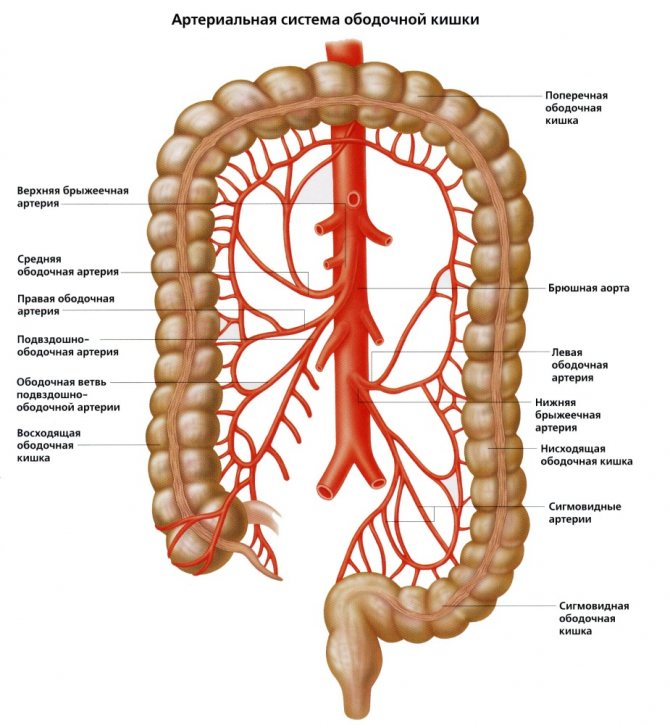
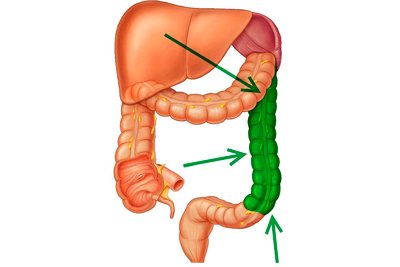
The blood supply to the colon is carried out by various arterial vessels. Vessels from the superior mesenteric artery go to the right part of the colon, and vessels from the inferior mesenteric artery go to the left (Fig. 406). The final section of the colon, i.e., the rectum, is supplied with blood by arteries coming from the inferior mesenteric, internal iliac and internal pudendal arteries.
406. Blood supply of the colon.
1 — mesocolon transversum; 2 - v. mesenterica inferior; 3 - a. mesenterica inferior; 4 - a. colica sinistra; 5—colon descendens; 6 - aa. et vv. sigmoideae; 7 - a. et v. iliaca communis; 8 - a. et v. rectalis superior; 9 - colon sigmoideum; 10 - appendix vermiformis; 11 - caecum; 12 - a. et v. ileocolica; 13 - colon ascendens; 14 - a. et v. Colica dextra; 15 - a. et v. mesenterica superior; 16 - a. et v. colica media; 17 - colon transversum.
The ileocolic artery departs from the superior mesenteric artery to the area of the ileocecal angle, a. ileocolica. It goes from top to bottom, deviating to the right, and lies behind the peritoneum lining the posterior abdominal wall. Its level of origin is located 6-10 cm below the origin of the superior mesenteric artery. Near the ileocecal angle, the ileocolic artery divides into the iliac and colic branches. The first is directed along the upper edge of the ileum and anastomoses with a. ilei, the second goes near the inner edge of the ascending colon. A number of vessels depart from the ileal and colonic branches, which supply blood to the ileocecal angle, cecum, peritoneum, retroperitoneal tissue and lymph nodes of this area.
Artery of the vermiform appendix, a. arrendicis vermiformis , arises from the ileocolic artery. The origin of the artery of the appendix may be located above the division of the ileocolic artery into the iliac and colon branches (the most common option) or at the site of this division. The artery of the appendix can also arise from the iliac or colonic branch, as well as from a. ilei (Fig. 407). The artery of the appendix is first located posterior to the terminal section of the ileum, then passes through the free edge of the mesentery of the appendix and gives off 4-5 branches to it.
407. Diversion options a. appendicis vermiformis.
1 - a. ileocolica; 2 - a. appendicis vermiformis; 3 - ileum; 4 - appendix vermiformis; 5 - caecum.
colon artery goes to the ascending colon , a. Colica dextra . Its origin is located 5-8 cm below the beginning of the superior mesenteric artery. It can also arise from a common trunk with the middle colic or ileocolic artery.
The right colon artery is divided into two branches: descending and ascending. The first of them connects with a branch of the ileocolic artery, forming an arterial arch, from which numerous branches extend to the ascending colon; the second is directed to the mesentery of the transverse colon. Sometimes the right colic artery is absent; in such cases, anastomosis of the ascending branch of the ileocolic artery is performed with a branch of the middle colic artery.
The transverse colon is supplied with blood by several arteries: the middle colon, right colon, accessory middle colon, left colon artery or its branch.
Middle colon artery, a. colica media , departs from the superior mesenteric artery approximately 4-8 cm below its beginning. The accessory middle colic artery also arises from the superior mesenteric artery in most cases.
Most often, the mesenteric bed is formed from two sources: the middle colic artery and the ascending branch of the left colic artery. If the mesenteric bed is formed from three arteries, then in some cases the right and middle colic arteries, as well as the ascending branch of the left colic artery, take part in it, in others - the middle colic artery, the accessory colic artery and the ascending branch of the left colic artery. In Fig. 408 presents options for blood supply to the transverse colon.
408. Options for blood supply to the transverse colon.
1 - colon transversum; 2 - a. colica media; 3 - a. mesenterica superior; 4 - colon descendens; 5 - a. colica sinistra; 6 - a. mesenterica inferior; 7 - a. ileocolica; 8 - colon ascendens; 9 - a. Colica dextra.
The location of the main arterial trunks in the mesentery of the transverse colon is as follows: in the right sector the middle colic artery is most often located, in the middle sector - sometimes the middle colic or accessory middle colic artery, in the left sector - the ascending branch of the left colic artery. The highest concentration of arterial trunks is observed in the right sector of the mesentery, less often in the left and even less often in the middle sector.
