The human body is susceptible to various diseases. Diseases can affect any internal organ. The duodenum is no exception. The most famous ailment of this part of the digestive system is peptic ulcer. Many people associate it with the stomach, but in fact it is associated with more than just that. The duodenum is quite often involved in the pathological process. What is this disease? What other diseases can affect the duodenum? Before looking for answers to these questions, it is worth considering the structure of the named section of the digestive system.
Structure of the duodenum
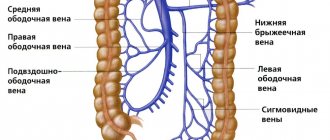
The human digestive system is complex. One of its components is the duodenum. It is considered the initial section in the small intestine. The duodenum originates from the pylorus of the stomach and ends at the duodenojejunal flexure, which passes into the next section of the small intestine (the jejunum).
The duodenum contains several components:
- the upper part, the length of which is from 5 to 6 cm;
- the descending part, which is 7–12 cm in length;
- horizontal part, which is 6–8 cm in length;
- the ascending part, equal in length to 4–5 cm.
SRS2. Hormones of the stomach and duodenum: physiological significance, regulation of secretion.
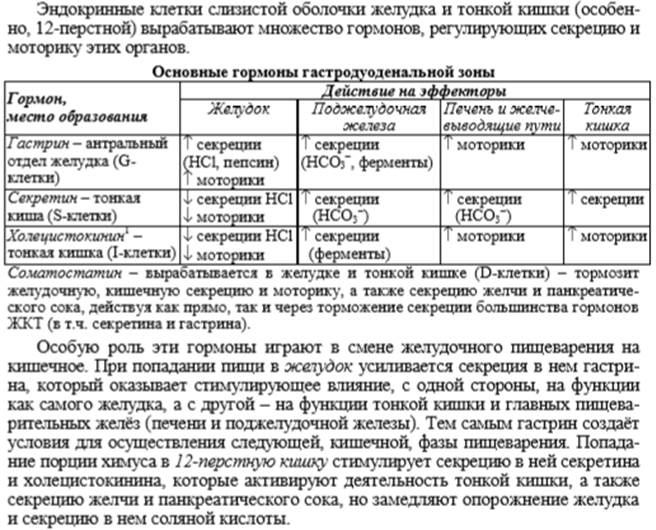
Below is a brief description of the most studied gastrointestinal hormones.
Gastrin
secreted by cells of the antrum of the stomach, duodenum and upper jejunum;
also found in the central nervous system. There are 6 known molecular forms of the hormone, of which gastrin-17 and gastrin-34 predominate, consisting of 17 and 34 amino acid residues, respectively. The release of gastrin is stimulated by food intake and distension of the stomach. Inhibition of the secretion of this hormone occurs when the gastric contents become acidic. The main physiological effect of gastrin is stimulation of the secretion of hydrochloric acid and pepsin, as well as regulation of the trophism of the stomach, duodenum and pancreas. Normally, the gastrin content in the blood reaches 120 ng/l.
Severe hypergastrinemia is observed in Zollinger-Ellison syndrome (see
APUD system
)
,
less pronounced in atrophic gastritis, pernicious anemia, duodenal ulcer, after vagotomy, as well as in liver and kidney failure. A fragment of the gastrin molecule, pentagastrin, is used as a stimulator of hydrochloric acid secretion in studying the secretory function of the stomach.
Cholecystokinin
produced in the small intestine, also found in the central nervous system. It is involved in the release of pancreatic enzymes and bile after eating. There are 3 known molecular forms of cholecystokinin, which are peptides consisting of 39, 33 and 8 amino acids. Cholecystokinin-8 has the greatest biological activity. Cholecystokinin preparations are used in cholecystography and assessment of the enzyme secretory function of the pancreas.
Secretin
is produced in the mucous membrane of the duodenum and is a peptide consisting of 27 amino acid residues. Its secretion is stimulated by acidification of the duodenal contents and inhibited by alkalization of the duodenal contents. The main physiological effect of secretin is to stimulate the secretion of water and bicarbonate from the pancreas. Hormone preparations are used in laboratory assessment of the external secretion of the pancreas.
Vasoactive intestinal peptide
(VIP) is produced in the small intestine, found in the central nervous system and in neurons throughout the gastrointestinal tract, and consists of 28 amino acid residues.
