of intestine, the doctor must connect the remaining ends or perform an anastomosis. The opposite ends of the intestine may differ in diameter, so technical difficulties often arise. Surgeons use three types of connections:
For stitching, a manual or machine stitch is used. If it is technically impossible to restore the intestines or to quickly recreate its functions, a colostomy (outlet) is used on the anterior wall of the abdomen. With its help, feces are collected in a special colostomy bag. A temporary colostomy is removed after a few months, but a permanent one remains for the rest of your life.
Consequences of rectal resection
An operation to remove part of the rectum sometimes has negative consequences:

After resection of the rectum, the operated organs continue to function and can be injured by feces. To prevent injury, the patient must strictly follow the diet recommended by the doctor and avoid physical activity for six months.
Possible consequences of the operation
After any surgical intervention, even after appendectomy, disturbances occur to varying degrees. In the first days, intestinal atony, weakened peristalsis, bloating, and difficulty passing gases often develop. It is no coincidence that surgeons jokingly call the normalization of this process in an operated patient “the best music for a doctor.”
The development of many other consequences is also possible: abscess, peritonitis, bleeding, wound suppuration, obstruction, suture failure, post-anesthesia complications from internal organs. All this occurs in the early period, when the patient is under observation in a hospital, where specialists will provide professional assistance in a timely manner.
Nutrition in the postoperative period
In the postoperative period, it is especially important to follow a special diet so that it does not injure the intestines or cause fermentation and diarrhea. On the first day after surgery, the patient fasts; the necessary vitamins and minerals are administered intravenously. Fermented milk products, legumes, raw vegetables and fruits are excluded for two weeks. Subsequently, the diet does not greatly limit the diet of the operated patient. Sample menu after rectal resection:

There are many different recipes for preparing dishes, so you can use them to have a varied diet.
Nutrition while preparing for surgery for colon cancer
A diet is immediately determined, foods that give a lot of toxins are excluded from the diet: fruits, potatoes, cabbage, beans, peas. High-calorie, fortified foods low in toxins are prescribed. Vitamins can be given separately as intravenous infusions with glucose or as tablets by mouth. Small quantities of boiled meat, eggs, butter, sour cream, fruit juices, rice, soufflé with cream, yogurt, and kefir are recommended. It is advisable to coordinate the patient’s nutrition with a diet doctor.
Prevention of colorectal cancer
To prevent colorectal cancer, you should lead a healthy lifestyle, breathe fresh, clean air, drink high-quality water, eat more plant-based foods and limit the use of animal fats. An important factor is secondary prevention, timely detection of polyps and their removal. There is a high probability of detecting cancer cells in a polyp whose size is more than five centimeters. The polyp develops very slowly over 10 years. This time is used for preventive examinations, which begin to be carried out from the age of fifty in people who do not have risk factors for developing colorectal cancer. For those who are predisposed to developing cancer, preventive measures begin ten years earlier. It is important to immediately consult a doctor if suspicious symptoms appear in the bowel function and undergo an examination so as not to undergo rectal resection.
