Epidemiology
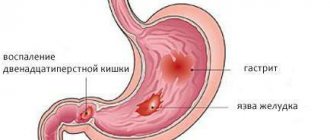
An ulcer of the duodenal bulb is usually secondary to damage to the gastric mucosa. Therefore, the diagnosis usually writes “stomach and duodenal ulcer”, without specifying the location.
About 5% of all people on Earth have this pathology. In men it occurs 4 times more often than in the fair sex. And the ratio of city dwellers to rural residents is approximately 2 to 1. Most likely, this is due to the quality of products, eating habits and work activities of residents of urbanized areas.
Causes
An ulcer of the duodenal bulb occurs due to the corrosive effect of hydrochloric acid (which is part of the digestive juice) on the mucous membrane of the small intestine. There are several reasons that cause an increase in acidity:
- excessive release of gastrin (a hormone that regulates digestion);
- passion for spicy, bitter, salty, sour, fried and fatty foods;
- insufficient food intake during the day and overeating in the evenings;
- long-term use of hormonal or anti-inflammatory drugs;
- regular exposure to stress;
- smoking and drinking alcohol, especially on an empty stomach.
In rare cases, the appearance of erosions and ulcers in the duodenum may be associated with an increase in calcium levels in the body, decreased liver and kidney function, and chronic obstructive pulmonary diseases.
Symptoms and treatment of scar deformation of the duodenal bulb
Cicatricial deformation of the duodenal bulb is a residual form of the main pathological process associated with a severe form of erosion or ulcer of the corresponding localization of the base organ.
What are the additional reasons for the formation of such a structure? How is it detected and diagnosed? How effective is non-surgical treatment? You will read about this and much more in our article.
Reasons for the development of the pathological process
The duodenum, which is the initial section of the small intestine and located after the pylorus of the stomach, consists of several elements. The key is a bulb or ampoule that has longitudinal folding.
As part of various pathological processes and the formation of an inflammatory reaction on the mucous membranes of the organ, a partial change in the structure of the epithelium occurs, resulting in the creation of preconditions for the formation of scars.
Such deformations usually clearly indicate a partially or completely healed ulcer, but may also indicate other causes of pathology. The most famous:
- Incoming deformation against the background of severe edema due to the inflammatory process of the entire duodenum,
- Physical compression of the bulb due to the influence of external or internal factors - injuries, features of the anatomical structure of the patient’s neighboring organs, and so on,
- Systemic pathological processes affecting the gastrointestinal tract complex. In the latter case, scarring of the duodenal bulb is a secondary complication.
Symptoms of scar deformation of the duodenum
The symptoms of scar deformation of the duodenum are not specific and depend on the severity of scarring and its type, the presence of secondary provoking circumstances that form the prerequisites for exacerbation of the process.
In general, during the remission stage, the problem practically does not manifest itself, especially if the scarring is minor.
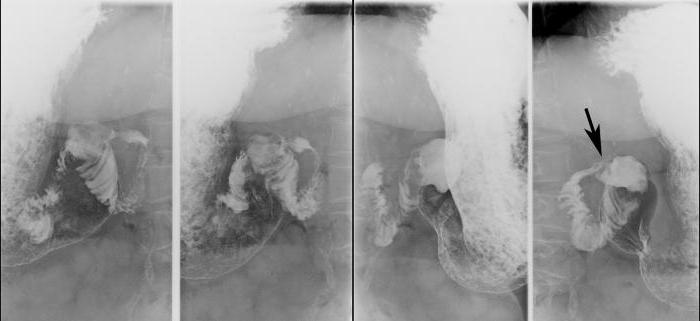
In this context, during instrumental examination, asymmetry of the bulb is observed, caused by partial shortening of one of its contours, but the lumens of the organ are open, and the evacuation of the contents proceeds normally.
Primary, externally diagnosed signs are characteristic of moderate and severe deformities with the formation of diverticulum-like protrusions, “trefoils” within the framework of cicatricial convergence with a narrowing of the lumen up to 50% or more, a parallel slowdown in the function of evacuation of biological contents up to 1 day or more.
In this context, the following manifestations are possible:
- Pain in the upper abdomen radiating to the back and neighboring organs. The pain syndrome intensifies with prolonged fasting and at night,
- The appearance of belching , nausea, increased gas formation and intestinal discomfort, and other broad-spectrum dyspeptic disorders,
- Staining of vomit and feces with bloody inclusions, indicating the start of internal bleeding - such a symptom directly threatens the patient’s life and requires his immediate hospitalization in a hospital and intensive care unit.