Under physiological conditions, it stimulates the secretion of water by the pancreas and intestines, suppresses the formation of hydrochloric acid by the cells of the gastric mucosa, relaxes the smooth muscles of blood vessels, the gall bladder, and part of the esophagus. Hyperproduction of VIP is noted in Werner-Morrison syndrome, ganglioneuroblastomas (see APUD system
) and dumping syndrome (see
Postgastroresection syndromes
)
.
In megacolon and Chagas disease, atrophy of VIPergic neurons of the intestine was detected.
Gastroinhibitory polypeptide
(GIP) is produced primarily in the duodenum and jejunum and consists of 42 amino acid residues. The secretion of GIP is stimulated by the entry of lipids, glucose and some amino acids into the duodenum. Normally, GIP potentiates glucose-stimulated insulin secretion.
Enteroglucagon
Produced primarily in the ileum and colon, it is involved in the regulation of intestinal trophism. It is a polypeptide consisting of 69 amino acid residues. The secretion of this hormone is stimulated by lipids and carbohydrates from the intestinal contents. Severe overproduction of enteroglucagon is observed in glucagonomas, celiac disease, malabsorption syndrome, cystic fibrosis, dumping syndrome and after resection of the distal parts of the small intestine.
Pancreatic peptide
(PP) is found predominantly in the tissue of the pancreatic islets and consists of 36 amino acid residues. PP secretion is stimulated by food intake. In physiological concentrations, PP inhibits exocrine pancreatic secretion, bile secretion, and gastrointestinal motility. A decrease in PP production is noted in chronic pancreatitis and cystic fibrosis of the pancreas. In most cases, high concentrations of PP are found in the blood of patients with pancreatic apudoms.
Gastrin - releasing hormone
found in the stomach, upper part of the small intestine and central nervous system. It is a peptide consisting of 14 amino acid residues. Under physiological conditions, it stimulates the secretion of hydrochloric acid and gastrin. It is believed that this hormone is a mediator of physiological gastrin stimulants.
Somatostatin
produced in the antrum of the stomach, in the tissue of the pancreatic islets, central nervous system. There are two known molecular forms of this hormone - somatostatin-14 and somatostatin-28, which consist of 14 and 28 amino acid residues, respectively. Somatostatin suppresses the secretion of insulin, glucagon and other gastrointestinal hormones; when administered intravenously, it inhibits motility, the secretion of digestive juices and slows down blood flow in the gastrointestinal tract. It is produced in increased quantities by somatostatinomas and other pancreatic apudoms. Synthetic analogues of somatostatin are used in complex therapy of gastrointestinal bleeding of various origins, as well as to inhibit gastrointestinal motility during instrumental studies. The creation of long-acting somatostatin preparations makes its use promising for the treatment of acromegaly, diabetes mellitus, and apuds of the gastrointestinal tract.
Motilin
synthesized in the mucous membrane of the small intestine, consists of 22 amino acid residues. The release of motilin is triggered by food intake. The main effect of this gastrointestinal hormone is to increase gastrointestinal motility. Increased levels of motilin in the blood are found in diarrhea of infectious origin, Crohn's disease, ulcerative colitis, and dumping syndrome.
Neurotensin
synthesized in the small intestine, found in the central nervous system. and pancreatic apud tissue. This is a peptide consisting of 13 amino acid residues. The secretion of this gastrointestinal hormone is stimulated by fatty foods. The physiological role is not well understood. Neurotensin drugs cause vasodilation, contraction of smooth muscles, inhibition of gastric secretion and motility.
Functions of the duodenum
The duodenum performs several important functions:
- It begins the process of intestinal digestion. The food coming from the stomach is brought here to an alkaline pH, which does not irritate other parts of the intestine.
- The duodenum regulates the production of bile and pancreatic enzymes depending on the chemical composition and acidity of food coming from the stomach.
- The initial section of the small intestine also performs an evacuation function. From it, food gruel coming from the stomach is sent to other parts of the intestine.
Digestion in the duodenum
As soon as food enters the duodenum, both the pancreas and liver immediately “know” about it. The tiny intestinal glands, which also produce digestive secretions, “learn” about this.
This brings the entire gastrointestinal tract into working position and ensures efficient digestion.
As soon as food begins to move further into the duodenum, a whole “bouquet” of digestive enzymes falls on it.
Here, careful mechanical and chemical processing of food takes place. Almost all substances are broken down: proteins, fats, and carbohydrates.
There are two types of glands in the duodenum
The first are located at the beginning of the duodenum. They are a transitional option between the gastric and intestinal glands.