Briefly about anatomy
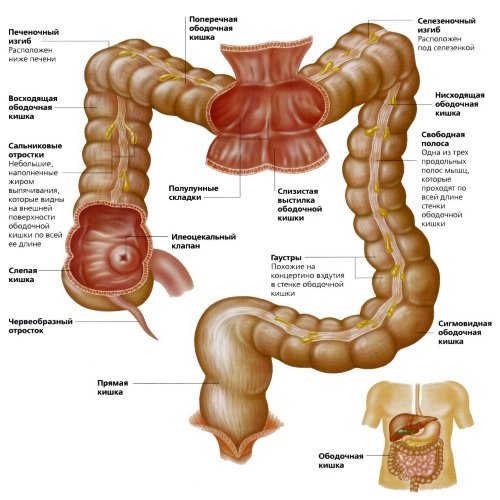
The colon, a photo of which can be found in our article, is the main section of the large intestine and an anatomical continuation of the cecum. The diameter of the department ranges from 5 to 8 centimeters, and its length is 1.5 meters.
There are the following sections of the colon.
Rising
This part of the organ is not involved in digestion, but large amounts of liquid consumed with food are absorbed here. This part of the colon contains liquid chyme, which comes here from the small intestine and is converted into solid feces.
The length of this section is 12-20 cm . The ascending colon is located on the right side of the posterior abdominal wall. The ascending section passes into the transverse colon, the diseases of which will be discussed further.
Transverse
The length of this section is 45-50 cm . Originates on the right side of the hypochondrium.
The transverse colon, the diseases of which will be analyzed, is located so that it is in contact with other organs of the digestive system - the liver, stomach, gall bladder and the tail of the pancreas.
This section has a separate mesentery attached to the mesenteric band.
The hepatic flexure of the colon is located on the left side of the hypochondrium, above the liver. The splenic flexure of the organ, on the contrary, is located lower. The transverse section resembles in its shape a loop located in the projection above or below the navel. The junction of the transverse colon with the descending colon forms an acute angle in the left part of the abdominal cavity .
Descending
The length of this section is 22 cm , and the lumen of part of the organ narrows as it approaches the sigmoid section, which begins with the splenic flexure and continues to the pelvic cavity.
The colonic flexure of the colon has fatty pendants along its entire length. These formations are filled with fatty deposits. The blood supply to the fat pendants is provided by blood vessels passing along the muscular layer of the organ.
Colon: where is it located and how does it hurt?
Not everyone has heard about the colon, but this does not diminish its important role in the digestive system. It consists of transverse, ascending, descending and sigmoid parts. In general, its length can reach one and a half meters, and is curved in the abdominal cavity.
Where is the colon located in humans?
The colon is a part of the intestine that not everyone has heard of, but, nevertheless, this part of the organ plays a huge role in the digestion process.
The colon is the main section of the large intestine. It begins in the area of the cecum and is divided into its parts. The cecum and colon are connected by the Busi sphincter, which ensures the movement of products from one part to another part of the gastrointestinal tract.
On average, the described section of the intestine has a length of one and a half meters, and the diameter of the intestines can vary depending on the characteristics of the patient and is 5-8 cm. Since the colon is one of the largest parts of the large intestine, it has a large number of sections - ascending, transverse, descending and sigmoid.
The first part is not involved in the process of digestion and breakdown of food, but it is in the ascending intestine that the main absorption of water and other liquids occurs.
Liquid stool also passes through it, which gradually turns into solid feces. The section itself is located on the back wall of the abdomen on the right side.
The length of the ascending part varies between patients and can be 12-20 cm.
Structure:
- Ascending, the length of which is 10-25 cm. This is the beginning of the colon, located on the right of the abdominal cavity, and is a continuation of the blind part of the intestine. May vary depending on the position of the person's body. When in a vertical position, its base is directed downward. It becomes transverse, forming the hepatic flexure.
- Transverse - length is 45-60 cm. In its location it comes into contact with the stomach, liver, gall bladder, and resembles a loop in shape. The transverse part forms the splenic flexure. Stretches to the right from the costal cartilage to the left hypochondrium.
- Descending - length varies from 10 to 25 cm. The descending colon is located on the left side of the abdominal cavity. Its continuation is the sigmoid part of the digestive system.
- Sigmoid - length ranges from 20 to 50 cm. The origin is the iliac edge of the posterior crest from above. It forms two loops, one with the convex part down. The second loop is distal, located upward on the psoas muscle. The final part of the colon passes into the rectum.
Causes of development of colon diseases
In order to prevent pathologies of this part of the gastrointestinal tract, you should know what they may be associated with:
- an insufficiently active lifestyle, and this condition is especially dangerous when it is associated with poor nutrition;
- frequent consumption of fatty foods;
- frequent constipation or diarrhea, which can be caused by infection, viruses and other pathogens;
- atonic constipation in patients over 65 years of age;
- accumulation of a large number of toxic substances, most often due to the consumption of low-quality products and frequent constipation;
- the need to constantly take various medications;
- frequent use of unjustified biological additives and laxatives.
Source: https://travmatolog.net/obodochnaya-kishka-gde-nahoditsya-i-kak-bolit/
Functions of the organ
The functions of the colon are:
- the organ ensures the absorption of fluid along with electrolytes, glucose, vitamins and amino acids;
- participates in the breakdown of fiber;
- In this department, feces are formed and then removed from the body.
Important! Dysfunction of the organ affects the functioning of the digestive system, so diseases of the colon and their symptoms require special attention.
ARTERIAL SUPPLY TO THE COLON
Blood to supply the colon comes from the superior and inferior mesenteric branches of the aorta, the large central artery of the abdomen. The ascending colon and the first two-thirds of the transverse colon are supplied by the superior mesenteric artery, and the last third of the transverse colon is supplied by the descending The second colon and the sigmoid colon are supplied by the inferior mesenteric artery.
Diagram of the arteries of the colon
As in other parts of the gastrointestinal tract, there are anastomoses, or connections, between the branches of these two main arteries.
From the superior mesenteric artery depart the ileocolic, right colic and middle colic arteries, which connect with each other and with the left colic and sigmoid obvious branches of the inferior mesenteric artery.
In this way, an “arcade” of arteries is formed around the wall of the colon, supplying all its parts with arterial blood.
Venous outflow of the colon
The venous outflow system of the colon is a mirror image of the artery pattern. The inferior mesenteric vein is a tributary of the splenic vein.
Venous blood from the colon ultimately enters the portal vein. Basically, blood from the ascending colon and the first two-thirds of the transverse colon enters the superior mesenteric vein, and blood from the remaining parts of the colon enters the lower mesenteric vein.
From the inferior mesenteric vein, blood enters the splenic vein, which then merges with the superior mesenteric vein, forming the portal vein. The portal vein then pumps all venous blood through the liver on its way back to the heart.
LYMPHATIC DRAINAGE
Lymph collected from the walls of the colon passes through the lymphatic vessels along the arteries towards the main abdominal vessel for collecting lymph - the chyle cistern. There are many lymph nodes that filter fluid before it is returned to the venous system.
Lymph passes through the lymph nodes on the wall of the colon, through the nodes adjacent to the small arteries, supplying the colon, and then through the nodes of the superior and inferior mesentery.
Diseases
Where is the colon located and how does it hurt? First of all, a person who has inflammation of this part of the organ will feel pain in the lower abdomen and discomfort in the anus .
In addition, other signs of pathology may be observed:
- regular constipation;
- discharge of pus from the anus;
- the presence of blood impurities in the stool;
- flatulence;
- painful urge to defecate;
- loose stool.
If a person has pain in the upper, transverse, descending colon, symptoms of pathology may also indicate iron deficiency anemia . This occurs due to the formation of bleeding ulcers or erosions in the affected organ.
Diseases of the colon occur for the following reasons:
- lifestyle errors: physical inactivity, overeating, abuse of fatty foods;
- hypotension;
- chronic constipation;
- abuse of dietary supplements of dubious quality;
- long-term treatment with antibiotics.
The colon, the symptoms of inflammation of which cannot be ignored, is susceptible to many diseases, including the formation of a malignant tumor .
Hirschsprung's disease
This is a hereditary pathology that manifests itself in a person in infancy or early childhood..
A person with this disease suffers from prolonged constipation, which can last over several weeks.
In this case, enemas and laxatives are useless. However, constipation in Hirschsprung's disease alternates with debilitating diarrhea.
All these disorders of the functioning of the digestive system occur due to ganglion cells of the colon.
The parts of the intestine located above it hypertrophy due to constant contractions , which is why the intestines cease to empty themselves. With this disease, a person is indicated for surgery to remove hypertrophied parts of the organ.
Untimely treatment of the pathology can lead to such serious consequences as intestinal perforation, internal bleeding and even peritonitis.
Diverticulosis
The disease can be either congenital or acquired. Diverticulosis is a disease that is accompanied by protrusion of sections of the intestinal mucosa through its muscular layer . This is accompanied by the formation of sac-like formations in which feces can accumulate, which can provoke inflammation of the organ mucosa.
Typical symptoms of diverticulosis include lower abdominal pain, nausea, diarrhea and vomiting . Ignoring treatment for diverticulosis can lead to such serious consequences as organ obstruction, phlegmon and peritonitis.
Read this article about what diverticula are and how they are treated.
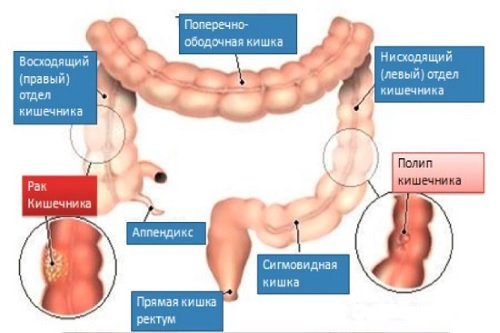
Polyposis
A disease accompanied by the formation of growths on the mucous membrane of the organ , the size of which ranges from a few millimeters to several centimeters.
Polyps are dangerous because they can degenerate into malignant neoplasms, that is, provoke intestinal cancer.
Symptoms of the disease include problems with defecation, since growths in the lumen of the organ interfere with the free movement and exit of feces.
Colon: where it is located and how it hurts
Not everyone has heard about the colon, but this does not diminish its important role in the digestive system.
It consists of transverse, ascending, descending and sigmoid parts. In general, its length can reach one and a half meters, and is curved in the abdominal cavity.
How to recognize that it is she who is hurting? What disease can discomfort be a symptom of? The answers to these questions are in this article.
Structure:
- Ascending, the length of which is 10-25 cm. This is the beginning of the colon, located on the right of the abdominal cavity, and is a continuation of the blind part of the intestine. May vary depending on the position of the person's body. When in a vertical position, its base is directed downward. It becomes transverse, forming the hepatic flexure.
- Transverse - length is 45-60 cm. In its location it comes into contact with the stomach, liver, gall bladder, and resembles a loop in shape. The transverse part forms the splenic flexure. Stretches to the right from the costal cartilage to the left hypochondrium.
- Descending - length varies from 10 to 25 cm. The descending colon is located on the left side of the abdominal cavity. Its continuation is the sigmoid part of the digestive system.
- Sigmoid - length ranges from 20 to 50 cm. The origin is the iliac edge of the posterior crest from above. It forms two loops, one with the convex part down. The second loop is distal, located upward on the psoas muscle. The final part of the colon passes into the rectum.
Causes of colon pain
You can understand that problems have begun in the colon of the intestine by the following signs: discomfort near the anus, pain in the lower abdomen, constipation, flatulence, the presence of blood discharge and pus in the stool. All these symptoms can be the beginning of serious diseases, for which only a doctor can identify and prescribe treatment.
Diseases
- Polyposis.
Polyps or lipomas form on the mucous membrane of the colon. Their sizes range from a few millimeters to several centimeters. The first symptom of the disease is problems with stool, as growths interfere with the passage of stool. Large polyps can cause hemorrhage in the intestinal area. Treatment is carried out surgically or with the help of cytostatic drugs. - Hirschsprung's disease.
This is a hereditary disease that develops in early childhood. The parts of the intestine located above the colon hypertrophy, preventing it from emptying itself. The disease develops as a result of the formation of ganglion cells. The patient is scheduled for surgery to remove the inflamed hypertrophied section. - Diverticulosis.
The disease can be congenital or acquired. It occurs as a result of protrusion of the mucous membrane through the muscle mass of the intestine. Feces get stuck in them, forming inflammation of the organ mucosa. Sometimes a symptom of a disease does not appear for a long time, but sooner or later it makes itself felt. The patient experiences vomiting, diarrhea, and severe pain in the lower abdomen. In the early stages of inflammation, the temperature rises. Treatment is carried out with medication, and if complications develop, in a hospital hospital. - Crohn's disease.