Preparation of the colon for examinations and operations in patients with colorectal cancer
More often, preoperative bowel preparation in the presence of partial colonic obstruction is carried out using standard measures - a slag-free diet and mechanical cleansing [6]. Such techniques are effective in 7.5–29.7% of cases [4]. A number of authors recommend the use of special elemental diets. Upon admission, the patient is given one cleansing enema and prescribed a diet including infant formula, vitamins, and minerals for 10 days. Drinking is not limited. Before the operation - another cleansing enema. E.A. Demerchyan (1992) notes that when chocolate and orange juice are added to such diets and laxatives (30 g of petroleum jelly or 33% solution of magnesium sulfate once) a day before surgery, the frequency of purulent-septic complications decreases from 13.8 to 6.3% [4]. At the same time, C. Schumann (1996) indicates unsatisfactory bowel preparation using this method in 83% of patients [10]. According to N.A. Belyakova (1989), taking polyphepan along with a slag-free diet for 5–7 days can reduce purulent-septic complications from 40.0 to 17.6% [2]. G.I. Vorobyov (1988) proposed a method of general lavage of the gastrointestinal tract (lavage). This method is applicable in the absence of stenosis or its compensated stage [3]. Contraindications are acute and chronic subcompensated intestinal obstruction, severe cardiovascular, renal, liver failure, diabetes mellitus, hypoparathyroidism, old age [8]. A number of authors suggest that lavage should be preceded by taking 30–60 g of castor oil, and when planning an operation with a perineal stage, one cleansing enema on the eve of the operation in the evening. At the same time, G.I. Vorobyov (1988) notes a decrease in purulent-septic complications to 9.9%, and I.S. Popova (1988) – from 23.14 to 17.39% [3.7]. There are many reports in the literature about the use of polyethylene glycol in preparation for colon surgery. Macrogols with a molecular weight of 3000 to 4000 are used as osmotic laxatives. To achieve the effect, simultaneous intake of a large amount of liquid (up to 2 liters) is necessary [5,9]. Elimination of obstruction was observed in 82–86% of cases [4]. For stenosing cancer, preparation of the colon is reduced to a slag-free diet from the day of admission, taking a 15% solution of magnesium sulfate 30 ml 4-6 times a day, in the evening before surgery - 2 cleansing enemas, in the morning - one [3]. In cases of complete (decompensated) colonic obstruction, conservative measures are in the nature of immediate preoperative preparation (infusions, fasting); patients are operated on urgently within a few hours. Thus, clinics treating colorectal cancer currently use different methods of preparing the intestine for surgery. Materials and methods In 39 patients with rectal cancer, we used the following method of preparation for surgery: from the moment of admission with subcompensated and compensated intestinal obstruction, patients received a slag-free diet. 4 days before surgery, patients took a 15% solution of magnesium sulfate, 30 ml, 5 times a day for 30 minutes. before meals; cleansing enemas were given 2-3 days before the operation, one in the evening, on the eve of the operation - two, in the morning on the day of the operation - one (4-5 enemas in total). Patients finished eating in the morning the day before surgery; the remaining time of the day on the eve of surgery was allowed to drink up to 1.5–2 liters of liquid. All patients received combined treatment including preoperative large-fraction radiation therapy and surgery. Among them there were 18 (46.2%) men and 21 (53.8%) women. The tumor was localized in the inferior ampullary in 21 (53.8%) patients, in the middle ampullary in 12 (30.7%), in the upper ampullary in 6 (15.4%). Intestinal damage along the circumference was up to 1/3 in 1 (2.6%) patient, from 1/3 to 1/2 in 22 (56.4%), more than 1/2 in 12 (30.7%), circular growth was noted in 4 (10.3%). The average length of the lesion along the length of the intestine was 4.9 cm. In one case, the tumor was complicated by obstruction, which was not decompensated; the remaining patients had an uncomplicated course of the disease. The above-described preparation technique made it possible to perform transabdominal resection of the rectum in 8 (20.5%) patients, one of them with a preventive sigmostoma and one with a J-shaped reservoir. The postoperative period in 4 patients was complicated by anastomotic failure, treated conservatively, in one - thrombophlebitis of the legs, in one - myocardial infarction. Abdominal-anal resection of the rectum with reduction of the sigmoid colon into the anal canal was performed in 21 (53.8%) patients. At the same time, coloanal anastomosis was formed in 8 (38.1%) of them. Necrosis of the reduced intestine, requiring the application of a transversostomy, was observed in 1 case, suppuration in the pelvis - in one, rectovaginal fistula - in one. Abdominal-anal resection with colostomy had to be performed in 4 (10.3%) patients: in 1 case due to previous gastric surgery, in one due