The second ones are located in the final part of the duodenum and along the entire surface of the small intestine.
What provides the juice of the intestinal glands?
- Neutralizes acid that enters the intestine from the stomach along with the food bolus
- Intestinal juice contains a lot of mucus, which lubricates the intestinal wall, preventing damage and facilitating the passage of the bolus.
- It also activates some pancreatic enzymes
- And finally, it takes part in the breakdown of proteins, fats and carbohydrates
Some diseases that may be associated with the duodenum
One of the diseases that occurs in the duodenum is duodenitis. This term refers to inflammatory-dystrophic changes in the mucous membrane. They arise due to exposure to harmful factors on the body: food poisoning, toxic substances that cause poisoning when they enter the digestive system, spicy foods, alcoholic beverages, foreign bodies. With duodenitis, pain is felt in the epigastric region, nausea, vomiting, weakness, and body temperature rises.
Diseases of the duodenum also include chronic duodenal obstruction. This is a process that leads to disruption of passage through the duodenum, that is, motor and evacuation activity in this part of the digestive system is disrupted. The disease occurs for many different reasons (for example, the presence of tumors, congenital anomalies, etc.). Signs depend on the reasons that caused chronic duodenal obstruction, on the stage of the disease and on how long the duodenum has been affected. Sick people experience symptoms such as discomfort and heaviness in the epigastric region, heartburn, loss of appetite, constipation, gurgling and transfusion in the intestines.

Where is the duodenum located and how does it hurt?
If a person has been diagnosed with inflammation of the duodenum, symptoms and treatment depend on the causes that provoked the disease.
A disease involving inflammatory processes in the duodenum is called duodenitis. The inflammatory process is provoked by gastritis, cholecystitis, and pancreatic diseases.
Taking these factors into account, the doctor selects appropriate drug therapy.
Causes of inflammation of the duodenum
Before treating the duodenum, it is important to find out the causes of the disease.
Most often, the onset of the disease is associated with the production of high concentration gastric juice, which comes from the stomach. It causes severe irritation and serious inflammation.
Duodenitis may appear due to poor passage of undigested food in the duodenum, which accumulates in its upper section. This is due to decreased tone of the organ. Food masses begin to irritate the mucous membrane, causing infection and inflammation.
Duodenal disease develops for the following reasons:
- due to food poisoning;
- due to alcohol abuse;
- with frequent consumption of marinades and spicy foods;
- if mechanical damage to the mucous membrane occurs;
- with hepatitis;
- cholecystitis;
- with Crohn's disease;
- if blood circulation is impaired;
- for chronic diarrhea;
- with neoplasms in the gastrointestinal tract.
Duodenitis is provoked by a bacterial infection of the duodenum, if the cause of gastritis and stomach diseases is Helicobacter pylori. Bacteria actively multiply in gastric juice with high acidity, since such microflora is an ideal environment for reproduction.
If treatment is not timely, microorganisms will soon provoke a pre-ulcerative condition, which over time develops into a duodenal ulcer.
Symptoms
As the disease develops, the patient does not even suspect where the duodenum is located and how it hurts.
And only over time the following signs are observed:
appetite disorder appears;
- there are disruptions in digestion;
- there is discomfort in the stomach;
- the patient complains of belching, bloating;
- Vomiting or nausea may occur.
This symptom occurs more often in women; - pain and spasms are felt;
- possible pain at night;
- there are severe hunger pains;
- the symptom of semolina in the intestine is pronounced;
- during a diagnostic examination, the bulb is irritated;
- the intestinal mucosa is hyperemic;
- blood may be excreted in the stool;
- anemia is observed;
- the patient often experiences a feeling of weakness;
- a person has diarrhea due to duodenitis;
- There is a feeling of liquid splashing in the stomach.
If duodenal disease is not detected, an ulcerative process begins, mucosal hyperemia is observed, and pathological changes occur in the gastrointestinal tract.
Diagnosis of inflammation of the duodenum
Before figuring out what to do and what drug therapy to prescribe for duodenal disease, the doctor refers the patient to undergo diagnostic procedures.
- An ultrasound is prescribed to identify pathologies of organs, their changes and the presence of formations.
- EGD is the main procedure that allows you to examine the gastrointestinal tract for the presence of inflammatory processes and pathological changes in the duodenum.
- X-rays using a contrast agent can reveal defects in the digestive system.
- The patient may be prescribed an endoscopy with the collection of biomaterial to identify the tumor.
- Taking gastric juice will allow you to study the acidity and composition.
- If a duodenal infection is suspected, a Helicobacter pylori test is performed.
- Using a coprogram, stool is examined.
- The patient undergoes a general blood test and an antibody test.
Classification
Duodenitis is divided into several types, which differ in the presence of the pathogen, the course of the disease and the location.
According to etiology, duodenitis is divided into 2 types:
- Acute, in which the symptoms of duodenal disease are pronounced. Signs of the disease appear unexpectedly and have a short course.
- Chronic duodenitis lasts for many years. With this form, the symptoms are mild and appear in most cases due to other pathologies of the digestive system.
Depending on the location, duodenitis can be:
- Diffuse with multiple inflammatory foci in the duodenum.
- Local with minor inflammation that resembles papillae on the walls of the duodenum.
According to the depth of the lesion:
- Superficial, in which swelling or hyperemia is observed.
- Interstitial, which affects the deep layers of tissue.
- Atrophic, when the mucous membrane is absent or its severe thinning is noticeable.
- Erosive, which is characterized by wounds and erosions on the walls of the duodenum.
Drug treatment
Painkillers –
Medicines can relieve attacks of pain. The most recommended are:
- Papaverine;
- No-shpa;
- Drotaverine.
Antacids –
Designed to restore acidity:
Enveloping tablets –
They are prescribed to protect the mucous membrane of the duodenum and stomach. Effective are:
Antibiotics –
If Helicobacter is present, the following is prescribed:
Motility stimulating –
Medicines help increase intestinal motility:
Anticholinergics –
Allows you to reduce or completely eliminate unpleasant sensations. These include:
Antacids and enterosorbents –
They have protective properties, protecting the duodenal mucosa from damage. These are drugs such as:
Anti-inflammatory –
They have a healing effect and have an anti-inflammatory effect:
Dopamine blockers –
Eliminate vomiting and improve motor skills:
Sedatives –
Medicines that have a sedative effect:
- Valerian;
- Sedavit;
- Tozepam;
- Phenozepam.
Physiotherapy for duodenal inflammation
The use of physiotherapeutic procedures will help cure the disease. This method is used when duodenal disease is not in the acute phase.
Most often, the doctor recommends the following activities:
- ultrasound treatment;
- magnetic therapy;
- diadynamic therapy;
- warming up with the use of drugs in the epigestral zone.
ethnoscience
Folk remedies can be used in children and during pregnancy.
1. Pick 2-3 lower leaves of aloe, which is at least 3 years old. Grind the leaves, add 250 g of red wine and 500 g of honey to the mixture. Place the mixture in a glass container and mix everything. Leave for 10 days. Take a teaspoon after meals three times a day. The course of treatment is 3 months.
2. Buy propolis tincture at the pharmacy. Before meals, add 15 drops to warm milk and drink. Treatment is carried out for 2-3 weeks.
3. Peel the potatoes and grate them. Squeeze the juice and drink it a teaspoon at a time if you feel pain.
4. Sea buckthorn oil has a powerful wound healing effect. It must be drunk three times a day.
Treatment of duodenitis and chronic duodenal obstruction
Treatment of diseases must be prescribed by a doctor. In order for the duodenum to restore its functions during duodenitis, the following measures may be required:
- fast for 1 or 2 days;
- gastric lavage;
- prescription of a special diet (No. 1, 1a, 1b);
- prescription of astringents, enveloping, antacid, antispasmodic, anticholinergic, ganglion-blocking agents, vitamins;
- in some cases, surgery and antibiotic therapy are required.
In case of chronic duodenal obstruction, treatment of the duodenum requires an individual approach. If the disease is caused by a mechanical obstacle, then surgical intervention is performed. In other cases, prokinetics may be prescribed. These drugs have a stimulating effect on the muscles of the gastrointestinal tract, increase contractile activity, tone of the stomach and duodenum, and make the evacuation of gastric contents faster.
Features of digestion
The breakdown of fats occurs in the duodenum.
Digestion in the duodenum is a rather complex process in which the duodenum plays an important role.
The entry of food gruel into the initial part of the small intestine is observed. Here it is joined by fluid that comes from the pancreas.
The secretions of the intestinal walls and bile are added to the gruel. At the next stage, the acidic environment of the food coma is neutralized by bile. As a result, the acidic contents do not negatively affect the walls of the digestive tract.
Bile has a positive effect on the process of emulsification and breakdown of fat, resulting in the formation of an emulsion. This leads to an increase in the area of interaction between fats and digestive juice enzymes. As a result, there is an acceleration of the process of digesting food.
Thanks to bile, fat breakdown products dissolve in the duodenum. This also ensures their complete absorption into the intestinal walls. Bile plays a fairly important role and has a positive effect on the process of absorption in the intestines of such elements as:
- Amino acids;
- Fat-soluble vitamins;
- Calcium salts;
- Cholesterol.
A fairly important function of bile is that it regulates intestinal motility. Bile contracts the intestinal muscles, which speeds up the movement of food through the intestines. After completing all functions, bile is excreted from the body almost completely.
The duodenum also receives pancreatic juice from the pancreas. This is a clear liquid that is used to digest various food components - fats, starch, proteins. Since it is influenced by other enzymes, it is activated in the intestinal cavity.
If the duodenum is affected by its own glands, this leads to the formation of intestinal juice. It contains mucus in large quantities, as well as the enzyme peptidase, which breaks down proteins. With the help of these glands, two types of hormones are produced - secretin and cholecystokinin-pancreozymin. With their help, the secretory function of the pancreas is enhanced, which leads to the regulation of its work.
The process of digestion in the duodenum is quite complex. That is why the organ must always be in working condition.
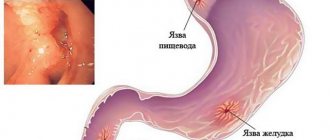
What is meant by peptic ulcer?
When considering diseases of the duodenum, special attention should be paid to peptic ulcers. This term refers to a serious disease that occurs in a chronic form with alternating periods of remission and exacerbation. The etiology of this disease is not well understood. Previously, it was believed that peptic ulcers were caused by substances such as pepsin and hydrochloric acid, which were produced in the digestive system. However, studies have shown that the microorganisms Helicobacter pylori play an important role.
Statistics show that the prevalence of duodenal ulcer ranges from 6 to 15%. It cannot be said that a representative of a particular gender gets sick less often or more often. Men and women are equally susceptible to this disease.
Possible diseases
Peptic ulcer is a very serious disease of the duodenum.
The duodenum is able to fully perform its functions only if it is completely healthy.
Read: Structure of the abdomen: abdominal organs and methods of examining the abdominal cavity
Today, there are a huge number of diseases to which this organ can succumb. Diseases of the duodenum can be of both inflammatory and non-inflammatory nature.
Among inflammatory diseases, patients most often develop duodenitis. In some cases, the development of bacterial or fungal infections in the form of actinomycosis and tuberculosis may occur. In most cases, these infections come from other organs. A serious consequence of duodenitis is peptic ulcer.
The duodenum can be affected by erosive and ulcerative diseases. Quite often they are accompanied by pathological processes in the liver. In this case, diseases of the cardiovascular system and respiratory organs can also be observed.
Quite often, patients experience gastric ulcers. It occurs against the background of stressful situations, poor diet, smoking, and the use of medications. In spring, the disease most often worsens. In fairly rare cases, diseases of a tumor nature are observed in the duodenum, which can be benign or malignant.
The duodenum is a very important organ of the digestive tract. It is characterized by a complex structure, which allows it to perform very important functions. Complete digestion in the duodenum can only take place if it is completely healthy. That is why, when the first symptoms of diseases of this organ appear, patients should seek help from a doctor.
What are the symptoms of a duodenal ulcer, you will learn from the video:
https://www.youtube.com/watch?v=w8RxI47fXwU&t=683s
Read along with this article:
- Small intestine: length and role in the digestive process
- The length of the human rectum, its age characteristics
- What are the differences between the parts of the small intestine?
- Digestive processes that occur in the small intestine
- Anatomy of the human intestine: what's what
- Human small intestine: anatomy, functions and process...
- The work of the pancreas. A special role and significance for everything...
- What is the length of the adult intestine, its features and functions
- Human intestine: intestinal length, general information, features...
Features of duodenal ulcers
Ulcers are lesions of the duodenum. They can be compared to erosions. However, there are significant differences between these two types of damage. Erosion affects only the mucous membrane that lines the duodenum. The ulcer penetrates into the submucosal and muscular layers.
Research shows that ulcers are found in the upper part in most cases. They are localized near the pylorus of the stomach. The diameter of the damage varies. Most often there are ulcers in which this parameter does not exceed 1 cm. In some cases, large ulcers are found. Doctors in their practice encountered injuries to the duodenum that reached 3–6 cm in diameter.
Stomach and duodenum
The stomach is an organ of the digestive system, bordering in its upper (initial) part with the esophagus, and in its lower part with the duodenum.
The stomach ensures the accumulation of food, its initial digestion and partial absorption, and the evacuation of contents in the duodenum. The stomach is located in the upper part of the abdominal cavity. The shape and volume of the stomach are not constant.
They change depending on the state of its muscle tone, its filling, the phase of digestion, body position, as well as the condition of nearby organs.
Conventionally, there are 4 parts of the stomach: the cardiac part, the body of the stomach, the fundus (vault) and the pyloric (pyloric) part, which, in turn, is divided into the antrum (pyloric cave) and the pyloric canal. The duodenum is directly adjacent to the stomach and is the initial section of the small intestine.
In a healthy adult, the duodenum has an average length of 30 cm and is horseshoe-shaped. There are 4 parts of the duodenum: the upper, or bulb, descending, lower horizontal and ascending.
In the descending one there is the papilla of Vater (major duodenal papilla), which is formed from the fusion of the common bile and pancreatic ducts, and the minor papilla, on which the accessory pancreatic duct opens. The lower horizontal part is covered by the peritoneum and is in contact with the inferior vena cava, aorta and pancreas. The ascending part passes into the small intestine.
The wall of the stomach is formed by the gastric mucosa, submucosal layer (submucosa), muscular and serous membranes. The gastric mucosa consists of a single-layer columnar epithelium, a layer of its own, represented by loose connective tissue, and a muscular plate.
The lamina propria contains tubular gastric glands, in which there are 3 types of cells: main cells, secreting pepsinogens and chymosin; parietal (parietal), secreting HCI and gastromucoprotein; accessory cells (mucocytes) that secrete mucoid secretions.
The pyloric glands contain hormonally active cells that secrete gastrin, etc.
The mucous membrane of the duodenum is covered with columnar epithelium, has villi, between which there are intestinal crypts, in which the mucous duodenal (Brunner's) glands open, producing a viscous alkaline secretion.
The mucous membrane also contains endocrine cells (Kulchitsky cells), which produce gastrointestinal hormones (secretin, cholecystokinin, etc.).
The duodenum, together with the stomach, pancreas, liver and its biliary system (biliary system), plays an important role in ensuring the secretory, motor and evacuation functions of the digestive tract.
The formation of intestinal enzymes in the duodenum itself begins in the crypts, and continues and ends on the surface of the villi of the mucous membrane, i.e. the entire mucous membrane of the duodenum is a glandular apparatus.
The mucous membrane of the duodenum produces kinasinogen, which activates enterokinase, which converts trypsinogen (proenzyme) into trypsin (active enzyme), secretes secretin, which stimulates pancreatic secretion, bile-forming function of the liver, bile secretion and other hormones.
The secretory activity of the stomach and duodenum is regulated by nervous and humoral mechanisms.
The stomach and duodenum are characterized by tonic, peristaltic, pendulum-like contractions and rhythmic segmentation.
Against the background of diseases and, obviously, age-related evolution, atrophic changes occur in the mucous membrane of the stomach and duodenum, accompanied by a decrease in hormonal and enzymatic activity of the stomach and duodenum.
Continuous secretion of gastric mucus is important in the formation of the so-called protective mucous barrier. In this case, the destroyed glycoproteins are restored due to their synthesis by constantly renewed mucus-forming cells.
Excitation of adrenergic and cholinergic receptors, insulin, serotonin, prostaglandins, secretin, and local mechanical irritation of the gastric mucosa have a stimulating effect on production. Some medications (acetylsalicylic acid, etc.) have an inhibitory effect on the formation and secretion of mucus.
Gastric mucus, integumentary epithelium, bicarbonates, prostaglandins and other factors form a protective barrier of the mucous membrane, which turns out to be ineffective, mainly due to active inflammation.
Source: https://gastroweb.ru/Zheludok/index.html
Clinical manifestations of peptic ulcer
In some people, the disease proceeds unnoticed, while in others, duodenal ulcer manifests itself with suspicious signs. The most commonly observed symptoms are:
- recurrent pain localized in the upper abdomen;
- digestive disorders;
- deterioration in a sick person’s appetite and weight loss;
- tarry stools;
- bleeding that occurs due to gastric juice corroding the walls of the blood vessel;
- pain in the back (they occur due to the growth of an ulcer into the pancreas);
- intense abdominal pain (they are observed when an ulcer perforates or peritonitis develops).