In addition, a relapse of the ulcerative pathological process against the background of organ structures weakened by cicatricial deformations sometimes leads to partial or complete blocking of the passage to the pylorus, where hydrochloric acid for the stomach is located.
Ultimately, this causes the substance to enter the intestine with subsequent migration of pancreatic bile fluids through various parts of the gastrointestinal tract, contributing to the development of a complex pathological acute process.
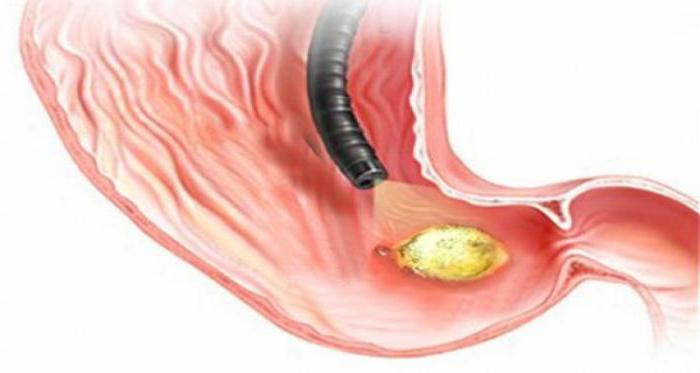
Diagnosis of pathology
Determination of the primary and final diagnosis of cicatricial and ulcerative deformation of the duodenal bulb 12 is carried out comprehensively based on the results of laboratory instrumental studies. The main activities include the following procedures:
- X-ray examination with the introduction of barium-based contrast to assess the degree of evacuation function,
- Ultrasound of the duodenum. Allows you to assess the condition of the bulb in general terms,
- Penetrating fibrogastroduodenoscopy. The most informative, but invasive endoscopic technique,
- Other activities as necessary.
In parallel with the implementation of basic instrumental procedures, laboratory diagnostics are prescribed:
- General analysis of stool and blood,
- Blood biochemistry,
- Gregersen analysis,
- Other studies as necessary.
The main specialized specialist who makes the appropriate diagnosis based on anamnesis and objective data is a gastroenterologist.
Treatment of scar deformity of the duodenal bulb
After determining the main diagnosis, the gastroenterologist prescribes individual treatment, including complex measures:
- Drug therapy,
- Diet,
- Preventive actions.
After the main inflammatory process has been removed, the rationality of performing surgical intervention to eliminate scar structures within the framework of classical surgery is considered.
Such measures are relevant in case of relapses of the pathological process, advanced forms of scar deformities, and the presence of a number of complications.
As part of pharmaceutical treatment, painkillers and anti-inflammatory drugs , agents for improving peristalsis, corticosteroids, and colloidal solutions that restore mucous membranes are prescribed.
In addition, symptomatic treatment is carried out, eliminating the most unpleasant manifestations of the underlying ulcerative pathology and secondary cicatricial deformities of the duodenal bulb.
Various physiotherapeutic procedures are prescribed for the second time , including electrophoresis, UHF, balneological treatment, ozokerite applications and other actions as necessary. They are carried out after the acute phase of the problem has resolved.
Self-prescription for scar-inflammatory deformation of the duodenal bulb 12 of any medications, various procedures, including the use of folk recipes introduced into the main treatment regimen without the prior approval of a gastroenterologist, is strictly prohibited!
Correction of the power plan
In most cases, in the absence of complications and multiple relapses of the pathological process, diet shows high effectiveness in moderate and advanced forms of cicatricial deformation of the duodenal bulb (DU). Correction of the diet begins with the exclusion of the heaviest foods that are prohibited for consumption in case of ulcers and deformities of the organ bulb. Completely prohibited:
- Any type of alcohol
- Rye bread,
- Fatty fried foods
- Pickles and smoked meats,
- Canned food and marinades,
- Rich broths.
Spices, sweets, coffee, and tea are consumed with great restriction.
Under additional control are any foods and dishes that can significantly affect the acidity of the stomach, cause intestinal hyperactivity, or, conversely, significantly slow down its work.
The list of general recommendations includes split meals - you need to eat more often, but in small portions.
It is allowed to steam, boil, or, in extreme cases, bake. Food is served only warm. The consistency of the products is small pieces, paste-like and liquid (large pieces are not allowed).