to bleeding, in two due to insufficient blood supply to the intestine being prepared for removal. There was a complication (suppuration in the pelvis) after such an operation in 1 patient. Extirpation of the rectum was performed in 6 (15.4%) cases: due to insufficient blood supply when trying to reduce it - in two, due to the local spread of the tumor - in three. Complications (suppuration in the pelvis) developed in 5 patients; one patient died. Thus, sphincter-preserving operations after bowel preparation using this method were performed in 29 (74.4%) patients; purulent-inflammatory complications were observed in 7 (24.1%) of them. Surgeries with colostomy were performed in 10 (25.6%) patients. Postoperative mortality was 2.6% for the entire group of patients. The search for methods that could reduce the preparation time for examinations and operations on the colon, and ease the work of nursing staff, led us to the use of the drugs “X-prep” and “Duphalac”. The method of preparation with the drug "X-prep" was as follows: in the first half of the day before the operation, the patient took a bottle (75 ml) of the drug "X-prep" orally, and then, during the rest of the day, drank 2-3 liters of liquid (clarified juices, mineral or plain water without gases). In this case, in the morning, before taking the drug, an easily digestible breakfast was allowed, and after that, eating was prohibited (cleansing enemas were not included in the method). A contraindication, in addition to increased individual sensitivity, was the stenotic nature of the colon tumor. This method of preparation for the study was used in 37 patients with various colon tumors and suspected of their presence. Irrigoscopy was performed in 19 patients, of which 10 were patients with rectal cancer. In this case, the preparation was considered satisfactory in 6 patients, unsatisfactory in 4 patients, however, in only one patient the presence of feces in the intestinal lumen prevented the filling of the colon with contrast up to the valve of Baugin. In 2 patients with primary multiple synchronous colon cancer against the background of polyposis, in 2 patients after resection of the colon with the formation of an anastomosis, in 1 patient after obstructive resection for rectal cancer, in 1 patient with a villous tumor of the rectum, the preparation was also considered satisfactory . Of the two patients without organic lesions of the colon (lung cancer and B12-deficiency anemia), in 1 the preparation was satisfactory, and in 1 the study failed due to the presence of feces in the intestinal lumen, which prevented the filling of the contrast. In 1 patient with sigmoiditis, preparation was considered unsatisfactory, although the contrast mass freely filled all parts of the colon. Thus, in 17 (89.5%) patients, during irrigoscopy, the contrast mass filled the colon up to the Bauginian valve, although the preparation was considered satisfactory in 13 (68.4%) patients. In 6 (31.6%) patients, the preparation was considered unsatisfactory; in 2 (10.5%) of them, feces in the intestinal lumen prevented its filling with contrast. Colonoscopy was performed in 18 patients, 5 of them with villous tumors of the rectum (for the purpose of endosurgical sanitation); in all 5, the preparation was considered satisfactory, although a total colonoscopy was not performed. Of the 4 patients with rectal cancer, the preparation was considered satisfactory in 3, and in 1 patient, dense stool prevented the performance of a total colonoscopy. Three patients who underwent rectal resection with colostomy underwent total colonoscopy; in one case, poor preparation was noted. In 2 cases, the lumen of the transverse colon altered by the tumor was impassable for the colonoscope, but the examined area was prepared satisfactorily. Of the 3 patients without organic lesions of the colon, total colonoscopy was successful in 2 (with unsatisfactory preparation noted in 1), and in 1 the study was stopped due to dense fecal masses in the intestinal lumen. In 1 patient with scar narrowing of the anastomosis after combined treatment for rectal cancer, colonoscopy was discontinued for the same reason. Satisfactory quality of preparation for colonoscopy was noted in 13 (72.2%) patients, unsatisfactory in 5 (27.8%), and in 3 (16.7%) patients the presence of feces in the intestinal lumen prevented a total examination of the colon. Thus, during an instrumental examination of the colon of 37 patients prepared using "X-prep", satisfactory preparation was noted in 26 (70.3%) cases, unsatisfactory - in 11 (29.7%), and the study was interrupted in 5 ( 3.5%) cases of which are due to the obstruction created by feces in the intestinal lumen. V.L. Astashov and A.F. Loginov (2003) uses lactulose preparations (Duphalac) as an adjuvant for preoperative bowel preparation. The laxative effect of lactulose is determined by two main mechanisms: a decrease in the pH of the colon contents and stimulation of peristalsis; bacterial breakdown of lactulose to fatty acids with an increase in osmotic pressure in the intestinal lumen. To achieve a guaranteed laxative effect, the dose