Causes of small intestine cancer
Malignant cells differ from normal cells of the body in their ability to undergo uncontrolled and endless division (in healthy cells the number of possible divisions is limited), loss of the ability to die naturally, and the possibility of spreading to neighboring tissues and organs and their destruction.
In the body of any person, mutations constantly occur that cause the appearance of malignant cells. But usually the immune system quickly detects them and destroys them before the tumor begins to grow. However, if, under the influence of some factors, too many altered cells are formed or the immune system does not recognize them in time, a malignant tumor appears.
Doctors do not have an exact list of the causes of small intestinal cancer. The only known risk factors that increase the likelihood of its occurrence are:
- Crohn's disease. This is a chronic inflammation of the small intestine. Under the influence of a long-term inflammatory process, the normal ability of the mucous membrane to recover is disrupted and its cells can become malignant.
- Celiac disease. With this disease, the body produces antibodies to the proteins of cereal plants - gluten. Immune compounds settle on the lining of the small intestine, causing inflammation. Chronic inflammation impairs the ability for normal mucosal regeneration.
- Familial adenomatous polyposis. This is a hereditary disease in which, due to an error in genes, many polyps form on the mucous membrane. Polyps themselves are benign formations, but over time they degenerate into malignant ones.
Symptoms of small intestine cancer
Quite often, small intestinal cancer is asymptomatic until the tumor blocks the intestinal lumen or metastases appear in other organs, signs of damage to which will become the first manifestations of the disease.
Even if symptoms of small intestinal cancer do appear, they are often vague and do not specifically indicate malignant lesions:
The first manifestations of small intestine cancer are usually nonspecific Photo: shutterstock.com
- an admixture of blood in the stool or black stool (the closer to the stomach the bleeding site, the more the blood iron is oxidized under the action of digestive enzymes, becoming black);
- diarrhea;
- bloating;
- stomach ache;
- anemia.
The so-called “minor symptoms” of intestinal cancer - signs of tumor intoxication - appear already at a late stage of the process:
- causeless weight loss;
- long-lasting temperature of about 37 degrees for no apparent reason;
- weakness, sweating;
- causeless apathy;
- drowsiness or, conversely, insomnia.
Such manifestations individually can be symptoms of a sluggish infection, chronic fatigue syndrome, or a reaction to stress, so they are rarely paid attention to. Even after consulting a doctor, the patient often does not receive proper care.
If the neoplasm blocks the intestinal lumen, symptoms of so-called “high” intestinal obstruction begin to appear:
- fast saturation;
- feeling of heaviness and fullness in the stomach;
- vomiting of food eaten the day before or several days ago; relief comes after vomiting;
- constipation, impaired passage of gases.
If the tumor begins to disintegrate, severe intestinal bleeding may occur. The stool becomes profuse, cherry-colored, and the patient shows signs of severe blood loss (pallor, rapid heartbeat, sharp decrease in blood pressure, weakness). Also, when the tumor disintegrates, perforation of the intestine and peritonitis is possible.
When metastases occur, signs of damage to other organs come to the fore: jaundice, cough, bone pain and pathological fractures, etc.
Diagnosis of small intestine cancer
Diagnostic options are relatively limited as there are few methods available to visualize the condition of the small intestine. Until now, this section of the gastrointestinal tract is considered a “white spot in gastroenterology.” The doctor may order the following tests:

- X-ray of the abdominal cavity with contrast - allows you to visualize the lumen of the small intestine, see narrowings, obstacles in the path of contrast;
- gastroduodenoscopy - prescribed for suspected duodenal cancer; other parts of the small intestine are not available for endoscopy;
- Ultrasound of the abdominal cavity is not very informative for studying the condition of the intestines, but allows you to visualize neighboring organs where metastasis is possible;
- computed tomography of the abdominal cavity with contrast - allows you to assess the condition of the small intestine - lumen, wall thickness, and so on;
- MRI of the abdominal cavity with contrast;
- PET-CT is one of the most accurate, but extremely expensive methods for detecting malignant neoplasms and metastases;
- diagnostic laparoscopy - endoscopic examination of the abdominal cavity, if there is a suspicion that the cancer has spread to the outer wall of the intestine, peritoneum, omentum;
- exploratory laparotomy - if all other diagnostic options have been exhausted, as a last resort, doctors may suggest open surgery to evaluate the condition of the abdominal cavity.
