Surgical treatment of gastric and duodenal ulcers is considered one of the most controversial issues in modern medicine. The fact is that this method of combating these diseases, although highly effective, is fraught with the development of numerous complications. Therefore, many specialists in the treatment of ulcerative lesions of the gastrointestinal tract prefer conservative therapy. However, in some cases, surgical intervention simply cannot be avoided.
What are ulcerative lesions of the digestive system?
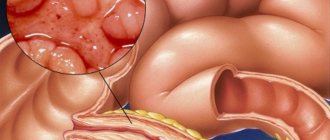
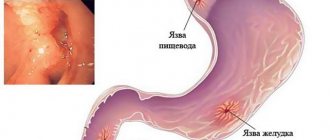
Peptic ulcer is a chronic disease that manifests itself in the form of ulcerative lesions of the mucous membranes of the stomach and duodenum. The pathology is quite widespread. According to statistics, up to 10% of the population suffers from peptic ulcers. Moreover, in most cases it affects young, able-bodied people aged 20 to 40 years.
The disease significantly worsens the patient's quality of life and has an extremely negative impact on his overall health. Stomach and duodenal ulcers are accompanied by severe pain, nausea, vomiting and heartburn. In the absence of adequate therapy in an advanced form, the disease can lead to such serious consequences as perforation of the gastric and intestinal walls, perforation, penetration, and the development of internal bleeding that poses a danger to the patient’s life. That is why ulcerative lesions of the gastrointestinal tract need to be treated promptly and competently.
Allowed drinks and foods, methods of cooking, postoperative diet rules
A sample menu after surgery for a perforated gastric or duodenal ulcer includes gentle, carefully selected and properly prepared foods. 5-6 meals a day in small portions are organized.
All products are prepared:
- steamed;
- boil;
- baked;
- or stewed.
For easy digestion, food should be liquid, semi-liquid, very soft or pureed. Also, it facilitates the work of the digestive organs by following the rules of separate nutrition, when one product or certain types of products are consumed at one meal, and others at another.
Postoperative nutrition includes the following drinks, foods, and dishes:
- green, herbal teas;
- milk (tea with milk);
- fruit drink, compote;
- jelly;
- porridge with milk or water (oatmeal, or pureed buckwheat, rice, semolina);
- soft-boiled eggs without oil, steamed omelet;
- light vegetable soups, cream soups;
- milk soups;
- pureed vegetables (pumpkin, potatoes, carrots);
- skim milk, cottage cheese, sour cream and other non-acidic dairy products;
- dietary meat (chicken, rabbit, turkey), broths from them;
- steamed cutlets and zrazy from dietary meat, fish or vegetables;
- lean fish;
- low-fat cheeses;
- fruit jellies;
- soufflés, mousses from permitted products;
- homemade pate;
- dried premium bread, biscuits.
Tea can be sweetened a little, preferably with honey.
For seafood, cod, hake fillet, gobies and other dietary fish are suitable. During the first time after surgery, fresh vegetables and fruits are not included in the patient’s diet. But their subsequent use will contribute to faster rehabilitation of the patient.
In order not to provoke increased secretion of the stomach, fruits should not be sour and rough. You can eat bananas, pears, melons, and sweet apples. Soups and purees can be prepared using potatoes, carrots, pumpkin, zucchini, and beets.
Oatmeal, rice, and buckwheat porridge occupy a large place in the diet after surgery for a perforated stomach or duodenal ulcer. For desserts, you can have various jellies, soufflés, and mousses made from permitted products.
Since fresh baked goods are prohibited, bread is consumed dried. The use of a small amount of natural vegetable oil or butter is allowed. The permissible salt intake is up to 6 grams per day.
The rules of postoperative nutrition relate not only to the correct selection of products, but also to the regimen. It consists of 5-6 meals a day in small portions. Such crushing also reduces the load on the mucous membranes and prevents dangerous stretching of their cavities, especially in the first time after surgery.