of Duphalac in the form of syrup should be 40–60 ml. The drug is used on the day of surgery with an interval of 5–6 hours, followed by a single cleansing enema with a volume of no more than 1 liter. If Duphalac is taken on the eve of surgery, then the enema is performed in the morning on the day of surgery [1]. We used Duphalac in 17 patients with colorectal cancer to prepare for colon surgery. A combined technique was used. Two days before the operation, a slag-free diet was prescribed from 2:00 p.m. During these days, unlimited fluid intake was allowed. The patient took 30 ml of the drug in the evening 2 days before surgery and 120 ml of the drug diluted in 1 liter of water the evening before the operation. In 10 (58.8%) patients the tumor was localized in the rectum, in 3 (17.6%) - in the rectosigmoid junction, in 4 (23.6%) - in the colon. At the same time, the lesion of the intestine by the tumor along the circumference was circular in 7 (41.2%) patients. The tumor occupied less than 1/2 of the circumference in 6 (35.2%) patients, more than 1/2 in 3 (17.6%) people. In one patient, the tumor was previously removed with the formation of a preventive colostomy and preparations were made for surgery to close the colostomy. In one case, the tumor was complicated by subcompensated intestinal obstruction; the remaining patients had an uncomplicated course of the disease. The above-described preparation method allowed patients to perform the following operations: extraperitoneal closure of the colostomy - 1 patient, extirpation of the rectum - 4 patients, other radical operations with the formation of an intercolic anastomosis - 8. In 2 cases of tumor localization in the lower ampullary section, it was possible to perform a sphincter-preserving operation - abdominal anal resection of the rectum with reduction of the sigmoid colon into the anal canal. Hartmann's operation was performed in one case due to the presence of subcompensated intestinal obstruction. Poor preparation (presence of liquid feces and air in the intestine) was observed in 3 cases, good preparation (when the intestinal lumen is opened, there is no intestinal content) - in 13 (81.3%) cases. In one case, due to the diagnosis of an acute gastric ulcer, surgical intervention was postponed and, thus, it was not possible to monitor the quality of preparation. In the postoperative period, no purulent-septic complications were observed. In one patient, the postoperative period was complicated by acute myocardial infarction, which was associated with the presence of concomitant pathology. All patients note the good organoleptic properties of Duphalac. When using it, there were no side effects or exacerbation of concomitant chronic diseases. Conclusions 1. The most commonly used preparation of the colon for surgical interventions, including a waste-free diet and mechanical cleansing, allowed sphincter-preserving operations to be performed in 74.4±6.9% of patients with rectal cancer; the frequency of purulent-inflammatory complications was 24.1±6.8%. 2. With the help of the “X-prep” drug, the colon was satisfactorily prepared for instrumental studies in 70.3±7.5% of patients with colorectal cancer. 3. When preparing the colon for operations for colorectal cancer with the drug Duphalac, good preparation was in 81.3±9.4% of cases; there were no purulent-septic complications; all patients noted the good organoleptic properties of the drug.
Literature 1. Astashov V.L., Loginov A.F. Optimization of intestinal preparation of severe and elderly patients for colon studies and surgical interventions // Pharmateka. – 2003, No. 1. – P. 30–32. 2. Belyakov N.A. Enterosorption in preparing patients for operations on the colon // Vestn. hir. – 1989. – T. 142, No. 2. – P. 30–33. 3. Vorobyov G.I. Preparation of the colon for operations using the method of general lavage: Recommendation method. – M., 1988. – 20 p. 4. Demerchyan E.A. Optimization of diagnostic and treatment methods for patients with obstructive colonic obstruction: Abstract of thesis. dis. E cand. honey. Sci. – Kharkov, 1992. – 18 p. 5. Colorectal cancer: Preparation of the colon for surgery / M.D. Khanevich, M.A. Shasholin, A.A. Zyazin. – M.: MedExpertPress; Petrozavodsk: Inteltek, 2003. – 136 p. 6. Kokhnyuk V.T., Yudin A.A., Ospischev A.A. Preparation of the intestine for operations in patients with colorectal cancer / Current problems in oncology and medical radiology: Collection of scientific works. works – Minsk: Research Institute of Oncology and Medical Radiology named after. N.N. Alexandrova, 2000.– pp. 177–184. 7. Popova I.S. Comparative assessment of methods for preparing the colon for surgery: Abstract of thesis. dis. E cand. honey. Sci. – M., 1988. – 24 p. 8. Cancer of the colon and rectum /Ed. IN AND. Knysha. – M.: Medicine, 1997. – 304 p. 9. Hammer HF, Sana Ana GA, Schiller LR, Fordtran JS Studies of Osmotic Diarrhea Induces in Normal Subjects by Ingestion of Polyethylene Glycol and Lactulose. J. Clin. Invest 84 (1989) 1065–1062. 10. Schumann C. Darm–Mykosen. Behandlung durch Regulation des Okosystems Darm. Die PTA in der Apotheke 25 (1996) 168–171.