Of these symptoms, the most common is pain. It can be different in nature - sharp, burning, aching, vague, dull. Pain usually occurs on an empty stomach (in the morning after waking up). They can also appear after eating in about 1.5–3 hours. Unpleasant sensations can be relieved with antacid medications, food, and even a glass of milk or warm water. The fact is that when foods and drinks enter the body, they partially neutralize the effects of hydrochloric acid. However, after a short period of time the pain returns again.
Enzymes in the duodenum
These are digestive enzymes of the pancreas and intestinal glands.
Pancreatic enzymes:
- lipase, steapsin - break down fats
- amylase - breaks down carbohydrates
- proteases (trypsin, chymotrypsin, carboxypeptidase, elastase, nuclease) - break down proteins
Small intestinal enzymes:
- peptidases (enteropeptidase, alanine aminopeptidase) - continue the breakdown of proteins
- Erepsin - breaks down proteins
- sucrase, maltase, isomaltase, lactase - continue the breakdown of carbohydrates
- intestinal lipase - continues the breakdown of proteins
Diagnostic procedures for peptic ulcer disease
The diagnosis of “duodenal ulcer” cannot be made based only on symptoms and an external examination of a sick person, because the above signs are characteristic of a wide range of diseases. The listed symptoms may hide not only a duodenal ulcer, but also cholelithiasis, stomach cancer, pancreatitis, benign tumors, etc.
A suitable and reliable method for diagnosing peptic ulcer disease is fibrogastroduodenoscopy. During this test, a special instrument with a light source and camera is inserted through the mouth into the stomach to examine the lining of the digestive system. The image is formed on the monitor. The doctor evaluates the stomach and duodenum. Diseases are diagnosed by noticeable pathological changes. If necessary, the specialist takes a sample of the mucous membrane to examine for the presence of microorganisms that provoke the occurrence of peptic ulcers.

Digestion in the duodenum
The duodenum plays a major role in digestion. The main digestive juices pour into it: pancreatic, intestinal and bile; hormones are formed in the intestinal mucosa that regulate the secretion of the stomach, pancreas, and liver; there is a rhythm sensor here that sets the frequency of contractions of the duodenum and small intestine.
To obtain pancreatic juice or bile in its pure form, fistulas of the pancreatic ducts or common bile duct are applied to the dog.
It is impossible to obtain pure pancreatic juice or bile from humans. Usually in clinical practice, a mixture of duodenal juices is obtained using duodenal intubation. For this purpose, a thin probe with a metal olive at the end is inserted through the mouth into the duodenum, through which the contents of the intestine flow out.
Composition and secretion of pancreatic juice. Pancreatic juice is a colorless liquid. The reaction of the juice is alkaline, due to the content of sodium bicarbonate (NaHCO3) in it; its pH is 7.3 - 8.7. The juice contains enzymes that digest proteins, fats and carbohydrates, i.e. all the nutrients in food. Under the influence of pancreatic juice enzymes, the breakdown proceeds to the final products of digestion, i.e., to products suitable for absorption and assimilation by the cells of the body. Protein-digesting enzymes (trypsin and chymotrypsin) act, unlike pepsin, in an alkaline environment and break down the protein molecule into amino acids. The juice contains lipase, which is responsible for the main digestion of fats, breaking them down into glycerol and fatty acids; amylase and maltase, which break down complex carbohydrates into monosaccharides; a nuclease that breaks down nucleic acids. Pancreatic secretion is regulated by neural and humoral pathways.
Pancreatic juice begins to secrete 2 - 3 minutes after the start of a meal. Irritation of oral receptors by food reflexively excites the pancreas. Further separation of juice is supported by irritation of the duodenal mucosa with food gruel and hydrochloric acid of gastric juice. Under the influence of mechanical and chemical stimuli, active hormones are formed in the mucous membrane - secretin and pancreozymin, which are then absorbed into the blood, carried by its current to the cells of the pancreas and stimulate its secretion. When negligible amounts of secretin are introduced into the blood, abundant secretion of pancreatic juice is observed. Pancreozymin increases the amount of enzymes in pancreatic juice. Currently, hormones are extracted from the mucous membrane of the digestive tract of cattle and are used in medical practice to stimulate the activity of the human digestive glands.
The duodenal glands are located in the mucous membrane of the duodenum. Their juice contains an enzyme that breaks down protein, and a large amount of mucus - mucin, which performs a protective function. A special enzyme, enterokinase, was also found in the juice, which converts the inactive enzyme trypsinogen in pancreatic juice into the active form - trypsin.
The role of the liver in digestion. Bile is produced by liver cells and enters the intestines through a system of ducts. Part of the bile formed during pauses in digestion accumulates in the gallbladder, where, as a result of the absorption of water, its concentration increases 7-8 times. During digestion, as a result of contraction of the gallbladder, thick gallbladder bile is expelled into the duodenum.
Bile has an alkaline reaction and is colored golden yellow. Bile contains bile acids, bile pigments, cholesterol and other substances. Bile pigment - bilirubin - is formed in the liver from the breakdown products of hemoglobin. Most of the pigment is excreted in the stool in the form of stercobilin, which gives the stool its color. In diseases of the liver and biliary tract (stones, inflammation), in which the release of bile into the intestines is mechanically delayed, the feces become colorless and acquire a putrid odor. In this case, a significant part of the bile from the bile ducts enters the blood, which causes the yellow color of the skin and the white membrane of the eyes. Due to metabolic disorders, bile cholesterol can precipitate in an insoluble state and form stones in the gall bladder and bile ducts. A smaller portion of bilirubin from the intestine is absorbed into the blood and excreted in the urine in the form of urobilin, giving it a certain color.
A person produces 500-1200 ml of bile per day. Its main importance for digestion is that it activates many enzymes and especially lipase of pancreatic and intestinal juices, which in the presence of bile acts 15 - 20 times stronger. By lowering surface tension, bile emulsifies fats, that is, it crushes large drops of fat into tiny balls. This increases the surface area of interaction between enzymes and fat. In addition, bile plays a significant role in the absorption of fats and vitamin K, enhances intestinal movement and, having a bactericidal property, delays putrefactive processes in the intestines.
The process of bile formation and release of bile into the intestine is regulated by the nervous and humoral pathways. The sight and smell of food, the act of eating, the presence of food in the stomach and duodenum reflexively enhance bile formation and the release of bile into the intestine. Humoral irritants of bile secretion are the hormones secretin, gastrin, meat extractives, protein digestion products and bile itself. Bile acids, being absorbed in the intestines, increase secretion. The duodenal hormone cholecystokinin causes contraction of the gallbladder.
Drug treatment of duodenal ulcers
Peptic ulcers can be treated with medication or surgery. In the first method, doctors prescribe drugs to sick people that neutralize hydrochloric acid. They are called antacids. Medicines that help suppress the production of hydrochloric acid in the human body also help with illness. For example, Omeprazole may be prescribed.
If the diagnosis reveals Helicobacter pylori microorganisms, then three-component therapy can be prescribed. Omeprazole or Ranitidine are prescribed in combination with antibiotics (Amoxicillin and Clarithromycin).

Surgery for peptic ulcer disease
When the diagnosis of duodenal ulcer is made too late, surgical treatment is prescribed. It is carried out for certain indications:
- with perforation of the ulcer or heavy bleeding;
- frequent exacerbations of the disease that occur despite drug treatment;
- narrowing of the outlet of the stomach, which arose due to scar deformation of the duodenum;
- chronic inflammation that does not respond to drug therapy.
The essence of surgical treatment is to remove part of the stomach. During the operation, the part of the internal organ that is responsible for the secretion of gastrin in the body is excised. This substance stimulates the production of hydrochloric acid.

In conclusion, it is worth noting that if suspicious symptoms characteristic of diseases of the duodenum occur, you should seek help from specialists at the clinic. Self-medication for ailments is inappropriate, because incorrect drug therapy, its absence or unnecessary folk remedies can cause serious harm to your body and worsen your well-being.
Adjustable
The formation and secretion of pancreatic juice from the pancreas is reflexive and humoral.
Reflex - with the participation of the central nervous system, but the reflex mechanism is less pronounced than in the stomach (with the release of smell, food).
The humoral principle of pancreatic juice formation is more pronounced.
Hormones of the duodenum. 11/24/2000
- these are substances that have biological activity, affecting locally, i.e. on the gastrointestinal tract.
These include enterokinase
, which activates the enzyme
pepsinogen
, converting it into pepsin.
Poliocystokinin
and
pancreozymin
are the same substance, but have dual activity. Activates the activity of the pancreas, enhancing the formation of enzymes and enhances the contraction of the gallbladder - the release of bile into the duodenum → polycystokinin (kinin - moves, in - enhances, it - inhibits).