Possible complications
Cicatricial deformation of the duodenal bulb often causes complications, especially in the presence of predisposing circumstances. The most common problems:
- Relapse of the ulcerative process. Observed on average in a quarter of patients, even when they undergo full-fledged treatment 3-6 months after therapy,
- Blockage of the duodenum. It is formed in the case of advanced forms of scar deformities, with the development of an extreme pathological process. Leads to systemic spillage of bile/hydrochloric acid throughout the gastrointestinal tract, requiring hospitalization,
- Bleeding. Caused by a violation of the integrity of the mucous membranes and epithelial structures in the localization of scars. Requires first aid and qualified treatment in a hospital with hospitalization of the patient.
- Secondary manifestations. Dyspeptic disorders that do not disappear for weeks and months, induction of the development of irritable bowel syndrome, and so on.
Preventive actions
As part of basic preventive measures aimed at preventing the development of scar-ulcerative deformation of the duodenal bulb or the progression of the pathological process after healing of the ulcer, it is recommended to perform the following actions:
- Full completion of the rehabilitation period. It includes drug therapy, physiotherapy, a special regime,
- Dieting. The adaptive nutrition system must be adhered to on an ongoing basis, until the final disappearance of all signs of pathology, including those confirmed by diagnostic measures,
- Rejection of bad habits. First of all, we are talking about alcohol consumption and smoking,
- Moderate physical activity. If there is deformation of the duodenal bulb, active physical activity is contraindicated, however, light cardio training is acceptable and recommended,
- Regular preventive examinations. Includes a visit to a gastroenterologist, laboratory tests, ultrasound, fluoroscopy, and other procedures as necessary.
Source: https://MedTelo.ru/travmy/simptomy-i-lechenie-rubtsovoy-deformatsii-lukovitsy-dpk.html
Pathogenesis
An ulcer of the duodenal bulb manifests itself in a wave-like course with alternating remission and exacerbation. Conventionally, three stages are distinguished:
- acute course (symptoms are pronounced, there are ulcers and erosions on the mucous membrane);
- attenuation of the process (no complaints, ulcers are scarred);
- remission (no symptoms, scars are epithelialized).

The main role in the appearance of ulcers is played by a violation of the acid-base balance on the intestinal mucosa. If more hydrochloric acid is formed than alkali, it is not completely neutralized and damages surrounding tissues. Cells break down, release enzymes and increase damage. In this area of the mucous membrane, inflammation forms, which intensifies with each new portion of chyme. In addition, increased peristalsis and an increase in the number of secretory cells in the stomach allows acid to be secreted even outside of meals.
Treatment
Treatment of patients with cicatricial deformation of the duodenum is surgical. Significant importance is also given to preoperative preparation, which includes measures aimed at normalizing motor skills and restoring metabolic disorders.
First of all, regular gastric lavage is indicated. Taking into account the level of hypochloremia, hypokalemia, azotemia, metabolic alkalosis, hypoproteinemia, intravenous infusions of polyionic solutions and protein hydrolysates are performed:
- To correct the water-electrolyte composition, an isotonic solution is administered.
- To restore carbohydrate metabolism, 10-20% glucose is used.
- Normalization of protein balance is achieved by using plasma, proteins, and albumins.
- Cardiac glycosides are prescribed to stabilize the functioning of the cardiovascular system.
- Vitamins B, C, K are indicated for hypovitaminosis.
Peptic ulcer disease is dangerous due to the development of severe consequences. The morphological changes in the structure of organs that arise in this case are irreversible and lead to increased functional disorders. A healthy lifestyle, proper nutrition, absence of bad habits, minimizing stressful situations - all this significantly reduces the likelihood of signs of the disease and its complications.
Symptoms
How does a duodenal bulb ulcer manifest itself? Its symptoms and treatment are closely related, so it is important to understand which syndrome is prevalent. The clinical phenomena are very intense and cause a lot of inconvenience to the patient.

The very first and main symptom is pain in the umbilical area. It can be either acute or aching, it all depends on the quantity and quality of meals. In addition, at first it is easy to get rid of it by drinking antacids. Sometimes the pain may return at night and radiate to the lower back.
Every ulcer sufferer knows: to get rid of nausea, belching or pain, you just need to have a snack. Preferably something like jelly. But this remedy is not universal, because vomiting can return after eating, “bringing” with it heartburn and a feeling of heaviness as a “bonus”. From time to time, these people suffer from bowel problems in the form of constipation and flatulence.
Complications
Acute ulcer of the duodenal bulb is a life-threatening and health-threatening disease. In severe cases, severe bleeding, perforation of the intestinal wall and the formation of sepsis are possible.
An ulcer can not only corrode the wall of a hollow organ, but also leak into the adjacent one. For example, from the duodenal bulb the pathological process moves to the pancreas, forming fistulas and abscesses.
Chronic complications include stenosis (narrowing) of a section of the intestine. This makes it difficult for food to pass through, causing it to stagnate and rot in the stomach. In humans, this manifests itself as a feeling of heaviness, weakness, pallor, exhaustion, and lack of appetite. In some cases, there may be vomiting with pieces of undigested food eaten several days ago.
Why is deformation dangerous?
Cicatricial deformation of the duodenal bulb is not normal; digestive function is impaired.
As a result, the patient will have a feeling of discomfort and pain, will suffer from diarrhea or constipation, and belching. But the worst complication is a decrease in the intestinal lumen. Due to scar deformation, the intestinal passage narrows significantly, and the food bolus gets stuck in the stomach.
There are compensated and decompensated intestinal obstruction. In the first case, that is, if the obstruction is compensated, the intestinal passage narrows significantly, but is not completely blocked, so it can partially cope with its work.
If this is decompensated patency, the diameter of the lumen is less than 0.5 cm or it is absent. Such a patient urgently needs surgery.
Diagnostics
An ulcer of the duodenal bulb is diagnosed quite easily, given that patients seek help from a doctor already at the height of the disease, when discomfort prevents them from living normally.
First, the doctor collects anamnesis and conducts an examination. Of course, palpating the abdomen does not provide much information, but it is possible to suspect, with a high degree of probability, an ulcerative process. Then the patient is sent for a blood test, biochemical markers, a stool test for occult blood, and gastrin levels and Helicobacter pylori activity are determined.
The most common diagnostic procedure remains esophagogastroduodenoscopy, or, more simply, endoscopy. It allows you to examine the mucous membrane of the digestive tube, cauterize all identified ulcers, and take tissue and fluids for examination. Radiography is also informative. Images with contrast will clearly show the location of the ulcers and the condition of the gastric and duodenal mucosa.
Treatment of duodenal bulb ulcer
First of all, you need to prepare yourself for the fact that this is a long and painstaking process, consisting of diet, physiotherapy and medication. Don’t be alarmed; all this needs to be done not at the same time, but according to a clearly developed plan and in consultation with a doctor.
To begin with, the gastroenterologist determines the cause that caused the ulcer and directs all efforts to get rid of it. There is drug therapy for this. These include antacids, prokinetics, proton pump inhibitors, and many other pharmacological wonders. In addition, mild sedatives and sleeping pills can help in the fight against stress ulcers, but they should be used with caution. Penicillin antibiotics and macrolides work well against Helicobacter pylori.
At the recovery stage, to maintain the strength of the body, the patient is recommended to undergo balneological procedures, novocaine electrophoresis and warming.
Folk remedies
Treatment of duodenal bulb ulcers with folk remedies is fraught with unpleasant health consequences. Therefore, before starting this kind of experiment, warn your doctor. He will be grateful to you for this.

On the Internet, as well as from our grandmothers, there are many recipes for treating ulcers. In order to reduce acidity and increase mucosal resistance, people drink fresh potato juice, a mixture of honey and butter, or simply dissolve honey in warm water and consume it before meals. There are also more exotic recipes, for example, using a teaspoon of sea buckthorn seed oil before each meal.
All these methods can remove discomfort, some even promote the healing of ulcers, but preference should still be given to traditional methods of treatment.
Prevention
Not everyone is ready to undergo surgery, but other treatment for narrowing the lumen will not help. Those who want to avoid surgery should treat the ulcer, since bulb deformation is always a complication of this disease. What exactly should be done?
- Take all medications prescribed by your doctor.
- Avoid heavy physical labor and active sports.
- Walk outdoors more often.
- It is better to avoid stress and take calming pills.
- It is necessary to give up bad habits, that is, do not abuse alcohol, do not smoke.
- Diet is very important. The patient should eat frequently, every 3 hours, eating only warm cooked or steamed foods.
- In autumn and spring, when a recurrence of the disease is possible, be examined by a doctor.
Proper treatment of a duodenal ulcer will help avoid such a serious complication as deformation of the duodenal bulb. It sometimes leads to intestinal obstruction, which the doctor can only cure with surgery. It is worth taking care of yourself even before complications arise, since later it will be difficult to establish normal functioning of the gastrointestinal tract. Even the best doctors cannot yet perform miracles, and no expensive drugs can restore your lost health.