It occurs as a result of immune inflammation on the walls of the gastrointestinal tract, forming fistulas, ulcers and abscesses in the mucous membrane. Crohn's disease is a hereditary and chronic disease, and it can also be triggered by smoking. Antibodies are formed in the mucous membrane, they can ascend and spread throughout the digestive system, as well as in the stomach and esophagus.The patient immediately loses weight, suffers from sharp pain, inflammation in the anus, nausea and bouts of diarrhea. Treatment consists of medication and supportive therapy. During the period of acute development, surgery is prescribed to remove the inflamed area.
Oncological diseases
A tumor in the colon appears as a result of an advanced form of the disease and inflammation. Hereditary predisposition plays a major role. Obesity, a sedentary lifestyle, an unbalanced diet, frequent constipation - all this can be the beginning of the acute development of oncology.
The symptoms are quite similar to other ailments: colic in the lower abdomen, diarrhea, mucus and blood in the stool. As cancer develops, complications worsen. Treatment depends on the forms and stage of the disease. An operation is performed to remove inflammation. If metastases are detected, chemoradiotherapy is prescribed.
- Adenocarcinoma. A common form of cancer. Neoplasms affect the mucous area and organ cells, quickly spreading metastases.
- Signet ring cell carcinoma. The disease is formed as a result of the accumulation of signet ring cells filled with mucus, unconnected to each other.
- Squamous cell carcinoma. The tumor is formed from squamous epithelial cells. Dangerous oncology, high risk of death. This diagnosis is extremely rare.
- Undifferentiated cancer. Oncological formation consists of cells that do not secrete mucus and are not components of the glands. They are separated by connective tissue stroma, forming cords.
- Unclassified cancer. Malignant tumors that do not fit any description of other forms of cancer. Rarely seen.
The meaning and work of the organ
The colon encloses the small intestine. The ascending part occupies the right corner, the transverse part is located at the top of the abdominal cavity, the descending part is on the left, and the sigmoid part is located at the bottom left. Does not participate in the digestion process.
Digested food comes from the small intestine. In the ascending part, the absorption of liquid, vitamins, and microelements begins, gradually forcing it to descend through the remaining parts.
A substance, chyme, is released from the thin section, under the influence of which solid feces are formed.
Examination methods
Constant sharp pain in the lower abdomen and digestive system problems may be a sign of the disease. It is necessary to consult a gastroenterologist who will prescribe examinations. The earlier the disease is detected, the more favorable the outcome of the disease.
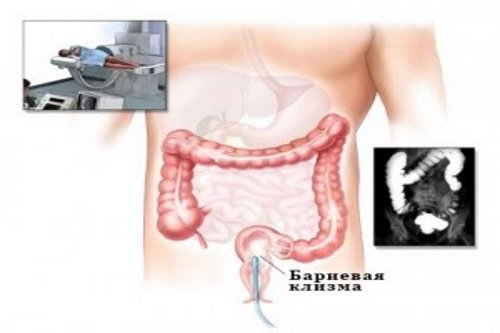
- Irrigoscopy. X-ray, in which the desired section is filled with a suspension. With this study you can detect: fistulas, tumors, ulcers and polyps.
- Colonoscopy. It is carried out using a special apparatus that allows you to examine the intestine from the inside. This is the most accurate research method. During the colonoscopy procedure, you can remove a benign tumor, take a biopsy, remove a foreign object, and stop bleeding.
- Examination with a rectal speculum. The examination is carried out using a rectal speculum, inserting it 10-15 cm into the anus. The examination is not carried out in case of severe pain, inflammation or sphincter spasms.
Disease Prevention
Prevention of diseases of the colon, as well as the gastrointestinal tract, consists primarily of normalizing nutrition.
It is recommended to consume more fiber, plant foods, protein, and enough water.
Minimize the consumption of trans fats, quickly digestible carbohydrates, fast food and other heavy, fatty foods. Obesity also has a negative impact on the digestive tract.
Smoking and alcohol have a negative impact on all systems of the body, including the digestive processes, creating disturbances.
There is also a genetic predisposition to diseases; such people need to be examined twice as often. Older people are also at increased risk.
At the first sign of pain symptoms, visit a gastroenterologist or therapist. He will prescribe the necessary examinations to make a diagnosis and prescribe the correct treatment.
Source: https://GastroTract.ru/simptom/boli/obodochnaya-kishka.html
What is the colon
This is the name given to most of the large intestine. Anatomically, it is divided into several sections: ascending, transverse, descending and sigmoid. The colon begins with the ascending section, which is a continuation of the cecum.

There are several functions of the colon:
- suction;
- excretory;
- protective;
- motor.
The absorption function is the absorption of liquid with electrolytes, vitamins, amino acids, glucose and fatty acids dissolved in it from the chyme formed during the digestion of food. As a consequence of this process, liquid masses form into harder feces.
The excretory function is the release into the intestinal lumen of digestive enzymes, as well as substances excreted from the blood that are unnecessary for the body (metabolites, salts, drugs, toxins).
The protective function is due to various bacteria living on the intestinal mucosa - thanks to them, a solid part of the human immune system is formed.
As for motor activity, it is characteristic of all parts of the intestine - thanks to it, the movement of feces is ensured.
If an inflammatory or other pathological process develops, all functions of this part of the intestine are disrupted with typical manifestations.
Wall structure
Located in the abdominal cavity, throughout the entire length of the wall of the colon are formed by the following layers (membranes):
The mucous membrane lines the inner surface of the intestine. It contains epithelial cells, between which there are a large number of endocrine glands. The glands bend to form crypts. Each crypt contains goblet cells that produce mucus to facilitate the passage of feces. The surface of the crypts is dotted with cells with a set of villi and enzymes for breaking down substances that enter the intestines. The mucous layer also contains blood vessels, clusters of lymphatic plaques (follicles), nerve endings and single muscle fibers. Lymphatic follicles are of great importance in the development of immunity in childhood. Protrusions of the mucous wall increase the absorption surface of the intestine several times.
The submucosa is a connective tissue with a high content of nerve fibers, lymphatic follicles, and blood vessels.