To determine the general condition, the patient will be prescribed a general and biochemical blood test. If metastases to other organs are suspected, tests are performed to determine how intact the functions of these organs are.
Ileum: functions and main diseases
The ileum is the lower part of the small intestine, located in front of the cecum.
The ileum is located in the right iliac fossa (right lower abdomen) and is separated from the cecum by the bauhinian valve (ileocecal valve). A small part of it may occupy the umbilical region, epigastrium, and pelvic cavity.
The upper loops of the intestine are located vertically, the lower loops are horizontal. The ileum is displaced to the right of the midline.
Often the jejunum and ileum are considered together because they are completely covered by peritoneum and have their own mesentery. With the help of the mesentery, both sections of the intestine are fixed to the posterior abdominal wall.
The mesentery itself has two layers of peritoneum, between which pass nerves and vessels that provide nutrition to the intestine, as well as fatty tissue. The ileum is fixed to the free edge of the mesentery.
The second edge of the mesentery (root) has a length of 12 to 16 cm and is attached to the posterior abdominal wall obliquely, in the direction from top to bottom and from left to right. This corresponds to the left edge of the second lumbar vertebral body and up to the right sacroiliac joint.
The line along which the mesentery is attached is not constant; it can be at different angles relative to the midline of the abdomen (from 12 to 63˚). Its width also changes along its entire length: it increases from the duodenal-jejunal flexure and becomes shorter towards the ileocecal angle.
In rare cases, the ileum has a residual part of the embryonic bile duct on its wall. It is called Meckel's diverticulum, its length does not exceed 7 cm, its diameter is approximately equal to the diameter of the ileum and extends from the side opposite to the mesenteric attachment.
Location of organs in relation to the ileum.
Above and in front of the ileum lie the loops of the transverse colon, the mesentery and the greater omentum. Posterior to the loops of the small intestine is the parietal peritoneum and organs of the retroperitoneal space. The lower loops of the ileum lie above or between the organs of the pelvic cavity.
- 1 Building
- 2 Functions
- 3 Main diseases
Structure
The structure of the walls of the ileum and jejunum is similar. The inner layer is the mucous membrane, abundantly covered with numerous villi. They are formed by the mucous membrane itself and rise by 1 mm. The villi are covered with columnar epithelium; in the center of each villi there is a lymphatic sinus and blood vessels (capillaries). There are fewer villi in the ileum than in the jejunum.
Each villi is involved in the process of nutrient absorption. Monosaccharides and amino acids are absorbed through venous vessels, and fats through lymphatic vessels. The surface of the ileal mucosa has an uneven surface due to the presence of crypts, circular folds and villi.
These formations increase the total surface of the intestinal mucosa, which is necessary for the absorption of digested food.
Intestinal villi are leaf- or finger-shaped and protrude into the intestinal lumen. The number of villi in the ileum ranges from 18 to 31 per 1 square mm, they are slightly thinner than the villi of the duodenum.
Intestinal crypts, or Lieberkühn's glands, are presented in the form of depressions in the mucous membrane and have the shape of tubes. The excretory openings of the glands open between the villi.
The mucous membrane and submucosa together form circular folds of the intestine. The mucosal epithelium is single-layered, prismatic, bordered. In addition, the mucous membrane has its own submucosa and the following muscle layer.
The muscular layer of the ileum is represented by two layers of smooth muscle fibers: the outer, or longitudinal, and the inner, or circular, which is more powerful.
Between both layers is loose fibrous connective tissue, where the myenteric nerve plexuses and blood vessels are located. The thickness of this layer gradually decreases towards the terminal ileum.
The muscularis mucosa performs the function of pushing and mixing the chyme.
The outer lining of the ileum is serous. The ileum is covered with serosa on all sides.
Functions
The ileum performs a number of functions, the main ones being: the secretion of enzymes, the digestion of food and the absorption of nutrients, salts and minerals.
Intestinal juice is secreted under the influence of mechanical and chemical irritation of the intestinal walls by chyme. Up to 2.5 liters are produced per day. The juice reaction is alkaline.
The dense part of the intestinal juice consists of lumps of epithelial cells, which produce enzymes and gradually accumulate them. At the necessary moment, the cells are rejected into the intestinal lumen and destroyed, providing cavity digestion.
Each epithelial cell on its surface has a microvilli - a kind of outgrowth on which digestive enzymes are fixed. This is another level of digestion in the ileum, called parietal (membrane).
At this stage, food is hydrolyzed and absorbed.