Based on the above, the diet for a perforated gastric or duodenal ulcer is formed in accordance with the following rules:
- using only approved products and cooking methods;
- small meals (6 times a day);
- It is unacceptable to overeat and drink large amounts of liquid at once;
- food should be warm, within 15-60°C;
- food should be soft (liquid, semi-liquid, puree);
- You need to chew food thoroughly to grind it and soak it with saliva.
To comply with all dietary standards, the most convenient option is home cooking.
Indications for surgery
Among the indications for surgical treatment of ulcers, gastroenterologists identify the following factors:
- degeneration of the ulcer, development of a malignant process;
- gastric polyposis;
- frequently recurring cases of exacerbation of the disease;
- severe course of peptic ulcer with accompanying complications;
- lack of effectiveness of conservative treatment methods;
- goalie stenosis;
- metaplasia of the gastric mucosa;
- large sizes of foci of ulcerative lesions;
- presence of recurrent bleeding;
- numerous ulcers of the gastrointestinal tract;
- gastric deformities of a cicatricial nature;
- violations of the evacuation function of the stomach;
- individual intolerance by the patient to certain components of medications used to treat peptic ulcer disease;
- pyloric stenosis;
- frequent cases of relapse;
- suspicion of malignancy;
- a sharp deterioration in the patient’s health, loss of ability to work;
- gastric deformities;
- the presence of giant ulcers, the diameter of which exceeds 3 cm;
- pyloric ulcer;
- The patient's age is over 50 years.
It is worth noting that surgical intervention is much more often indicated for ulcerative lesions of the stomach rather than the duodenum.
Contraindications for surgery
Surgical intervention for ulcerative lesions has a fairly narrow range of contraindications, which usually include the following:
- the presence of serious diseases and pathologies of internal organs;
- thrombocytopenia (reduced blood clotting);
- decompensation of the functioning of internal organs;
- respiratory failure;
- heart attack;
- acute stroke;
- esophagitis;
- pregnancy;
- alcoholism in chronic form;
- presence of mental illness;
- heart failure;
- the presence of distant cancer metastases;
- renal pathologies.
However, all these contraindications are considered to be relative, and in the case of serious complications that threaten the patient’s life, they are limited to exceptional situations in which, according to experts, the risk of surgical intervention is extremely high.
The essence of surgical treatment
Surgical treatment for gastric and duodenal ulcers involves organ-saving operations or the use of radical resection techniques. The choice of type of operation is determined by a specialist surgeon individually in each case. This takes into account factors such as the age and general health of the patient, the presence of complications and concomitant diseases, the form and stage of the course of the peptic ulcer, the size of the ulcerative lesions, etc.
During the operation, doctors are aimed at excision of the ulcerative lesion, eliminating the pathology that causes the development of associated complications, and reducing the level of gastric secretion. At the same time, it is extremely important that the treatment entails as few side effects and complications as possible, which also largely depends on the level of skill and qualifications of the surgeon.
Classification and features of implementation
Depending on the patient’s condition and the degree of development of the lesion, the doctor decides which operation to perform. There are several types of interventions, which require their own characteristics in preparation and implementation, and also require certain surgeon skills. The classification is based on several factors:
With the radical nature of the intervention, the cause of the pathology is completely eliminated.
- Nature of the intervention: radical - complete elimination of the cause of the pathology;
- palliative - partial elimination of the provoking factor;
- symptomatic - relief of manifestations of pathology.
- emergency - immediately after diagnosis;
- one-stage;
There is also the concept of “re-operation”, which can be done after the recovery period, after the previous one, and there is a simultaneous intervention, which involves performing several surgical techniques simultaneously. Each of the varieties follows a specific algorithm and involves a characteristic rehabilitation.
Gastric resection
This is a complete abdominal surgery, which is considered particularly traumatic. Such intervention is carried out only if the stomach cannot be restored by other methods. Modern technology has been significantly simplified. Typically, resection is performed when gastric cancer develops or benign tumors appear. Such treatment occurs in several stages:
- Inspection of the peritoneum and determination of the possibility of surgery.
- Cutting off the gastric ligaments and giving the organ mobility.
- Removal of the necessary part of the stomach.
- Connection of the organ stump and intestines.
Gastric resection can be of two types:
- Complete - removal of more than 90% of the organ.
- Partial – excision of part of the stomach; distal resection – removal of the lower third of the organ for a non-infiltrative tumor;
- proximal type - surgery for neoplasms that do not grow into the serosa.
Ulcer surgery
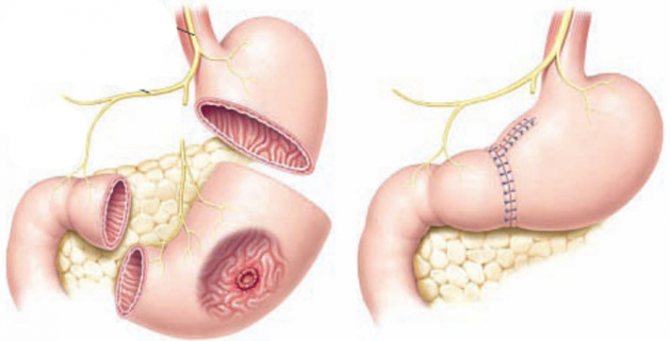
In most cases, proper care and drug treatment can get rid of the pathology without the intervention of surgeons. However, if the decision to treat the disease in this way is unsuccessful, they resort to surgery. To prevent recurrence of the disease, the antral and pyloric sections of the organ are removed so that ¼ of the stomach remains.
This type of stomach removal is outdated. For removal, low-traumatic interventions are performed that affect the cause of the pathology.
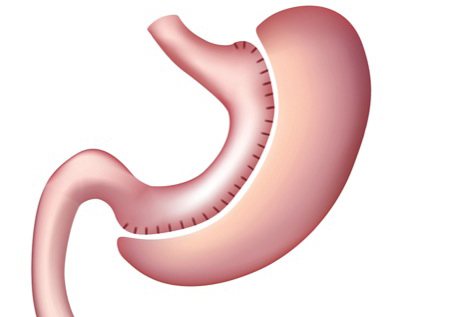
Obesity surgery
If the body weight is excessive, the patient is prescribed longitudinal resection or “sleeve” removal. The intervention involves cutting off most of the organ, preserving the gastric valves after surgery. This event allows you to reduce the volume, but does not disrupt the digestive process. This technique reduces appetite by excision of the area that produces the corresponding hormone.
Radical surgery for cancer
If the patient's condition and diagnostic results indicate the presence of a malignant neoplasm in the gastric cavity, complex, multi-stage operations are performed. If the pathology starts, complete removal of the organ will be required - gastrectomy. This type of intervention is more difficult than resection, since the stomach, lymph nodes and omentum are excised. Radical operations for stomach cancer require strict lifelong adherence to strict nutritional rules.
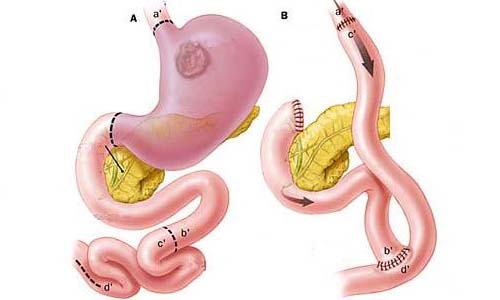
Gastroenterostomy
In case of contraindications to resection, patients are prescribed this type of operation. It involves the formation of an anastomosis between the gastric cavity and the small intestine. The goal is to relieve stress on the organ and speed up the evacuation of food. Despite this, such an intervention is possible only if there are no other options due to the large number of complications.
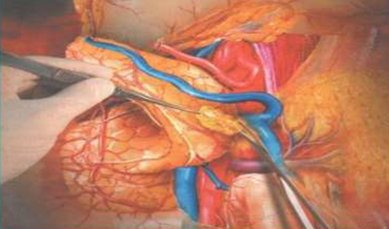
Vagotomy of the stomach
This type of intervention is an innovative approach to the treatment of ulcerative organ damage. The operation involves excision of the vagus nerve, which provides impulse transmission for increased acid production. After surgery, the acidity level decreases and the ulcers go away. Vagotomy was first performed in 1911, and it came into surgical use in 1946.
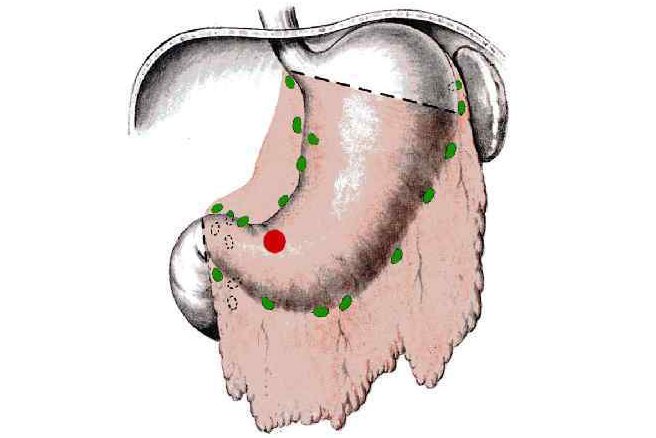
Lymph dissection
It is often performed when tumors appear. The technique is used to remove lymph nodes and adjacent adipose tissue, in order to eliminate channels for feeding the tumor. Lymph node dissection can be performed as a separate surgery or as part of a complete or partial gastrectomy. The operation has two types - D1 (excision of gastric nodes) and D2 (removal of distant formations).
Laparoscopy
Laparoscopic surgery is performed if the patient has a hernia or cancer. Laparoscopy of the stomach is a low-traumatic intervention that involves several small incisions and insertion of an endoscope into the abdominal cavity to obtain a magnified image. The hernia or tumor can be removed partially or along with the organ.
Types of surgical treatment
Modern medicine for the treatment of gastrointestinal ulcers offers the following types of surgical intervention:

- Vagotomy is an operation that is a surgical dissection of the so-called branch of the vagus nerve, which is responsible for the process of stimulating gastric secretion. With this type of surgical intervention, the natural process of transition of gastric contents into the cavity of the duodenum is disrupted, resulting in the connection of the stomach with the small intestine.
- Resection today is considered one of the most effective techniques used in the treatment of peptic ulcer disease. This type of surgical intervention involves excision of individual areas of the gastrointestinal tract affected by ulcerative lesions. Postoperative recovery takes about a year.
- Local excision is a surgical intervention to remove foci of ulcerative lesions surgically. This technique is characterized by a reduced degree of trauma, but it only eliminates the consequences of the disease without fighting its cause, which leads to frequent cases of relapse.
- Palliative suturing of an ulcer is usually used in case of perforation. During the operation, the abdominal cavity is cleaned of its contents, followed by suturing of the ulcerative lesion with a seromuscular suture in a transverse direction relative to the gastric axis.
- Gastroenterostomy is an operation to create a so-called gastrointestinal anastomosis. In this case, a channel is created connecting the stomach with the small intestine, which serves to pass food bypassing the duodenum and the pylorus.
Resection for obesity
With a high degree of obesity, in some cases longitudinal resection is prescribed. The procedure is sometimes called sleeve removal. The operation cuts off most of the stomach, but preserves the physiological valves. As a result, the volume of the organ decreases, but the digestion process is not disrupted. The stomach no longer looks like a muscular sac, it looks like a narrow tube with a volume of about 150 ml. There is a dramatic weight loss and a decrease in the feeling of hunger, since the zone that produces the hormone responsible for this feeling is removed. Longitudinal resection allows you to lose up to 60% of excess weight, while no foreign objects such as a balloon or band are placed in the stomach. This method of treating obesity can be used at any age.

Preparing for surgery
Preoperative preparation for gastric and duodenal ulcers involves conducting a series of medical and diagnostic studies. These include:
- electrocardiogram;
- general blood analysis;
- X-ray of the stomach;
- Analysis of urine;
- esophagogastroduodenoscopy with taking material for biopsy;
- X-ray of the esophagus and duodenum;
- computed tomography of the gastrointestinal tract;
- carrying out analysis to determine the concentration of lipids and fats;
- ultrasound examination of the liver;
- chest x-ray;
- conducting a study to determine parathyroid hormones.
Prohibited Products
The prohibited list includes many products. They usually have a negative impact on digestion and create excess stress on the gastrointestinal tract, and can also cause excessive production of hydrochloric acid.
Therefore, any junk food is excluded from the diet for a perforated stomach ulcer. But you should also avoid the following products:
- boiled and fried eggs;
- various sauces, mayonnaise;
- fatty meat broths and soups made from them;
- spices, seasonings;
- confectionery;
- baked goods, fresh bakery products;
- instant products (fast food);

- salted crackers and nuts, seeds, chips;
- sausages;
- alcohol-containing and sweet carbonated drinks;
- grape;
- salo;
- mushrooms;
- legumes;
- citrus;
- cabbage;
- garlic;
- sorrel;

- canned food;
- kvass, coffee, strong tea;
- sweets, ice cream.
Advice! It is necessary to avoid fruit juice and cocoa drinks. It is better to replace them with medicinal mineral water without gas, for example, Essentuki, Borjomi.
Refusal to prepare dishes from the listed products will help shorten the rehabilitation period after radical therapy.
Possible complications
Surgical treatment of ulcerative lesions of the stomach and duodenum has a higher degree of effectiveness compared to conservative therapy.
However, cases of the development of a number of postoperative complications are quite often observed. The most common ones include:
- hypoglycemic syndrome;
- food allergies;
- anastomositis;
- anastomotic narrowing;
- pancreatitis;
- scar deformities;
- hepatitis;
- enterocolitis;
- development of dumping syndrome - rapid throwing of food into the intestines from the gastric cavity;
- alkaline reflux gastritis;
- bleeding.
Surgical treatment of gastric and duodenal ulcers, despite possible complications, is today considered the most effective way to combat this pathology, bringing favorable results in 85-90% of cases. With a competent approach, the correct choice of type of operation and a sufficient level of qualifications of the surgeon, all possible risks are minimized.
Menu examples for the day
The following sample menu after surgery for a perforated ulcer is used two weeks after surgical suturing of the perforation. It is compiled based on the above rules. Namely:
- only acceptable products;
- permitted methods of preparation;
- compliance with rules and diet.
Despite all the restrictions, the patient’s diet is quite varied and, most importantly, provides the body with the necessary elements. Thus, the menu for the day might look like this:
Three breakfast options:
- steamed omelette, skim milk or yogurt;
- oatmeal with soft-boiled egg, biscuits, tea with milk;
- milk porridge from pureed rice, compote.
Second breakfast options:
- light chicken broth, green tea (can be sweetened with honey);
- vegetable cream soup, dietary fish zrazy, fruit drink;
- fruit jelly, rose hip decoction.
Lunch options:
- mashed potatoes with soft chicken cutlets, warm milk;
- pumpkin porridge, steamed beef cutlets, fruit and berry jelly;
- Lean fish soup with unleavened biscuits, compote.
Second lunch:
- lean beef broth with vegetables, dried white bread, jelly.
- low-fat turkey soup, fruit puree, fruit drink;
- viscous oatmeal soup, baked pumpkin, tea.
Afternoon snack options:
- milk cream soup, biscuits, tea with milk;
- pureed buckwheat porridge, fish in jelly, herbal tea;
- pumpkin and carrot puree, low-fat cottage cheese with sour cream, biscuits.
Three dinner options:
- mashed potatoes with a little butter, steamed vegetable zrazy, warm milk;
- cod soup with finely chopped vegetables and a small amount of herbs, crackers, berry juice;
- beef broth, homemade pate, dried bread, jelly.
Tea should not be strong, jelly sour or too sweet, dairy products only low-fat, low-fat broths, dietary meat and fish, premium bread, dried or in the form of crackers, a minimum of salt. Try to eat at the same time with intervals of 2.5-3 hours, but no more than 4 hours.
Not all possible dishes and dietary products are presented here after surgery for a perforated ulcer, but from the examples presented, a general picture of the selection of products and their preparation can be seen. Based on this, you can further diversify the patient’s menu.
Thus, after a successful operation, the patient’s further recovery depends on following a diet. But even after the recovery period, in order to avoid relapse, do not forget about the main principles of a healthy diet.