The muscular coat is formed by thick layers of internal muscle fibers (circular layer) and external fibers (longitudinal layer). Nerve plexuses are located between the layers. The longitudinal layer consists of three ribbon strands throughout the entire colon. Between the muscle fibers, the intestinal walls protrude, forming haustra. The haustrae are separated by circular muscle fibers. Contraction of haustra ensures better movement of feces.
The serosa is the outer lining of the colon. There are fatty growths on its surface. The role of the processes is not fully understood.
Colon , like other intestines, each part of the human colon is supplied with blood from a network of arteries.
The arteries of the ascending colon and most of the transverse colon are supplied by the superior mesenteric artery.
The inferior mesenteric artery supplies blood to the descending colon and the left part of the transverse colon.
Venous blood flowing from the colon passes through the hepatic portal system, and then enters the general circulation again.
Symptoms of inflammation
Naturally, the first manifestations of an unhealthy process are disturbances in peristalsis, and, accordingly, in the evacuation of feces. The movement of masses through the intestines slows down, resulting in prolonged constipation. Or vice versa, persistent diarrhea may appear. In any case, intestinal atony develops, which leads to obstruction or other equally serious conditions, often requiring surgical intervention.

Other manifestations of dysfunction depend on the type of pathological process. Experts identify several of the most common diseases.
Small intestine
What's special about this section of the organ? The blood supply to the distal intestine, like its other components, is constantly subject to overload and blood flow disturbances. This is due to the fact that parts of the small intestine are constantly in motion due to the passage of food. The diameter of the intestines changes, which should lead to constant bending of the blood vessels. But this does not happen due to the arcaded arrangement of blood vessels.
The ascending and descending branches of the arteries, arcade by arcade, anastomose with each other. There can be from 4 to 6 such arcades at the end of the small intestine, while at the beginning of the intestine only a first-order arc is observed.
The arcaded blood supply to the intestines allows the intestines to move and expand in any direction. And for various pathologies, it is possible to isolate loops of the small intestine without disrupting the entire blood circulation.
Colitis
This term refers to inflammation of the large intestine, including the colon. The causes of the disease are:
- gross eating disorders;
- infection;
- food or household poisoning.
A provoking factor may be a sedentary lifestyle, metabolic disorders, long-term use of medications, uncontrolled use of dietary supplements, and so on.
Intestinal inflammation can be either acute or chronic, but in both cases the symptoms are similar, the only difference is that in acute colitis the symptoms are more pronounced.
Colitis manifests itself as follows:
- spasmodic pain in the lower abdomen;
- nausea;
- belching;
- unpleasant taste in the mouth;
- progressive weakness;
- weight loss;
- there is blood and mucus in the stool;
- bowel dysfunction (diarrhea or constipation);
- painful urge to defecate;
- Body temperature may rise.
When colitis becomes chronic, flatulence and bloating are added to these symptoms.

Treatment of the colon in this case consists of taking antibiotics (if the inflammation is infectious) and medications that normalize stool. Be sure to drink plenty of fluids - special solutions with electrolytes (for example, Ringer's solution) to replenish the loss of fluid and salts. In the first days, a strict or even starvation diet is prescribed.
Symptoms
Colon cancer has certain clinical manifestations, which depend on the location of the malignancy, the degree of spread of the tumor process and the presence of complications. However, in the early stages of formation they do not appear, which makes it difficult to identify the pathology and reduces the success of treatment.
The left and right sides of this organ have different physiological functions, and therefore react differently to the malignant process. If the tumor has affected the tissues of the ascending colon, then the initial signs are as follows: pain, rumbling and a feeling of heaviness in the abdomen, decreased or complete loss of appetite. Right-sided damage leads to impaired absorption of nutrients, which affects the deterioration of the digestion process.
Colon cancer developing in the descending segment, on the contrary, is not associated with pain. Its main symptoms are constipation alternating with diarrhea, bloating and a feeling of a dense, heavy lump in the left side of the abdominal cavity.
In 1970, A.M. Ganichkin identified 6 clinical forms of development of malignant formation:
- toxic-anemic;
- obstructive;
- enterocolitic;
- pseudoinflammatory;
- dyspeptic;
- tumor (atypical).
The most typical signs of tumor growth in the colon that are noticeable without medical examination are:
Disruption of the normal digestive process. It is characterized by bloating and rumbling in the abdomen, belching, nausea, rarely ending in vomiting, bowel dysfunction (constipation, diarrhea), and loss of appetite.
Painful sensations. Unpleasant discomfort may be felt in the lower abdomen, left or right side. They have a pulling, aching character.
Changes in the characteristics of feces. In addition to structural disturbances, large amounts of mucus appear, and in some cases, blood clots.
Hirschsprung's disease
This is a congenital pathology that is inherited. Its main reason is the absence of ganglion cells in the colon, and they are part of the nervous regulation system of intestinal motility.
With this disease, the child experiences flatulence and constant constipation from the moment of birth (part of the intestine does not work, and, accordingly, fecal stagnation occurs). However, the condition does not improve even with an enema. Constipation may give way to diarrhea. With age, this leads to hypertrophy of the overlying sections of the intestine, and subsequently disturbances in the passage of intestinal contents occur.
Forecast
For colon cancer, when the disease is diagnosed in the initial stages, the prognosis is most often favorable. A negative outcome, even after treatment, is observed in cases where the pathology is diagnosed at late stages.
In this case, the presence of metastases in neighboring organs, tissues and outside the intestine is noted. Treatment in later stages involves eliminating symptoms and alleviating the patient's condition.
At the first stage, the five-year survival rate after surgery ranges from 90 to 100%. When a cancerous tumor is detected in the colon in the later stages of development, survival rate in the first five years after surgery ranges from 50 to 20%, depending on the characteristics of the course, the presence and number of metastases.
Acute and chronic constipation
Acute constipation is the absence of bowel movements for several days. If this condition is accompanied by abdominal pain, tension in the abdominal wall, deterioration in health, increased body temperature, nausea, the person needs urgent hospitalization.
If there are no such symptoms, it is necessary to identify the cause of fecal retention and eliminate it. In addition, you should promote the removal of feces - for this you can use cleansing enemas, mild laxatives, and foods rich in fiber.

Chronic constipation is a condition in which a person complains of infrequent bowel movements (less than three per week). Associated symptoms are a feeling of incomplete bowel movement, blockage in the anorectal area. To treat chronic constipation, it is necessary to identify and eliminate its cause, that is, the underlying disease.
Treatment
Asymptomatic dolichocolon is not considered a disease and does not require treatment. For chronic constipation, therapeutic measures restore bowel movement and improve well-being.
Treatment should be comprehensive and step-by-step. To stimulate your intestines, try to move more: do morning exercises, walk, sign up for a pool or gym.
Diet
Adjust your diet and eating habits.
Principles of nutrition
- Eat regularly. Long breaks in eating increase the risk of complications. It is no coincidence that volvulus is called “the disease of a hungry man.”
- Eat food in a calm environment, without rushing.
- Maintain drinking regime. For normal bowel function, 1.5-2 liters of fluid per day is required, including first courses, vegetables, and fruits.
- Include foods rich in dietary fiber in your diet.
- Avoid foods that are too rough. Increased peristalsis can cause intestinal obstruction.
- Eliminate foods that increase the formation of gases in the intestines. Flatulence causes abdominal pain.
- Any methods of culinary processing of products are allowed.
Grocery list
| Recommended | Not recommended |
|
|
Adjust the list depending on individual preferences and food intolerances.
Medicines
- Laxatives - treatment begins with preparations based on dietary fiber (Psyllium, wheat bran, Mucofalk). If ineffective, osmotic agents are prescribed: Macrogol (polyethylene glycol) and Duphalac (lactulose). Irritating drugs (Bisacodyl, Senade) are used to a limited extent, as they are addictive.
- Antispasmodics - reduce the tone of intestinal smooth muscles, relieve painful spasms (Papaverine hydrochloride, Duspatalin, No-shpa).
- Defoamers are drugs to combat flatulence, prescribed for bloating (Espumizan, Sab Simplex).
- Eubiotics (probiotics) are drugs for correcting the microflora of the colon, prescribed for concomitant dysbacteriosis (Linex, Helac Forte, Bifiliz).
We recommend reading:
Proctitis: symptoms and treatment methods (diet, drugs, surgery)
Physiotherapy
Physiotherapy methods stimulate intestinal motor activity.
- acupuncture;
- cutaneous and rectal electromyostimulation;
- laser therapy;
- acupuncture.
Surgery
If conservative treatment is ineffective or there is a significant deterioration in health, surgery is recommended.
Basic techniques:
- subtotal resection of the colon - removal of all parts of the colon except the lower part of the sigmoid segment;
- segmental resection of the colon - excision of a pathologically changed section;
- colectomy – removal of the entire colon.
In case of intestinal obstruction, endoscopic detorsion is performed - straightening the volvulus. If the procedure is ineffective, a laparotomy is performed, the intussusception or volvulus is removed, the knot from the loops is untangled, and the viability of the intestine is assessed. In case of necrosis, the affected area is removed.

Irritable bowel syndrome
The exact reasons why this disease develops have not been identified. It manifests itself as increased sensitivity of the intestines, including the colon, to the slightest changes in diet and acute reactions to many foods. During periods of exacerbation, patients complain of abdominal discomfort, frequent pain, bowel problems (constipation or diarrhea), a feeling of incomplete bowel movement, and straining during bowel movements. Feeling unwell, flatulence, loss of appetite, headache and fatigue are observed.
Treatment of irritable bowel syndrome consists of strictly following a suitable diet, taking medications that regulate stool, and probiotics. Physical activity and a healthy lifestyle are recommended.
Prevention measures
In order to exclude the development of cancer when the pathological process affects organ tissue, experts recommend following a number of preventive measures:
- properly . The diet should not include a large number of dishes containing animal fats. It is also necessary to eat enough foods that contain vitamins, minerals, nutrients and fiber.
- Treat diseases that are precancerous in a timely manner In order to diagnose them in the early stages, when a benign tumor has not transformed into a malignant one, you should regularly visit a doctor and undergo preventive examinations.
- Avoid the development hypotension .
- To live an active lifestyle . If you stay in one position for a long time, it is recommended to take short breaks, during which you move. Exercises in the morning and walks in the fresh air are also useful.
- Avoid constipation. They can also cause colon cancer.
- When working in hazardous conditions, use special protective equipment. They will help reduce the adverse effects of various substances on the body.
Nonspecific ulcerative colitis
It can develop in any part of the intestine, including part of the colon. The symptoms and treatment of ulcerative colitis are specific. The cause of the disease may be a genetic predisposition, microbial factor, immune system disorders, bad habits, nutritional errors, and pathologies of the intestinal wall.
With ulcerative colitis, the intestine becomes sensitive to irritating factors, which is why ulcers appear on the mucous membrane, which, however, do not penetrate beyond the submucosal layer. A characteristic sign of ulcerative colitis is frequent loose stools, up to 40 times a day. There is blood, mucus, or pus in the stool. As the disease progresses, symptoms of intoxication, dystrophy, and systemic disorders appear - the entire body suffers, and signs of ulcerative colitis are detected in the skin, mucous membranes, skeleton, and internal organs.
Treatment of the disease is individual, based on examination data. As a rule, glucocorticoids, 5-aminosalicylic acid preparations, probiotics, sorbents, and, if necessary, antibiotics and immunocorrective drugs are prescribed. Naturally, appropriate nutrition is prescribed.
The leading factors in the development of colon diseases are a sedentary lifestyle, improper diet and regimen (lack of plant fiber, predominance of protein foods and fats), excessive use of medications and bad habits.
Bowel length
The length of the human intestine constantly changes throughout life. Firstly, this is due to age. In infancy, the total length of the intestines exceeds the height of a person by 8 times, and after body growth stops - only 6 times. The intestines grow especially quickly during the transition from milk to solid foods.
Since the muscle tone of this organ is different for all people, it can vary from 3 meters to 5. It is known that all the muscles of a person relax after his death, and the intestines after death lengthen to 7 meters.
The diameter of the smallest intestine is from 2 to 4 cm, and it is called the jejunum. And at the widest point in the large intestine, its diameter is 14-17 cm.
The diameter of the organ changes along its entire length, and on an individual basis. And where one person has a thickening of the intestine, another may have a narrowing on the contrary.
Symptoms of colon pathology
You can suspect that there are problems with the colon based on the following symptoms:
- Pain. They can be aching and spasmodic. Localization of unpleasant sensations is the left and right lower abdomen, the area above and below the navel. Spasms and soreness force the patient to go to the toilet, since the act of defecation brings relief. There is usually no connection between food and the appearance of pain, with the exception of inflammatory processes in the transverse colon, which is located under the stomach and reacts with reflex contractions to its excessive filling.
- Chronic constipation. There are rare stools (less than 3 times a week), difficult bowel movements, and a feeling of incomplete bowel movement.
- Diarrhea. It bothers you constantly, or appears sporadically, alternating with constipation.
- Bloating. Occurs after eating food that does not usually cause this symptom.
- Flatulence is excessive accumulation and release of gases in the intestines.
- Streaks of blood and mucus in the stool.
Symptoms of splenic flexure syndrome.
The leading symptoms of splenic flexure syndrome are:
- Pain syndrome, which can be so sharp that it resembles an angina attack;
- The pain may spread to the left half of the chest, which is perceived as myocardial infarction;
- The pain decreases with the passage of gas;
- Defecation also improves the patient's condition;
- The patient notes a feeling of fullness in the stomach;
- Possible stool disorders: diarrhea or constipation.
Considering that the clinical picture of splenic flexure syndrome can masquerade as other diseases, doctors always need to be wary of this pathology. Palpation reveals pain in the area of the splenic flexure and tympanitis on percussion. Sometimes, even purely externally, swelling of a given area is determined.
The specialist prescribes a survey X-ray of the abdominal cavity and an ultrasound, during which an accumulation of gases under the left hypochondrium becomes visible. Considering that the clinical picture may be similar to a heart attack or angina, it is imperative that such patients be given an ECG to rule out heart disease.
Colon diseases
Colon diseases are divided into the following categories:
- congenital (Hirschsprung's disease and developmental defects - duplication, narrowing, fusion of part of the intestine);
- acquired (all diseases of the colon that occur throughout life);
- inflammatory (ulcerative colitis, Crohn's disease, infectious colitis);
- non-inflammatory (polyposis, diverticulosis, dyskinesia);
- precancerous (Crohn's disease, ulcerative colitis, familial polyposis);
- malignant (colon cancer).
Nonspecific ulcerative colitis
Nonspecific ulcerative colitis is a chronic inflammation of the colon, which manifests itself as ulcers and areas of necrosis that do not extend beyond the mucous membrane. The exact causes of this disease are unknown, but the factors that provoke the development of ulcerative inflammation have been identified:
- genetic predisposition;
- imbalance of intestinal microflora;
- food allergies;
- stress.
Mostly young people suffer from ulcerative colitis. Characteristic symptoms of the disease:
Crohn's disease
Crohn's disease is an inflammatory process that spreads to all parts of the intestinal tube and affects all its layers (mucosal, muscular, serous), leading to the formation of ulcers and scar changes in the wall of the colon. Possible causes of this disease include:
- autoimmune disorders;
- genetic mutations;
- infectious factors.
Tumor in the splenic flexure of the colon. Stages and forms of the disease.
Oncology of the flexure of the spleen most often occurs in people aged 55 to 75 years, in the same percentage in both men and women. Tumors affect the bends of the colon, since fecal stagnation most often occurs in these places.
The splenic angle in the colon is the right bend of the colon, the place where the transverse colon passes into the descending colon. The bend forms an acute angle, which is fixed by the diaphragmatic intestinal ligament.
The place of formation of carcinoma is considered to be the walls of the colon, namely in its mucosa. Lack of treatment threatens to infect all layers of the wall and may extend beyond its limits. Cancerous tumors can spread to adjacent organs and tissues. Metastasis can only appear in the last stages of cancer. Metastasis can occur by lymphogenous (moves through regional lymph nodes), implantation (through serous membranes bordering the tumor site), hematogenous (through blood vessels). Most often, metastases affect the spleen, liver, lungs, and less often - bones and brain.
With the development of a tumor as a result of polycystic disease, the appearance of multiple foci of localization (double, triple) is possible.
Based on morphological changes, cancer tumors are divided into forms:
- exophytic – grows into the intestinal lumen;
- infectious endophytic - grows deep into the wall and does not have sharply defined boundaries;
- mixed mesophytic - combines both previous forms;
According to development, cancer of the splenic flexure is divided into stages:
- the first is a small tumor, localized in the submucosal layer or mucous membrane. The boundaries are clearly visible. There are no metastases;
- the second, a) is a larger tumor. It occupies no more than half of the intestinal lumen and does not extend beyond its limits. There is no metastasis; second, b) – the tumor is increasing, there may be single metastases;
- third, a) - a malignant formation occupies more than half of the lumen and can grow into the walls and adjacent peritoneum. There are no metastases; third, b) – the tumor affects organs near the localization of the lesion. Multiple metastases appear;
- the fourth is a large-scale formation that spreads to neighboring tissues and organs. Multiple metastases are typical.
It is very important to identify the disease in the initial stages. Since the fourth stage is almost untreatable, the risk of death increases significantly.
Splenic flexure syndrome is a collective term consisting of several symptoms that develop as a result of the accumulation of gases in the left hypochondrium.
As a result of the accumulation of gases, stretching of the splenic flexure of the large intestine occurs, which gives quite characteristic clinical symptoms.
The reason for the development of this symptom may be:
- Irritable bowel syndrome;
- Dysbacteriosis;
- Distension of the stomach with air, both during eating and during medical procedures;
- Intestinal obstruction;
- Poisoning;
- Upper abdominal adhesions;
- Diseases of the pelvic organs;
- Poor posture;
- Tight clothing that compresses the abdominal organs.
Considering the number of reasons that can lead to splenic flexure syndrome, it should be noted that the true syndrome is noted only with visual confirmation of the presence of gases under the left hypochondrium.
Diagnostics
A proctologist is involved in identifying and treating pathologies of the colon. The examination plan for patients with symptoms of diseases of this organ includes:
- Colonoscopy. Endoscopic examination of the large intestine is carried out through the anus. The endoscopist examines the mucous membrane of the organ in real time and takes material from suspicious areas for histological analysis.
- Irrigoscopy. This method of X-ray diagnostics with contrast allows you to clearly visualize defects of the intestinal wall, identify neoplasms and defects of the colon.
- Histological examination. Studying the morphology of a tissue sample taken from the intestine is the most reliable way to diagnose cancer, ulcerative colitis, Crohn's and Hirschsprung's disease.
- Coprogram. Examination of stool smears under a microscope is carried out to identify signs and possible causes of the inflammatory process in the small intestine and to assess the evacuation function of the intestinal tract.
- Culture of stool for microflora. If the infectious nature of the inflammatory process is suspected, this analysis makes it possible to make an accurate diagnosis and isolate the pathogen, which is extremely important for selecting antibacterial treatment.
Classification
The widespread nature of the growth of malignant neoplasia allows us to divide them into three clinical and anatomical forms.
- Exophytic tumors with characteristic growth into the lumen of the affected intestine and localization in its right half. There are nodular, polyp-like, villous-papillary.
- Endophytic neoplasms that do not have clear contours and develop in the thickness of the intestinal wall. Most often located in the left half of the colon. There are ulcerative, circular-structuring, infiltrating.
- Mixed (combined) neoplasia.
According to the international morphological classification, taking into account the cellular structure, colon cancer is divided into the following categories.
| Histological form of carcinoma | Occurrence |
| Adenocarcinoma (highly, moderately, poorly differentiated) | 90-95 |
| Mucinous | 10 |
| Signet ring cell | 4 |
| Squamous cell | Less than 1 |
| Adengosquamous | -“- |
| Undifferentiated | -“- |
| Unclassifiable | -“- |
Recommendations for prevention and therapy
Each of the listed colon diseases has its own treatment tactics. For ulcerative colitis and Crohn's disease, patients are prescribed salicylates, hormones and immunosuppressants. If intestinal inflammation is infectious in nature, antibacterial therapy is recommended. With dyskinesia of the colon, the patient is referred for treatment to a neurologist or psychotherapist. Severe diverticulosis, polyposis, colon anomalies, Hirschsprung's disease are indications for surgical treatment. For a cancerous tumor, complex treatment is carried out taking into account the stage of the malignant process.
To minimize the risk of developing colon diseases, it is necessary to include plant foods in your diet, avoid unhealthy fats, take timely measures to eliminate constipation and be attentive to your health.
If the symptoms described in the article appear, you should immediately contact a proctologist. After 50 years, it is advisable to visit this specialist annually and undergo regular colonoscopy, even if there are no complaints about bowel function.
Complications
According to statistics, dolichocolon is the cause of acute intestinal obstruction in 8% of cases. The long colon has additional loops and pathological mobility.
Mechanisms of obstruction:
- formation of nodes from intestinal loops;
- intussusception - the introduction of one section of the intestine into another;
- volvulus is a rotation of a loop of intestine around the axis of the mesenteric vessels.
We recommend reading:
Main symptoms of appendicitis
The blood supply to the affected area is disrupted. When seeking medical help late, intestinal necrosis and peritonitis develop, which often leads to death.
What diseases are the intestines susceptible to?
The intestine is a very important organ for life in the human body. Like any organ, it is susceptible to various diseases, any of which leads not only to painful sensations in the abdominal cavity, but also affects the general well-being of a person and the condition of the entire body. For example, with severe diarrhea, a person rapidly loses body weight and strength. Without treatment for this pathology, the patient may simply die from exhaustion.
The type of disease determines where the pain occurs. Everyone knows that when the appendix is inflamed, pain most often occurs in the lower right side of the abdomen.
The main intestinal diseases include pathologies such as ulcerative or infectious colitis, duodinitis, Crohn's disease, intestinal obstruction, enterocolitis, enteritis and tuberculosis.
There are a number of other pathologies, but they occur much less frequently - intestinal stenosis, duodenal hypertension, irritable bowel syndrome.
How the intestines work
The human intestine is represented by two sections - thin (longer) and thick (short but wide). The blood supply to the intestine in its different parts, as well as its functions, differ greatly. There is a special valve between the sections of the intestine that prevents food from going back up from the colon. Food always moves in one direction - through the duodenum down to the rectum and further to the anus.
The muscle tissue of the intestinal walls is a structure of longitudinal and transverse fibers. They move without signals from the central nervous system, that is, a person does not control his peristalsis. Impulses of movement through the intestines are transmitted along nerve fibers that widely intertwine the entire intestine.
It is known where the intestines are located - in the abdominal cavity, but it does not just hang there - the intestines are attached to the walls of the peritoneum by special ligaments.
The human intestine secretes up to 3 liters of special juice per day, saturated with various alkalis. This feature allows it to digest food passing through the organ.
All intestines have a similar structure - they are covered from the inside by the mucous membrane, underneath it is the submucosa, then the muscles and the serous layer covers them.
The small intestine is represented by several sections that have their own functions. For example, in the duodenum there is a special duct through which bile from the liver enters it, finally digesting the food that has passed through the stomach.
The jejunum, immediately following the duodenum, breaks down peptins and disacchorides into elementary particles - amino acids and monosaccharides.
The next intestine, the ileum, absorbs bile acids and cyanocobalamin.
The large intestine is also a complex structure. It includes the descending and ascending colon, sigmoid colon, rectum and caecum, ending in the appendix.
The main job of the large intestine is to remove fluid from the chyme by absorbing it through the walls and forming feces.
It ends thick with receptors and anal sphincters located in it. When pressure is applied to fecal receptors, the brain receives a signal that the rectum is full and gives the command to start defecation. After this, the sphincters relax and release feces.
Diagnosis of intestinal diseases
Diagnosing bowel disease is very difficult. To do this, the doctor must collect as much information as possible about the patient’s condition, as well as about the processes occurring in his intestines.
First of all, a detailed medical history is collected. The doctor asks the patient about the symptoms he is experiencing. About what kind of stool the patient has, how often he experiences the urge to defecate, and most importantly, what type of pain the person has - its strength, location, duration.
Information about the presence of rumbling in the stomach and flatulence, that is, the release of gases, is important. The doctor pays attention to the patient's appearance. If he has dry and thin skin, weak brittle hair, pale face and general weakness, this, coupled with information obtained from the anamnesis, can help diagnose various diseases of the small intestine.
Using the palpation method, the specialist determines the exact location of the pain, and also determines the shape and size of the colon. Using this seemingly simple method, for example, inflammation of the appendix is diagnosed, since other methods in this case are not very informative.
Instrumental diagnostics are also widely used. After all, what is the intestines? This is an organ inside the abdominal cavity, which means it can be studied using ultrasound or a more informative MRI.