Intestinal juice contains 22 enzymes. The main one is enterokinase. It activates pancreatic trypsinogen. In addition, the juice contains lipase, amylase, peptidase, sucrase and alkaline phosphatase.
The advancement of chyme into the next sections of the digestive tract is carried out by contraction of the fibers of the muscular layer of the intestine. The main types of motion are pendulum-like and peristaltic waves. The first group of contractions mixes the chyme. Vermiform, or peristaltic, waves propel food into the distal intestine.
Both types of digestion exist interconnected. During cavity digestion, complex substances are hydrolyzed to intermediate substances. Next, intermediate products are broken down using membrane digestion, and the absorption process begins, which occurs through an increase in intraintestinal pressure, small intestinal motility, and villi movement.
Treatment of small intestine cancer
Surgery
Surgery is considered the main treatment for small intestinal cancer. If it is technically possible and the tumor has not grown into neighboring organs, the section of intestine with the tumor is removed at once, after which intestinal patency is restored. For advanced cancer, surgery may be performed to restore intestinal patency.
Chemotherapy
The doctor prescribes drugs that destroy actively dividing cells. Since in case of cancer it is the malignant cells that divide the fastest in the body, chemotherapy drugs act primarily on them. But since, in addition to cancer, cells of mucous membranes, hematopoietic organs, and hair follicles divide relatively quickly, the effect of chemotherapy drugs is not as narrowly targeted as we would like, and side effects are not uncommon. Chemotherapy for small intestinal cancer is used as a palliative method - prolonging life, but not capable of curing.
Radiation therapy
The area of the malignant neoplasm is irradiated with ionizing radiation, which damages the DNA of the cells, after which they die. Usually prescribed for metastatic small intestinal cancer to the area of metastases as a palliative method.
What it is
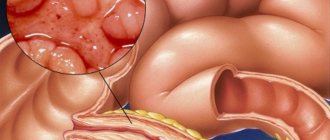
A key feature of a malignant neoplasm is its ability to spread metastases. The concept is translated from Greek as “otherwise standing.” Metastases are secondary foci of development of most malignant neoplasms.
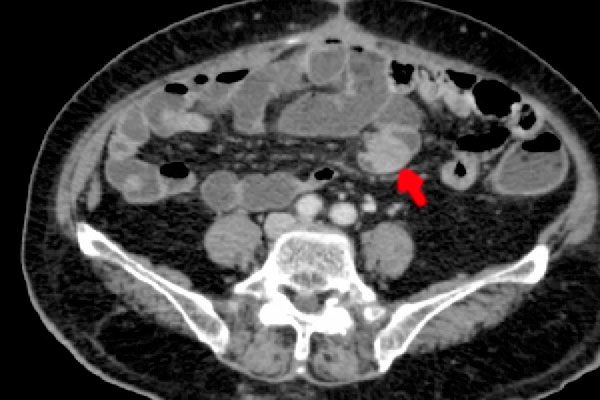
Photo: metastasis in the intestine
Modern scientists have come to the conclusion that metastases begin to develop immediately after the appearance of the primary tumor. Its particles constantly break off and move throughout the body in two main ways:
- lymphogenous;
- hematogenous.
Malignant particles that have broken away from the maternal lesion may remain inactive for a long time. Scientists cannot determine the reason why the mechanism of their rapid development is triggered.
It is possible that in the early stages of the disease the development of metastases is prevented by the primary tumor. Another reason may be the person’s immunity, which destroys some cancer cells, including those in the intestines.
With the development of a secondary tumor, the number of cells in it increases. Capillary networks are formed around the tumor, the task of which is to provide the tumor with nutrients. Because of this, healthy body tissues do not receive enough nutrients.
In terms of time, secondary neoplasms can appear after 1-2 years, or can be detected many years after surgery. Typically, the appearance of metastases is associated with the fourth stage of the oncological process.
Secondary neoplasms are usually called after the primary focus. For example, if cancer appeared in the kidney and spread to the intestines, then the pathology in it will be called “metastatic kidney cancer.”
At the genetic level, secondary formations may be similar to the maternal tumor. There are many examples where metastases were different from the primary tumor. This phenomenon is known as heterogeneity.
Metastases are dangerous because they disrupt the functioning of all important organs for the patient’s life. Death occurs precisely due to metastasis of the underlying cancer. Patients with metastases often require ongoing pain relief.
In this video, the process of metastasis is visualized using graphics: